Abstract
Xanafide, a DNA-intercalating agent and topoisomerase II inhibitor, has previously demonstrated comparable cytotoxicity to the parent drug amonafide (NSC 308847). The current study was conducted to investigate further the anti-proliferative effects of xanafide in human breast cancer cell lines, in vitro and in vivo. The in vitro activity of xanafide against MCF-7, MDA-MB-231, SKBR-3 and T47D cell lines was compared to that of paclitaxel, docetaxel, gemcitabine, vinorelbine and doxorubicin. In MCF-7, xanafide demonstrated comparable total growth inhibition (TGI) concentrations to the taxanes and lower TGI values than gemcitabine, vinorelbine and doxorubicin. MCF-7 (oestrogen receptor (ER)+/p53 wild-type) was the most sensitive cell line to xanafide. MDA-MB-231 and SKBR-3 exhibited similar sensitivity to xanafide. T47 D (ER+/p53 mutated), showed no response to this agent. The in vivo activity of xanafide was further compared to that of docetaxel in MCF-7 and MDA-MB-231 cell lines using the hollow fibre assay. Xanafide was slightly more potent than docetaxel, at its highest dose in MCF-7 cell line, whereas docetaxel was more effective than xanafide in MDA-MB-231 cell line. Our results show that there is no relationship between sensitivity of these cell lines to xanafide and cellular levels of both isoforms of topoisomerase II and suggest that ER and p53 status and their crosstalk may predict the responsiveness or resistance of breast cancer patients to xanafide.
Similar content being viewed by others
Main
Breast cancer is the most common malignancy affecting women in the Western world. Systemic chemotherapy is indicated for women with metastatic breast cancer (MBC) that is oestrogen/progesterone-negative or unresponsive to hormonal therapy, or rapidly progressing and life-threatening (Hortobagyi and Piccart-Gebhart, 1996). Several single-agent chemotherapeutic options have been shown to be effective as first- or second-line therapy in the management of MBC with the taxanes and anthracyclines being among the most active drugs (Pronzato and Rondini, 2006).
The taxanes, paclitaxel and docetaxel, bind to, and stabilise microtubules, causing cell-cycle arrest and apoptosis (Schiff et al, 1979). The overall response rates achieved in MBC patients were 29–63 and 47–65%, with paclitaxel and docetaxel, respectively (Montero et al, 2005). However, side effects such as hypersensitivity reactions, myelosuppression and neuropathy were observed with the taxanes, although docetaxel causes less neuropathy and more myelotoxicity (Ghersi et al, 2005).
Anthracyclines are active agents in primary adjuvant and palliative treatment of breast cancer (Kroger et al, 1999). Doxorubicin intercalates among DNA base pairs resulting in conformational changes in DNA structure and changes in the activity of topoisomerase. In MBC, response rates to single doxorubicin treatment range from 52% in previously untreated patients to 28% in patients previously exposed to an alkylating agent (Esteva et al, 2001). In patients who failed to respond to anthracycline and taxanes treatment, administration of capecitabine, gemcitabine or vinorelbine has been shown to result in overall response rates of 20–25% (Livingston et al, 1997; Blum et al, 1999; Valerio et al, 2001). Gemcitabine, an antimetabolite pyrimidine analogue, and vinorelbine, which inhibits microtubule polymerisation, have been widely investigated in the treatment of MBC (Martin et al, 2007).
In view of previous studies, in clinical practice, the potential therapeutic impact of standard chemo-agents for breast cancer is often limited due to intrinsic and/or acquired drug resistance in addition to drug-related toxicity. Therefore, balancing efficacy and toxicity is a major challenge, and the optimal choice of chemotherapy must be driven by patient and disease characteristics such as menopausal status, oestrogen and progesterone receptor status, Her-2 neu expression (Gralow, 2005), and tumour characteristics such as p53 gene involved in tumour response to therapy (Vogelstein et al, 2000).
Given the current status of the breast cancer treatment and to further improve the clinical outcome in these patients, new treatment approaches are needed.
Naphthalimides are DNA-intercalating agents that bind to DNA by insertion between the base pairs of the double helix. Intercalation causes the base pairs to separate vertically, thereby distorting the sugar-phosphate backbone and changing the degree of rotation between successive base pairs. Naphthalimides were designed by combining structural components of several antitumour compounds into a small molecule and have shown high antitumour activity upon a variety of murine and human tumour cells (Brana and Ramos, 2001). One of these compounds, amonafide (Sami et al, 1993) has been verified to exert ATP-independent topo II-mediated DNA cleavage (Andersson et al, 1987; Hsiang et al, 1989; Dorr et al, 2001). Furthermore, this agent is not affected by the multidrug resistance phenomenon and is not an efflux pump substrate (Dorr et al, 2001).
In previous clinical studies, amonafide demonstrated activity for the treatment of MBC (Costanza et al, 1995). However, it is metabolised to an active but myelosuppressive metabolite, the N-acetyl amonafide. A population study in women with breast cancer established that wide variation in the major side-effect of neutropenia was related to inter-individual patient differences in N-acetylating activity. Importantly, at the same prescribed dose, slow NAT2 acetylators were believed to be underdosed as reflected by minimal response rate and lack of grade 3 myelosuppression while rapid acetylators had greater haematologic toxicity attributed to slower clearance of the parent amonafide (Ratain et al, 1991, 1993). These data, and that from other studies in a variety of major tumour types, led to the conclusion that amonafide should not be considered for further clinical development.
Xanafide (amonafide L-malate), a novel salt formulation of amonafide, has been developed. Preliminary pharmacological and chemical equivalence studies demonstrated that xanafide had comparable pharmacokinetics and toxicity in vitro and in vivo, while having superior solubility, stability and compressibility than the parent drug, amonafide (personal communication). Individualising the dose of xanafide as a function of NAT2 phenotype may optimise patient safety and therapeutic benefit. Xanafide has recently received the FDA Orphan Drug Designation for the treatment of acute myeloid leukaemia (AML) and has now entered phase II clinical trials in patients with secondary AML.
The present study is the first one to report preclinical evaluation of xanafide. Our aim was to compare xanafide activity to standard breast cancer agents (paclitaxel, docetaxel, vinorelbine, gemcitabine and doxorubicin) in a panel of four breast cancer cell lines: MCF-7, MDA-MB-231, SKBR-3 and T47D, in vitro, and against paclitaxel in the first two cell lines, in vivo. This panel included oestrogen receptor (ER)-positive and ER-negative cell lines, since it has been shown that oestrogen can enhance the effects of topoisomerase II inhibitors in ER-responsive breast cell lines (Epstein and Smith, 1988).
Materials and methods
Cell lines
MCF-7, MDA-MB-231, SKBR-3 and T47D were obtained from the American Type Culture Collection (ATCC) (Rockville, MD, USA). Cell lines were grown in RPMI-1640 medium (Invitrogen, Gaithersburg, MD, USA), supplemented with 10% fetal bovine serum, 2 mM L-glutamine at 37°C in a humidified atmosphere containing 5% CO2.
Chemicals and compounds
All general chemicals were purchased from Sigma Chemical Co. (St Louis, MO, USA) unless otherwise specified. Xanafide was kindly provided by Xanthus Life Sciences. Paclitaxel, docetaxel, doxorubicin, vinorelbine and gemcitabine are commercially available. Before in vitro use, a 1 mM stock solution of each agent was prepared by dilution in culture media. Polyvinylidene fluoride hollow fibres (500 000 Da molecular weight cutoff, 1.0 mm ID) were purchased from Spectrum Medical Industries (Luguan Hills, CA, USA).
Animals
Athymic NCr nu/nu mice, 5–6 weeks of age were purchased from Taconic (Germantown, NY, USA). All studies involving these animals were conducted in accordance with National Cancer Institute (NCI) protocol and the McGill University Animal Care and Ethics guidelines.
Cytotoxicity assay
Cytotoxicity studies were performed using the sulphorhodamine B assay (Skehan et al, 1990). Cytotoxicity of each drug was evaluated by the GI50 and TGI values, representing the 50% growth inhibition and total growth inhibition, respectively, compared to non-treated control (C) and a control at time of addition of increasing drug concentrations (Tz). On day 1, MCF-7 & SKBR-3 (5000 cells) and MDA-MB-231 & T47D (20 000 cells) were seeded into 96-well plates in a volume of 100 μl per well. On day 2, one plate of each cell line was fixed in situ with trichloroacetic acid (TCA) to establish the cell population at time of drug addition (Tz). An aliquot of 100 μl of serial dilutions of the different agents was added to the appropriate well, resulting in a series of final concentrations ranging from 0.1 nM to 100 μ M. After 48 h of drug exposure, the medium in control and drug-containing wells was removed. Cells were washed with cold phosphate-buffered saline (PBS) and then precipitated with 50 μl ice-cold 50% TCA and fixed for 60 min at 4°. The supernatant was discarded, and cells were washed five times with tap water and air-dried. Fixed cells were then dyed with 50 μl of 0.4% sulphorhodamine B in 1% acetic acid solution and the plates were incubated for 10 min at room temperature. Unbound dye was removed by washing with 1% acetic acid and the plates were air-dried. Sulphorhodamine B was dissolved in 150 μl of 10 mM Tris-buffer (pH 10.5) and 540 nm optical density was measured in a Labsystems Multiskan® Multisoft apparatus. Percent net growth was calculated using the seven absorbance measurements (time zero, (Tz), growth control, (C), plus the test growth at the different drug concentration levels (Ti)) as follows: ((Ti–Tz)/(C–Tz)) × 100 for concentrations for which Ti>/=Tz and ((Ti–Tz)/Tz) × 100 for concentrations for which Ti<Tz. The results are expressed as the mean of three independent experiments±s.e.m.
Evaluation of xanafide antitumour activity using the in vivo hollow fibre assay
The in vivo hollow fibre test was performed using the original NCI protocol (Hollingshead et al, 1995). Confluent monolayers of MCF-7 and MDA-MB-231 cells were harvested, collected by centrifugation and resuspended in conditioned medium. In preliminary NCI studies, cell growth was assessed with fibres containing various cell densities. As a result, cell densities of 2.5 × 106 and 5 × 106 cells ml−1 were found to be suitable for drug studies with MCF-7 and MDA-MB-231 cell lines, respectively. Fibres filled with cells at the respective densities were incubated in 6-well plates overnight at 37°C in a 5% CO2 atmosphere. Female athymic NCr nu/nu mice at 5–6 weeks of age were obtained from Taconic. Each mouse hosted up to six fibres, which were cultured in two physiological compartments. For intraperitoneal (i.p.) implants, a small incision was made through the skin and musculature of the dorsal abdominal wall, the fibre samples were inserted into the peritoneal cavity in a craniocaudal direction and the incision was closed with skin staples. For subcutaneous (s.c.) implants, a small skin incision was made at the nape of the neck to allow insertion of an 11-gauge tumour implant trocar. The trocar, containing the hollow fibre samples, was inserted caudally through the s.c. tissues and fibres were deposited during withdrawal of the trocar. The incision was closed with a skin staple.
Mice were randomised into three groups: saline control group (n=6), xanafide and docetaxel treated groups (n=3 for each group). Xanafide was dosed at the maximum tolerated dose 30 mg kg−1, on the basis of reported in vivo studies with amonafide (Dorr et al, 2001), and docetaxel at 5 and 12.5 mg kg−1 based on previous paclitaxel NCI tested doses (Hollingshead M, unpublished data). Both agents, in PBS were given once daily by i.p. injection from day 3–7 after implantation as reported previously (Hollingshead et al, 1995). Animals were monitored daily and clinical signs and body weights were recorded daily.
On day 8, mice were killed and fibres were retrieved. The fibres were placed into 6-well plates, with each well containing 2 ml of fresh, prewarmed culture medium and allowed to equilibrate for 30 min at 37°C. To define the viable cell mass contained within the intact hollow fibres, a 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) dye conversion assay was used. Briefly, 1 ml of prewarmed culture medium containing 1 mg MTT ml−1 was added to each dish. After incubating at 37°C for 4 h, the culture medium was aspirated and the samples were washed twice with normal saline containing 2.5% protamine sulphate solution followed by overnight incubation at 4°C. To assess the optical density of the samples, the fibres were transferred to 24-well plates, cut in half and allowed to dry overnight. The formazan was extracted from each sample with dimethylsulphoxide (250 μl well−1) for 4 h at room temperature on a rotation platform. Aliquots (150 μl) of extracted MTT formazan were transferred to individual wells of 96-well plates and assessed for optical density at a wavelength of 540 nm. Results are expressed as % growth inhibition compared to control±s.d.
Statistical analysis
The comparisons between the untreated and treated groups were analyzed using the Student's t-test. Two-sided P-values less than 0.05 were considered statistically significant.
Results
In vitro antiproliferative activity of xanafide in human breast cancer cells
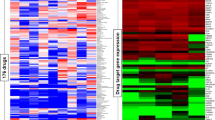
A panel of four human breast cancer cell lines: MCF-7, MDA-MB-231, SKBR-3 and T47D was used in this study. Their molecular characteristics are listed in Table 1. Using the SRB assay, the cytotoxicity profile of xanafide was compared with those of five anticancer drugs widely used in the clinic: paclitaxel, docetaxel, doxorubicin, gemcitabine and vinorelbine. The results were expressed as GI50 and TGI values and summarised in Table 2.
After 48 h exposure time, xanafide demonstrated a steep response curve in the four breast cell lines tested (Figure 1A–D). Xanafide inhibited the growth of the ER-positive MCF-7 and T47D cells in a concentration-dependent manner, with an average GI50 value of 5 and 20 μ M, respectively. Xanafide also inhibited the growth of the ER-negative SKBR-3 and MDA-MB-231 cells in a concentration-dependent manner, with an average GI50 value of 6 and 10 μ M, respectively (Table 2). T47 D was the less sensitive to the antiproliferative effect of xanafide (Figure 1D). Notably, no total growth inhibition of T47D was obtained which could, in part, be due to the long doubling time of this cell line (45.5 h).
In vitro cytotoxicity of xanafide in breast cell lines in comparison with common drugs. (A) MCF-7, (B) MDA-MB-231, (C) SKBR-3, (D) T47D. Xanafide (•), vinorelbine (▴), gemcitabine (▪), doxorubicin (○), paclitaxel (▵) and docetaxel (□). Cells were exposed to the different drugs for 48 h. % Net growth was determined with the SRB assay as described in Materials and Methods. The results are the average of three separate experiments±s.e.m.
To better visualise the differences in the cytotoxicity to achieve complete cell growth inhibition for all the agents, TGI concentrations (resulting in total growth inhibition) were expressed. At doses higher than the TGIs, net cell killing was observed in the four breast cell lines tested: MCF-7, MDA-MB-231, SKBR-3 and T47D (Table 2).
In MCF-7 cell line, xanafide exhibited a 1.7–2.2-fold lower TGI concentration than those of docetaxel and paclitaxel, respectively. Vinorelbine and doxorubicin induced similar effects and their TGI concentrations were 10-fold higher than that of xanafide. No total growth inhibition was achieved with gemcitabine (Table 2).
In MDA-MB-231 cell line, doxorubicin induced total growth inhibition at the lowest concentrations: 15 μ M, whereas paclitaxel, docetaxel and xanafide exhibited comparable TGI values: 20, 25 and 35 μ M. Vinorelbine and gemcitabine were less potent as shown by their respective 2.6- to 5.7-fold higher TGI concentrations, respectively (Table 2).
In SKBR-3 cells, gemcitabine and docetaxel induced total growth inhibition at 30 μ M. Paclitaxel, xanafide and vinorelbine exhibited comparable TGI concentrations, 35, 45 and 50 μ M, respectively. The TGI for doxorubicin was 80 μ M, 9-fold higher than that of xanafide (Table 2).
In T47D cell line, vinorelbine and gemcitabine induced similar cytotoxicity (TGI concentration of 17 μ M). Paclitaxel and docetaxel showed TGI concentrations of 35 and 60 μ M, respectively. Xanafide did not induce any complete growth inhibition in this cell line (Table 2).
These results indicate that the four breast cell lines tested exhibited differential sensitivity to xanafide and the common chemotherapeutic agents tested. Considering the TGI concentrations (Table 2) and the net cell killing achieved by xanafide, MCF-7 was the most sensitive cell line; MDA-MB-231 and SKBR-3 were almost equally sensitive while T47D was less responsive to this agent.
In vivo antitumour activity
On the basis of its cytotoxic activity in vitro, xanafide was further evaluated for in vivo activity in two ER+ and ER− breast cancer cell lines, MCF-7 and MDA-MB-231, respectively. The two cell lines were implanted i.p. and s.c. in NCr nude mice using the hollow fibre assay. Animals were treated with saline (control group), docetaxel dosed at 5 and 12.5 mg kg−1, i.p., or xanafide at 30 mg kg−1, i.p. on a q.d. × 5 treatment schedule, beginning on day 2 post-fibre implantation (days 3–7).
As shown in Figure 2, in the fibres retrieved from the i.p. sites, xanafide, administered as single agent, was effective at reducing the tumour cells growth of MCF-7 and MDA-MB-231 by 41 and 46%, respectively, as compared with control (P<0.05). Docetaxel exhibited dose-dependent growth inhibitory effects. At the lowest dose used, 5 mg kg−1, docetaxel produced a growth inhibition of 36 and 45%, in MCF-7 and MDA-MB-231, respectively (P<0.05). At 12.5 mg kg−1, the growth inhibition elicited was 39 and 51%, in MCF-7 and MDA-MB-231, respectively (P<0.05). These results show that xanafide was slightly more potent than docetaxel at its highest dose, in MCF-7. In contrast, its potency was lower than that of docetaxel in MDA-MB-231.
Antitumour effect of xanafide in comparison with docetaxel in MCF-7 and MDA-MB-231 breast cell lines in the in vivo hollow fibre assay. Fibres filled with the cells were implanted at the intraperitoneal (i.p.) and subcutaneous (s.c.) compartments of NCr nu/nu mice. The animals were treated with saline (control), xanafide (30 mg kg−1) or docetaxel (5 & 12.5 mg kg−1). Drugs were administrated once daily by i.p. injection from days 3–7 after implantation. On day 8, mice were killed and fibres were retrieved. The effectiveness of the drugs was evaluated on the basis of growth inhibition of the cells determined by MTT assay, as described in Materials and Methods.
In the fibres retrieved from the s.c. sites (Figure 2), xanafide administered as single agent produced comparable growth inhibition in MCF-7 and MDA-MB-231 cell lines, reducing the growth by 42 and 40%, respectively (P<0.05). Docetaxel showed dose-dependent inhibitory effects. At the lowest dose, the growth inhibition obtained was 31 and 36%, in MDA-MB-231 and MCF-7, respectively (P<0.05). At the highest dose used, 12.5 mg kg−1, the growth inhibition induced was 42 and 46%, in MCF-7 and MDA-MB-231, respectively (P<0.05).
Body weights were recorded daily during the course of the study, and expressed as the difference observed relative to start of treatment. For the docetaxel treated mice no loss in body weight was observed while in the xanafide treated mice, body weight was reduced by 12% by day 8, which was within the acceptable range based on NCI established criteria (Figure 3).
Discussion
Amonafide, a DNA-intercalating agent and topoisomerase II inhibitor, has been used as first-line treatment for MBC. However, amonafide is extensively metabolised, including N-acetylation to an active metabolite, N-acetyl amonafide, and the extent of amonafide N-acetylation is the major determinant of myelosuppression (Ratain et al, 1995). As a result, several compounds having structural analogy to amonafide have been synthesized (Sami et al, 1993, 2000; Dorr et al, 2001). Among these, azonafide has shown high potency against a panel of human colon cancer cell lines and was active against i.p. P388 leukaemia and s.c. B16 melanoma murine models (Sami et al, 1993).
Xanafide, the new formulation of amonafide, has been synthesized aiming at reducing the toxicity and improving the therapeutic index of the parent drug, amonafide. We have previously shown that xanafide and amonafide hydrochloride have comparable and significant inhibitory activity both in vitro against the three cell lines of the NCI prescreen program: H460 (non-small cell lung), SF268 (glioma) and MCF-7 (breast), and in vivo in MCF-7 (breast), COLO205 (colon) and PC-3 (prostate) cell lines, using the hollow fibre assay (Alami et al, 2003).
The aim of this study was to further investigate the antitumour effects of xanafide, in comparison with common breast drugs in a panel of breast cell lines well characterised for their oestrogen receptor, p53 status, Her-2 and topoisomerase II α and β levels: MCF-7, MDA-MB-231, SKBR-3 and T47D (Table 1). Xanafide exhibited a steep response curve in all four cell lines tested (Figure 1A–D). The GI 50 and TGI concentrations clearly show that these cell lines displayed differential sensitivity to xanafide with MCF-7 (ER+/p53 wild-type) being the most sensitive and T47 D (ER+/p53 mutated) the most resistant. Although this cell line was responsive to low doses of the other drugs tested, the lack of activity of xanafide in the T47D could be, in part, due to its long doubling time.
Furthermore, xanafide has proved to be more active than the taxanes, gemcitabine, vinorelbine and doxorubicin in MCF-7. The Two ER−/p53 mutated cell lines (MDA-MB-231 and SKBR-3) displayed comparable in vitro responsiveness to xanafide as demonstrated by their respective GI50 and TGI concentrations (Table 2).
Our in vitro results correlate with the in vivo data where xanafide was slightly more potent than docetaxel at its highest dose, in MCF-7 (Figure 2). These findings suggest a specificity of xanafide against the ER+, p53 w/t MCF-7 cell line.
These data raise the question of what are the mechanisms underlying the response to xanafide. Several clinical observations indicate a role for oestrogen and ER in the development, progression and treatment of human breast cancer (Angeloni et al, 2004). In addition, there is substantial evidence showing that alterations in the tumour suppressor gene, p53, are associated with the development of several types of cancer, including breast cancer (Hollstein et al, 1991). Considering that the p53 gene is mutated in approximately 50% of all tumours, its role in the control of cell cycle progression, maintenance of DNA integrity and induction of apoptosis is well documented (Zhan et al, 1993; Yonish-Rouach et al, 1995). It has also been shown that in breast cancer, p53 mutations are associated with a decrease in disease-free and overall survival of patients (Sirvent et al, 2001). Previous studies have reported that the ability of p53 to control the expression of ERα could suggest that specific p53 mutations in breast tumours may contribute not only to oncogenesis and drug resistance, but also to the more aggressive phenotype associated with the loss of ER expression. Interestingly, a high percentage of breast tumours with p53 mutations are ER-negative (Berns et al, 1996).
Our results showed that the two ER−/p53 mutated cell lines MDA-MB-231 and SKBR-3 exhibited moderate sensitivity to xanafide, whereas T47 D (ER+/p53 mutated) was more resistant to xanafide, with no induced cell killing, as compared with the extent of the anti-proliferative effect observed with MCF-7 (ER+/p53 wt) (Table 2). These findings may partially support a mechanism of responsiveness to xanafide in ER+ breast cancer where an active p53 gene is required. Additionally, related studies have shown that p53 was a negative regulator of the ER signalling pathways, suggesting a crosstalk between p53 and ER in breast cancer (Yu et al, 1997).
On the other hand, the DNA damage induced by topo II inhibitors triggers the p53-dependent apoptotic pathway that lead to cell cycle arrest (p21, cyclins, GADD45, PCNA) or to apotosis (Bcl-2, Bax, surviving, scotin) (Valkov and Sullivan, 2003). Related studies using tumour cell lines tested for their p53 status have shown that mutations of p53 correlate with drug resistance to a wide spectrum of anticancer agents, including topo II inhibitors (O'Connor et al, 1997; Sirvent et al, 2001). Usually, wild-type p53 expression predisposes cells to a more rapid rate of cell death after DNA damage. Previous studies have reported that non-small cell lung cancer cells having p53 mutations showed significantly poorer response to intensive chemotherapy that included etoposide and epirubicin (Vogt et al, 2002). In addition, treatment of MCF-7 with doxorubicin resulted in an increase of p53 expression, confirming a p53-mediated response to doxorubicin in cells containing a wild-type p53 gene product (Liem et al, 2003). Additional work has revealed that loss of wild-type p53 function confers resistance to etoposide in neuroblastoma cells (Keshelava et al, 2001) and in glioma cells (Yin et al, 2000). Others have also reported that p53 status in breast cancer patients correlated with a poor response to epirubicin (Mottolese et al, 2000). Furthermore, it has been postulated that the cell cycle arrest effect of wild-type p53 on cell cycle regulated topo IIα expression could potentially provide a sufficient amount of target enzyme for optimisation of treatment with topoisomerase II inhibitors (Valkov and Sullivan, 2003), thus supporting the greater potency of xanafide in MCF-7 cell line.
In addition, the topoisomerase II α gene, TOP2 α, is located at chromosome band 17q12-q21, close to the ErbB-2 oncogene (HER-2/neu), which is the most commonly amplified oncogene in breast cancer. Because of the physical proximity to ErbB-2, copy number aberrations may also occur in the topoIIα gene, which may be related to the altered chemosensitivity to topoII inhibitors (Jarvinen and Liu, 2006). Our results show that xanafide sensitivity was not correlated with expression levels of both topoisomerase II α and β. Considering the TGI concentrations, MDA-MB-231 and SKBR-3 expressing low levels and high levels of both isoforms, respectively, exhibited comparable sensitivity to xanafide. Our data are in agreement with those reported by Tewey et al (1984) where sensitivity to the topo II inhibitor, doxorubicin, showed no correlation with expression of either of the topoisomerase II isoforms.
In view of the previous findings together with our results, we speculate that p53 and ER and their signalling pathways are likely important determinants of breast tumour cells sensitivity to xanafide. Understanding these relationships may lead to strategies for xanafide-based chemotherapy optimisation and further precision targeting of tumour cells to avoid drug resistance and thereby chemotherapy failure. Furthermore, the steep response curves of xanafide activity in the four breast cell lines tested suggest that accurate individualised patient dosing is critically important for maximising clinical response while minimising neutropenic variability.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Alami N, Paterson J, Banerjee K, Yu Q, Grieshaber C, Leyland-Jones B (2003) Cytotoxicity of Two New Derivatives of Amonafide in Human Tumor Cell lines In vitro and In vivo Using the Hollow Fiber Assay. Washington, DC: 94th Annual AACR Meeting
Andersson BS, Beran M, Bakic M, Silberman LE, Newman RA, Zwelling LA (1987) In vitro toxicity and DNA cleaving capacity of benzisoquinolinedione (nafidimide; NSC 308847) in human leukemia. Cancer Res 47: 1040–1044
Angeloni SV, Martin MB, Garcia-Morales P, Castro-galache MD, Ferragut JA, Saceda M (2004) Regulation of estrogen receptor-alpha expression by the tumor suppressor gene p53 in MCF-7 cells. J Endocrinol 180: 497–504
Berns EM, Klijn JG, Smid M, van Staveren IL, Look MP, van Putten WL, Foekens JA (1996) TP53 and MYC gene alterations independently predict poor prognosis in breast cancer patients. Gene Chromosome Canc 16: 170–179
Blum JL, Jones SE, Buzdar AU, LoRusso PM, Kuter I, Vogel C, Osterwalder B, Burger HU, Brown CS, Griffin T (1999) Multicenter phase II study of capecitabine in paclitaxel-refractory metastatic breast cancer. J Clin Oncol 17: 485
Brana MF, Ramos A (2001) Naphthalimides as anti-cancer agents: synthesis and biological activity. Curr Med Chem Anti-Cancer Agents 1: 237–255
Costanza ME, Berry D, Henderson IC, Ratain MJ, Wu K, Shapiro C, Duggan D, Kalra J, Berkowitz I, Lyss AP (1995) Amonafide: an active agent in the treatment of previously untreated advanced breast cancer-a cancer and leukemia group B study (CALGB 8642). Clin cancer Res 1: 699–704
Dorr RT, Liddil JD, Sami SM, Remers W, Hersh EM, Alberts DS (2001) Preclinical antitumor activity of the azonafide series of anthracene-based DNA intercalators. Anticancer Drug 12: 213–220
Epstein RJ, Smith PJ (1988) Estrogen-induced potentiation of DNA damage and cytotoxicity in human breast cancer cells treated with topoisomerase II-interactive antitumor drugs. Cancer Res 48: 297–303
Esteva FJ, Valero V, Pusztai L, Boehnke-Michaud L, Budzar AU, Hortobagyi GN (2001) Chemotherapy of metastatic breast cancer: what to expect in 2001 and beyond. Oncologist 6: 133–146
Ghersi D, Wilcken N, Simes J, Donoghue E (2005) Taxane containing regimens for metastatic breast cancer. Cochrane Database Syst Rev 18: CD003366
Gralow JR (2005) Optimizing the treatment of metastatic breast cancer. Breast Cancer Res Treat 89: S9–S15
Hollingshead MG, Alley MC, Camalier RF, Abbott BJ, Mayo JG, Malspeis L, Grever MR (1995) In vivo cultivation of tumor cells in hollow fibers. Life Sci 57: 131–141
Hollstein M, Sidransky D, Vogelstein B, Harris CC (1991) p53 mutations in human cancers. Science 253: 49–53
Hortobagyi GN, Piccart-Gebhart MJ (1996) Current management of advanced breast cancer. Semin Oncol 23: 1–5
Houlbrook S, Addison CM, Davies SL, Carmichael J, Stratford IJ, Harris AL, Hickson ID (1995) Relationship between expression of topoisomerase II isoforms and intrinsic sensitivity to topoisomerase II inhibitors in breast cancer cell lines. Br J Cancer 72: 1454–1461
Hsiang YH, Jiang JB, Liu LF (1989) Topoisomerase II-mediated DNA cleavage by amonafide and its structural analogs. Mol Pharmacol 36: 371–376
Jarvinen TA, Liu ET (2006) Simultaneous amplification of HER-2 (ERBB2) and topoisomerase IIalpha (TOP2A) genes – molecular basis for combination chemotherapy in cancer. Curr Cancer Drug Targets 6: 579–602
Keshelava N, Zuo JJ, Chen P, Waidyaratne SN, Luna MC, Gomer CJ, Triche TJ, Reynolds CP (2001) Loss of p53 function confers high-level multidrug resistance in neuroblastoma cell lines. Cancer Res 61: 6185–6193
Kroger N, Achterrath W, Hegewisch-Becker S, Mross K, Zander AR (1999) Current options in treatment of anthracycline-resistant breast cancer. Cancer Treat Rev 25: 279–291
Liem AA, Appleyard MV, O'Neill MA, Hupp TR, Chamberlain MP, Thompson AM (2003) Doxorubicin and vinorelbine act independently via p53 expression and p38 activation respectively in breast cancer cell lines. Br J Cancer 88: 1281–1284
Livingston RB, Ellis GK, Gralow JR, Williams MA, White R, McGuirt C, Adamkiewicz BB, Long CA (1997) Dose-intensive vinorelbine with concurrent granulocyte colony-stimulating factor support in paclitaxel-refractory metastatic breast cancer. J Clin Oncol 15: 1395–1400
Martin M, Ruiz A, Munoz M, Balil A, Garcia-Mata J, Calvo L, Carrasco E, Mahillo E, casado A, Garcia-Saenz JA, Escudero MJ, Guillem V, Jara C, Ribelles N, Salas F, Soto C, Morales-Vasquez F, Rodriguez CA, Adrover E, Mel JR (2007) Gemcitabine plus vinorelbine versus vinorelbine monotherapy in patients with metastatic breast cancer previously treated with anthracyclines and taxanes: final results of the phase III Spanish Breast Cancer Research Group (GEICAM) trial. Lancet Oncol 8: 219–225
Montero A, Fossella F, Hortobagyi G, Valero V (2005) Docetaxel for treatment of solid tumours: a systematic review of clinical data. Lancet Oncol 6: 229–239
Mottolese M, Benevelo M, Del Monte G, Buglioni S, Papaldo P, Nistico C, Di Filippo F, Vasselli S, Vici P, Botti C (2000) Role of p53 and BCL-2 in high-risk breast cancer patients treated with adjuvant anthracycline-based chemotherapy. J Cancer Res Clin Oncol 126: 722–729
O'Connor PM, Jackman J, Bae I, Myers TG, Fan S, Mutoh M, Scudiero DA, Monks A, Sausville EA, Weinstein JN, Friend S, Fornace AJ, Kohn KW (1997) Characterization of the p53 tumor suppressor pathway in cell lines of the National Cancer Institute anticancer drug screen and correlations with the growth-inhibitory potency of 123 anticancer agents. Cancer Res 57: 4285–4300
Pronzato P, Rondini M (2006) First line chemotherapy of metastatic breast cancer. Ann Oncol 17: v165–v168
Ratain MJ, Mick R, Berezin F, Janisch L, Schilsky RL, Vogelzang NJ, Lane LB (1993) Phase I study of amonafide dosing based on acetylator phenotype. Cancer Res 53: 2304–2308
Ratain MJ, Mick R, Berezin F, Janisch L, Schilsky RL, Williams SF, Smiddy J (1991) Paradoxical relationship between acetylator phenotype and amonafide toxicity. Clin Pharmacol Ther 50: 573–579
Ratain MJ, rosner G, Allen SL, Costanza M, Van Echo DA, henderson IC, Schilsky RL (1995) Population pharmacodynamic study of amonafide: a Cancer and Leukemia Group B study. J Clin Oncol 13: 741–747
Sami SM, Dorr RT, Alberts DS, Remers WA (1993) 2-substituted 1, 2-dihydro-3H-dibenz[de, h]isoquinoline-1, 3-diones. A new class of antitumor agent. J Med Chem 36: 765–770
Sami SM, Dorr RT, Alberts DS, Sólyom AM, Remers WA (2000) Analogues of amonafide and azonafide with novel ring systems. J Med Chem 43: 3067–3073
Schiff PB, Fant J, Horwitz SB (1979) Promotion of microtubule assembly in vitro by Paclitaxel. Nature 277: 665–667
Sirvent JJ, Fortuno-Mar A, Olona M, Orti A (2001) Prognostic value of p53 protein expression and clinicopathological factors in infiltrating ductal carcinoma of the breast. A study of 192 patients. Histol Histopathol 16: 99–106
Skehan P, Storeng R, Scudiero D, Monks A, McMahon J, Vistica D, Warren JT, Bokesch H, Kenney S, Boyd MR (1990) New colorimetric cytotoxicity assay for anticancer-drug screening. J Natl Cancer Inst 82: 1107–1112
Tewey KM, Rowe TC, Yang L, Halligan BD, Liu LF (1984) Adriamycin-induced DNA damage mediated by mammalian DNA topoisomerase II. Science 226: 466–468
Valerio MR, Cicero G, Armata MG, Bajardi E, Crosta A, Badalamenti G, Arcara C, Agosta G, Vieni S, Latteri F, Russo A, Gulotta G, Gebbia N (2001) Gemcitabine (G) in Pre-treated Breast Cancer (BC). San Francisco, CA: 37th Annual Meeting of the American Society of Clinical Oncology, 20, 51b, abstract # 1953
Valkov NI, Sullivan DM (2003) Tumor p53 status and response to topoisomerase II inhibitors. Drug Resist Updat 6: 27–39
Vogelstein B, Lane D, Levine AJ (2000) Surfing the p53 network. Nature 408: 307–310
Vogt P, Zaczek A, Klinke F, Granetzny A, Bielawski K, Falkiewicz B (2002) p53 gene status in relation to ex vivo chemosensitivity of non-small cell lung cancer. J Cancer Res Clin Oncol 128: 141–147
Yin D, Tamaki N, Kokunai T (2000) Wild-type p53-dependent etoposide-induced apoptosis mediated by caspase-3 activation in human glioma cells. J Neurosurg 93: 289–297
Yonish-Rouach E, Deguin V, Zaitchouk T, Breugnot C, Mishal Z, Jenkins JR, May E (1995) Transcriptional activation plays a role in the induction of apoptosis by transiently transfected wild-type p53. Oncogene 11: 2197–2205
Yu CL, Driggers P, Barrera-Hernandez G, Nunez SB, Segars JH, Cheng SY (1997) The Tumor Suppressor p53 is a negative regulator of estrogen receptor signaling pathways. Biochem Biophys Res Commun 239: 617–620
Zhan Q, carrier F, Fornace AJ (1993) Induction of cellular p53 activity by DNA-damaging agents and growth arrest. Mol Cell Biol 13: 4242–4250
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Alami, N., Paterson, J., Belanger, S. et al. Comparative analysis of xanafide cytotoxicity in breast cancer cell lines. Br J Cancer 97, 58–64 (2007). https://doi.org/10.1038/sj.bjc.6603829
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603829
Keywords
This article is cited by
-
Cytotoxicity, anticancer, and antioxidant properties of mono and bis-naphthalimido β-lactam conjugates
Medicinal Chemistry Research (2020)
-
Novel PEG-coated niosomes based on bola-surfactant as drug carriers for 5-fluorouracil
Biomedical Microdevices (2009)
-
Functional expression of voltage-gated sodium channels Nav1.5 in human breast caner cell line MDA-MB-231
Journal of Huazhong University of Science and Technology [Medical Sciences] (2009)