Abstract
Optimal management of clinically localised prostate cancer presents unique challenges, because of its highly variable and often indolent natural history. There is an urgent need to predict more accurately its natural history, in order to avoid unnecessary treatment. Medical records of men diagnosed with clinically localised prostate cancer, in the UK, between 1990 and 1996 were reviewed to identify those who were conservatively treated, under age 76 years at the time of pathological diagnosis and had a baseline prostate-specific antigen (PSA) measurement. Diagnostic biopsy specimens were centrally reviewed to assign primary and secondary Gleason grades. The primary end point was death from prostate cancer and multivariate models were constructed to determine its best predictors. A total of 2333 eligible patients were identified. The most important prognostic factors were Gleason score and baseline PSA level. These factors were largely independent and together, contributed substantially more predictive power than either one alone. Clinical stage and extent of disease determined, either from needle biopsy or transurethral resection of the prostate (TURP) chips, provided some additional prognostic information. In conclusion, a model using Gleason score and PSA level identified three subgroups comprising 17, 50, and 33% of the cohort with a 10-year prostate cancer specific mortality of <10, 10–30, and >30%, respectively. This classification is a substantial improvement on previous ones using only Gleason score, but better markers are needed to predict survival more accurately in the intermediate group of patients.
Similar content being viewed by others
Main
The natural history of prostate cancer is highly variable and difficult to predict. Over treatment of asymptomatic patients is a serious problem leading to substantial morbidity. Introduction of prostate-specific antigen (PSA) testing in some countries has exacerbated this problem, leading to a much higher reported incidence rate, but having little influence on mortality rates (Evans and Møller, 2003). In the United States, where PSA testing has been common, the incidence to mortality ratio is about 7.6. Conversely, in the United Kingdom, where PSA testing is not performed routinely, the ratio is approximately 2.5. Autopsy series have confirmed that histologically proven prostate cancer can be identified in approximately 40% of men over 50 years of age who die of other causes (Breslow et al, 1977; Sakr et al, 1994). This is about four times higher than the lifetime risk for American men to be diagnosed with prostate cancer (approximately 11%), indicating that more intensive screening is likely to uncover even more indolent disease. This had led many countries, in particular the United Kingdom, to endorse a more conservative approach to disease detection and management. In the UK, PSA screening is not endorsed by the health service (although it is available on request) and radical prostatectomy or radiation therapy is not common practice. However, this approach is not without problems, since a substantial proportion of men develop progressive disease from which they ultimately die. Furthermore, conservative management can lead to considerable anxiety, especially when the clinical outcome is so uncertain.
Several studies have attempted to document the long-term risk of metastases and death from prostate cancer in men with conservatively managed, clinically localised cancers (Chodak et al, 1994; Albertsen et al, 1995, 1998, 2005a; Adolfsson et al, 1997; Holmberg et al, 2002; Johansson et al, 2004; Bill-Axelson et al, 2005). Two of these (Albertsen et al, 1998; Johansson et al, 2004) estimated outcome based on histological tumour grade, but did not include either clinical stage or initial serum PSA level and reviewed Gleason grades. The former (Albertsen et al, 1998) reported long-term outcomes for 767 men aged 55–74 years at diagnosis with conservatively treated clinically localised prostate cancer. Men with cancers that have Gleason scores of 2–4, 5, 6, 7, and 8–10 had a 4–7, 6–11, 18–30, 42–70, and 60–87% chance, respectively, of dying from prostate cancer within 15 years of diagnosis, depending on their age at diagnosis. Their revised estimate of 20-year survival (Albertsen et al, 2005a) indicated that annual mortality rates remained stable after 15 years from diagnosis. In contrast to these findings, the latter study (Johansson et al, 2004) reported an approximately three-fold increase in the rate of progression and prostate cancer-specific mortality rate after 15 years among their small cohort of 223 patients.
The first randomised trial of primary treatment with curative intent for men with localised prostate cancer was reported by Holmberg et al (2002) and later by Bill-Axelson et al (2005). This trial included 695 men, with clinically localised prostate cancer, randomised to either radical prostatectomy or no initial treatment with systemic treatment deferred until the development of symptomatic progression. The authors found a reduced risk of progression and death from prostate cancer in the radically treated men, but concluded that the disease-specific benefits of radical prostatectomy must be weighed carefully against the potential impact that surgery can have on quality of life. Other studies (Chodak et al, 1994; Albertsen et al, 1995, 1998, 2005a; Adolfsson et al, 1997; Holmberg et al, 2002) have concluded that watchful waiting or no initial treatment with treatment delayed until the development of symptomatic metastatic disease remains a viable treatment option.
These studies emphasise the varied natural history of clinically localised prostate cancer, especially for the intermediate risk prostate cancers with Gleason score 6–7.
A basic tenet of an effective screening programme is that the natural history of the disease should be understood well and that early detection can have an important impact on outcome. Neither of these requirements has been satisfied for prostate screening. This study was performed to evaluate the utility of whether other factors such as PSA, clinical stage and extent of disease could provide useful prognostic information in addition to histological grade.
Materials and methods
Study population and data collection
This was a population-based study in which potential cases were identified from six cancer registries in Great Britain. Within each region, collaborating hospitals were sought and cases from these hospitals were reviewed. National approval was obtained from the Northern Multi-Research Ethics Committee, followed by local ethics committee approval at each of the collaborating hospital trusts (Appendix A).
Men were included in this study if they were under age 76 years at the date of diagnosis and had clinically localised prostate cancer diagnosed by transurethral resection of the prostate (TURP) or needle biopsy. Diagnosis between 1990 and 1996 (inclusively) and a baseline PSA were required.
Patients treated by radical prostatectomy or radiation therapy within 6 months of diagnosis were excluded. In addition, those with objective evidence of metastatic disease (by bone scan, X-ray, radiograph, CT scan, MRI, bone biopsy, lymph node biopsy, pelvic lymph node dissection) or clinical indications of metastatic disease (including pathologic fracture, soft tissue metastases, spinal compression, or bone pain), or a PSA measurement over 100 ng ml−1 at or within 6 months of diagnosis were also excluded. These exclusions were a pragmatic method of focusing the study on patients who were very likely to have truly localised disease at presentation. Men who had hormone therapy prior to diagnostic biopsy were also excluded, because of the influence of hormone treatment on interpreting Gleason grade. We also excluded men who died within 6 months of diagnosis, or had less than 6 months of follow-up.
Registry data had limited utility for eliminating ineligible cases, thus a review of hospital records was necessary to establish eligibility. The review process and selection of cases is summarised in Figure 1.
Registry data collection officers and trained medical staff conducted on-site medical record reviews at each of 51 hospital trusts (Appendix A).
Clinical staging was centrally reviewed and, where unstated in the notes, was assigned, where possible, by an urologist based on the reported findings. In approximately 24% of cases, no information was available and in a further 16% of cases, stage could not be assigned. In both circumstances, these cases were designated Tx.
Original histological specimens from the diagnostic procedure (needle biopsy or TURP) were requested, collected, and centrally reviewed by a panel of expert urological pathologists to confirm the diagnosis and, where necessary, to reassign Gleason grades for all the prostate cancers using a conventional interpretation (Deshmukh and Foster, 1997) of the Gleason grading system. Approximately 12% of requested specimens were missing or unidentifiable in hospital pathology databases. A further 17% of cases had no Gleason grade assigned for a variety of reasons (Figure 1). Outcomes were determined through medical records and cancer registry data. In January 2005, the cancer registries were queried to obtain the most up-to-date survival data. Date of last follow-up was different for each cancer registry; the earliest was March 2004 and the latest was January 2005. Where available, death certificates for deceased patients were reviewed to verify cause of death. Deaths were divided into two categories, death from prostate cancer and death from other causes, according to standardised World Health Organisation criteria. Patients still alive at last follow-up were censored at that date.
Disease progression (treatment failure) was defined as clinical, histological, or radiographic evidence of metastatic disease (lymph node, bone, or soft tissue); or institution of additional hormone therapy, radiation therapy, surgery, chemotherapy, or death certified to be from prostate cancer.
Statistics
The primary end point to this study was time to death from prostate cancer. An initial analysis characterised patient status at different follow-up times (death from prostate cancer, death from other causes, alive with progression, alive without progression) in which censoring was done only if alive and progression free at last follow-up. Subsequent analyses of the main end points were performed by proportional hazards models, censoring at the time of death from other causes, or latest follow-up time. All follow-up times commenced at the point of 6 months following diagnosis. The following variables were recorded: Gleason score, all available PSA values, clinical stage, extent of disease (proportion of TURP chips with disease or linear proportion of needle biopsy containing disease), age at diagnosis, method of diagnosis (TURP or needle biopsy), and initial treatment (no initial treatment or early hormone management). Baseline PSA was defined as the last PSA value within 6 months of diagnosis (including pre-diagnostic values), but before initiation of hormone therapy and at least 3 weeks after any biopsy. Patients for which any of these values greater than 100 ng ml−1 were excluded.
Variables were first examined separately and then multivariate models were constructed by a forward stepwise selection method. For the multivariate models, a single linear trend variable across categories was used for assessing the importance of a new variable. If the variable was included, a second variable indicating missing (unassigned) data was added before proceeding to examine further variables. This was done to avoid loss of patients when one variable was missing. A predictor was developed using Gleason score and separate categories of PSA to create prognostic groups. All P-values are two-sided and 95% confidence intervals were based on the normal distribution with parameters derived from partial likelihood calculations.
Results
Cohort assembly
The process of identification of eligible patients is summarised in Figure 1.
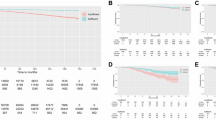
Of 2333 men eligible for evaluation, 1663 were managed by no initial treatment and 670 were managed by early hormone therapy. Overall, the median age at diagnosis was 70.1 years (range 44–76 years) and the median follow-up was 117 months (range 88–180 months). Most men (80%) were diagnosed after age 65 years. A competing risk analysis showed that after 10 years of follow-up, 55% of the men had died, 24% from prostate cancer and 31% from other causes and only 22% were still alive without progression (Figure 2).
Early hormone therapy treated patients were diagnosed more recently and had a shorter follow-up time, but the age at diagnosis was similar for both cohorts (P=0.25). Diagnosis was made by TURP in 1255 men (54%), needle biopsy in 1039 men (45%) and was unspecified in 39 men (1%). Patients treated early by hormone manipulation had a worse prognosis, even after multivariate adjustment. Consequently, results are also given separately for the two methods of initial management.
The distribution of baseline factors and the univariate risk of death from prostate cancer for these factors are shown in Table 1. Separate analyses for patients with early hormone therapy and no initial treatment are given in Appendix A (Table A1).
Gleason grade
Reviewed Gleason scores were available for 71% of the total cohort, 71% of those treated by no initial treatment, and 72% of those treated by early hormone therapy. Gleason score had the greatest discriminating power, even though this was based on a subset of the cohort (Table 1). A clear gradation was seen across groups with a χ2 (trend) of 186, in the total cohort, for prostate cancer death. The predictive power was weaker in patients initially treated by early hormone therapy, but was still stronger than any other variable for this group. Patients, whose histology was not available for review, were similar to the overall group, with a survival curve very similar to those with a Gleason score of 7. Those with a Gleason score of 4 or 5 had a 10-year prostate cancer survival rate of 92% compared to 41% for those with Gleason score 9 or 10. We further subdivided the Gleason score 7 into 3+4 and 4+3, but they behaved similarly (HR 2.17 vs 2.51, 10 years survival 73 vs 68% respectively).
Baseline PSA
Baseline PSA values were the second most useful variable and almost as discriminating as Gleason score. The χ2 (trend) was 153 for prostate cancer death. Again, a clear gradient was seen with survival at 10 years, being 86% for men with PSA values <4 ng ml−1, but only 46% for men with values between 50 and 100 ng ml−1. Much of the impact of PSA was independent of Gleason score, as can be seen from the multivariate analysis (Table 2a). Low values were less predictive for patients treated by early hormone management.
Clinical stage and extent of disease
A total of 1387 (60%) patients had sufficient information available to assign a clinical stage. In univariate analysis, a clear but smaller difference than for Gleason score or baseline PSA was seen. Extent of disease proved to be more useful than clinical stage for both cohorts (Table 1) and retained significance in multivariate models.
Age, method, and year of diagnosis
Age had a clear effect on non-prostate cancer death as expected. The 10-year death rates from other causes were 18, 30, 42, 47% for ages <65, 65–70, 71–73, 74–75 respectively (χ2 (trend)=104). An effect was also seen for death from prostate cancer. However, no effect was seen on progression rates (data not shown), suggesting this may represent confounding with other established risk factors, or misclassification of cause of death in the elderly.
Method of diagnosis (TURP or needle biopsy) and year of diagnosis had little impact on outcome.
Multivariate model
A forward stepwise selection multivariate model was developed. The variables were entered in the following order and their relative strengths indicated by the increment in χ2 (Δχ2): Gleason Grade (186.4), PSA (84), age (15.2), percentage cancer in the biopsy (9.8), clinical stage (8.0), and year of diagnosis (2.8). Full details are given in Appendix A (Table A2 (a)). Separate models for no initial treatment and early hormone therapy are provided also in Appendix A (Table A2 (b) and (c)).
The most predictive variable was Gleason score, followed by baseline PSA, age, extent of disease, and clinical stage. Method of initial treatment was also important, even after adjustment for other factors, reflecting an additional selection of poor risk patients among those given early hormone therapy.
A multivariate model for prostate cancer death based only on different levels of Gleason score and baseline PSA is shown in Table 2a and Table 2b.
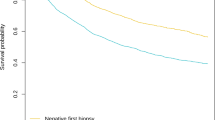
This was clearly better than the univariate models. Almost all of the information was contained in Gleason score and baseline PSA. With these two variables we were able to identify 17% of the cohort for which the Gleason score was⩽5 and PSA<25 ng ml−1 or the Gleason score was 6 and PSA⩽4 ng ml−1 where prostate cancer mortality at 10 years was less than 10% and 33% of the cohort with Gleason score 7 and PSA>25 ng ml−1, or Gleason score 8 and PSA>10 ng ml−1, or Gleason score⩾9 where prostate cancer mortality at 10 years was greater than 30%. This last group could be further split into a very poor prognostic group (Gleason score⩾9 and PSA>25 ng ml−1) comprising 5% of men with a 10-year prostate cancer mortality greater than 75% (Table 2b).
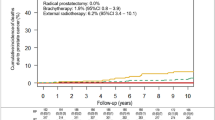
The relative importance of death from prostate cancer vs other causes over the first 10 years of follow-up for different prognostic groups is shown (Figure 3) separately for men aged 70 years or less and men aged more than 70 years, at diagnosis.
Discussion
Prostate cancer is currently the second leading cause of cancer death among men in both the UK and USA. However, approximately half the men diagnosed with this disease do not die from it, even in the absence of radical treatment (Satariano et al, 1998). This makes counselling patients about management difficult. Recent results from the Scandinavian Prostate Cancer Study Group (Bill-Axelson et al, 2005) demonstrate a reduction in metastatic disease and prostate cancer-specific mortality for radical prostatectomy compared to watchful waiting, but the gains are small and it is not clear which men will benefit in this. Our data incorporate informative prognostic parameters not analysed in previous studies on conservatively treated men. In agreement with Albertsen et al (1995) and Johansson et al (2004), we found Gleason score to be an important determinant of cancer-specific mortality. In addition, we found baseline PSA level and to a lesser extent clinical stage and extent of disease added further predictive value. Importantly, the information contained in PSA levels was largely independent of that available from Gleason score and vice versa, so that using both variables produced a simple classification into three groups with very different outcomes.
Compared to previous studies, there are several reasons why our findings are more applicable to a man diagnosed with localised prostate cancer in the modern era. Firstly, the incorporation of PSA augments the prognostic stratification by histological grading alone. Secondly, the Gleason scoring in our study more accurately reflects current pathological grading methods. Multiple investigators have documented an upward shift in Gleason score over time (Kondylis et al, 2003; Albertsen et al, 2005b) – not representative of a change in biology, but of pathologists today being more likely to assign higher Gleason scores. Albertsen et al (2005a, 2005b) assigned Gleason grades in 1990–1992 and 33% of patients had a Gleason score of 5 or less compared to our study where only 3% patients had this classification. Thirdly, in Albertsen's cohort, 24% of patients had a Charlson Index (Charlson et al, 1987) of two or greater, considered to be ‘significant co morbidity’. Consequently, the cohort represents probably a high proportion of patients not medically suitable, or patients deciding not to opt for primary curative therapy. Since conservative management was used for a much broader group of patients in the United Kingdom, our population-based cohort may be a more representative one for men faced with the choice of conservative vs curative-intent therapy. While 54% of our patients were diagnosed by TURP, which is much higher than would be found in a contemporary series, this did not have an impact on outcomes, PSA levels were on average also higher than for current series, but there were sufficient numbers of patients in all groups to obtain reliable prognostic information across the full spectrum of values. Lastly, our cohort is more than three times the size of previous studies, providing more accurate estimates of risk and greater statistical power.
Kattan et al (1998) found clinical stage, PSA, and Gleason grade to be parameters predictive of PSA recurrence for men treated by radical prostatectomy. In our study, clinical stage provided only a small additional amount of information on prostate cancer death. However, our information on clinical stage was unavailable for 40% of the cohort, and were recorded, was limited and based on a retrospective review of clinical notes from a variety of institutions. It is possible that carefully collected and complete prospective information would prove to be more prognostic. This is in contrast to the data on PSA that was 100% complete and centrally reviewed Gleason Grade, which was available for 71% of the cohort. Age was a strong predictor of death from causes other than prostate cancer, and provided some additional information on prostate cancer mortality. However, it did not predict progression, and its effect on prostate cancer mortality may reflect misclassification of cause of death in these elderly men.
Our analyses identified 33% of men with poor 10-year cancer-specific mortality (>30%), where no initial treatment is not a good option, especially when the risk of death from other causes is low. We also identified a group comprising 17% of men where the 10-year cancer-specific survival was very good (>90%). Long follow-up will be needed to see if these men remain at low risk of disease-related mortality, since it is not clear if mortality rate trends will plateau or continue to increase. In the Swedish (Johansson et al, 2004) cohort, cancer-specific mortality rates increased during years 15–20 following diagnosis relative to the initial 15 years, whereas Albertsen et al (2005a) found annual cancer-specific mortality rates to be unchanged after 15 years.
In our study, approximately 50% of patients have what may be considered an intermediate prognosis (10–30% 10-year cancer-specific mortality), where better markers of disease progression are needed. This applies especially to the 11% of men with Gleason score 6 and PSA level 4–10 ng ml−1, many of whom undoubtedly have a very good prognosis. Currently, we are collecting all available tumour blocks from the cohort to construct tissue micro-arrays. It is hoped that identification of new markers with altered DNA or protein expression in prostate cancer will help to highlight disease destined to be clinically relevant, especially for this intermediate group.
In conclusion, we have confirmed Gleason score as an important prognostic factor for men with conservatively treated localised prostate cancer and are the first to include PSA at diagnosis into the prognostic model for these patients. While providing valuable information for men considering or choosing conservative therapy, our study has also emphasised the urgent need to identify better markers of tumour behaviour to assist in formulating appropriate management of individual men with prostate cancer.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Adolfsson J, Steineck G, Hedlund P-O (1997) Deferred treatment of clinically localized low-grade prostate cancer: actual 10-year and projected 15-year follow-up of the Karolinska series. Urology 50: 722–726
Albertsen PC, Fryback DG, Storer BE, Kolon TF, Fine J (1995) Long-term survival among men with conservatively treated localized prostate cancer. JAMA 274: 626–631
Albertsen PC, Hanley JA, Barrows GH, Penson DF, Kowalczyk PD, Sanders MM, Fine J (2005a) Cancer and the Will Rogers phenomenon. J Natl Cancer Inst 97: 1248–1253
Albertsen P, Hanley JA, Fine J (2005b) 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA 293: 2095–2101
Albertsen PC, Hanley JA, Gleason DF, Barry MJ (1998) Competing risk analysis of men aged 55 to 74 years at diagnosis managed conservatively for clinically localized prostate cancer. JAMA 280: 975–980
Bill-Axelson A, Holmberg L, Ruutu M, Haggman M, Andersson SO, Bratell S, Spangberg A, Busch C, Nordling S, Garmo H, Palmgren J, Adami HO, Norlen BJ, Johansson JE, Scandinavian Prostate Cancer Group Study No. 4 (2005) Radical prostatectomy versus watchful waiting in early prostate cancer. N Engl J Med 352: 1977–1984
Breslow N, Chan CW, Dhom G, Drury RA, Franks LM, Gellei B, Lee YS, Lundberg S, Sparke B, Sternby NH, Tulinius H (1977) Latent carcinoma of prostate at autopsy in seven areas. The International Agency for Research on Cancer, Lyons, France. Int J Cancer 20: 680–688
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 40: 373–383
Chodak GW, Thisted RA, Gerber GS, Johansson JE, Adolfsson J, Jones GW, Chisholm GD, Moskovitz B, Livne PM, Warner J (1994) Results of conservative management of clinically localized prostate cancer. N Engl J Med 330: 242–248
Deshmukh N, Foster CS (1997) Grading prostate cancer. In Pathology of the Prostate Foster CS, Bostwick DG (eds) pp 191–227. Philadelphia: WB Saunders
Evans MS, Møller H (2003) Recent trends in prostate cancer incidence and mortality in Southeast England. Eur Urol 43: 337–341
Holmberg L, Bill-Axelson A, Helgesen F, Salo JO, Folmerz P, Haggman M, Andersson SO, Spangberg A, Busch C, Nordling S, Palmgren J, Adami HO, Johansson JE, Norlen BJ, Scandinavian Prostatic Cancer Group Study Number (2002) A randomized trial comparing radical prostatectomy with watchful waiting in early prostate cancer. N Engl J Med 347: 781–789
Johansson JE, Andren O, Andersson SO, Dickman PW, Holmberg L, Magnuson A, Adami HO (2004) Natural history of early, localized prostate cancer. JAMA 291: 2713–2719
Kattan MW, Eastham JA, Stapleton AMF, Wheeler TM, Scardino PT (1998) A preoperative nomogram for disease recurrence following radical prostatectomy for prostate cancer. J Natl Cancer Inst 90: 766–771
Kondylis FI, Moriarty RP, Bostwick D, Schellhammer PF (2003) Prostate cancer grade assignment: the effect of chronological, interpretive and translation bias. J Urol 170: 1189–1193
Sakr WA, Grignon DJ, Crissman JD, Heilbrun LK, Cassin BJ, Pontes JJ, Haas GP (1994) High grade prostatic intraepithelial neoplasia (HGPIN) and prostatic adenocarcinoma between the ages of 20-69: an autopsy study of 249 cases. In vivo 8: 439–443
Satariano WA, Ragland KE, Van Den Eeden SK (1998) Cause of death in men diagnosed with prostate cancer. Cancer 83: 1180–1188
Acknowledgements
We gratefully acknowledge support from Cancer Research UK, The Orchid Appeal, National Institutes of Health (SPORE) and the Koch Foundation. We also thank investigators and staff in the cancer registries and participating hospitals (Appendix A) for their support.
Funding bodies had no involvement in the design and conduct of the study, or in collection management, analysis and interpretation of the data, or in preparation, review or approval of the manuscript.
Author information
Authors and Affiliations
Consortia
Corresponding author
Appendix A
Appendix A
Members of the Transatlantic Prostate Group included listed authors and investigators designated by an asterisk.
Investigators in participating regional cancer registries and hospital trusts are listed below:
Thames Cancer Registry: Henrik Møller*, Shirley Bell (deceased), K Linklater, J Ottey V Fisher; Ashford & St Peter's, M Hall, N Harvey Hills; Barnet & Chase Farm, H Reid; Brighton and Sussex, N Kirkham, P Thomas; Bromley, D Nurse; Dartford & Gravesham, I Dickinson, P Thebe; East & North Hertfordshire, D Hanbury, M Ali-Izzi; Eastbourne, C Moffatt; Epsom & St Helier, M Bailey, L Temple; Essex Rivers Healthcare, W Aung, C. Booth; Frimley Park, B Montgomery, P Denham; Greenwich Healthcare, N Cetti, P Pinto; Guy's & St Thomas's, A Chandra, T O’Brien; Hammersmith Hospitals, N Livni; Havering Hospitals, I Saeed; Hillingdon, F Barker, T Beaven; King's Healthcare, G Muir, Z Khan; Kingston, C Jameson; Lewisham, A Giles; Mayday Healthcare, N Arsanious, A Arnaout; The Medway, E Boye; Mid Essex Hospitals; Mid Kent, M Boyle; North West London Hospitals, M Jarmulowicz; Royal Free Hampstead, RJ Morgan, A Bates; St Bartholomew's and The Royal London Hospitals, F Chinegwundoh, RTD Oliver, D Berney; Royal Surrey County, S De Sanctis; Southend, M Chappell; St George's, London, R Kirby, C Corbishley; St Mary's, London, A Patel, M Walker; West Hertfordshire, J Crisp, W Riddle; Worthing & Southlands Hospitals, J Grant.
Northern & Yorkshire Cancer Registry & Information Service: David Forman*, C Storer, C Bennett, C Spink; Airedale, I Appleyard, J O’Dowd; Hull & East Yorkshire, J Hetherington, A MacDonald; The Leeds Teaching Hospitals, P Whelan, P Quirke, P Harnden.
Oxford Cancer Intelligence Unit: Monica Roche*, Sandra Edwards, S Bose, P Hall; Heatherwood & Wexham Park, M Ali, O Karim; Milton Keynes, E Walker, S Jalloh; Northampton, M Miller, A Molyneux; Oxford Radcliffe, S Brewster, D Davies; Royal Berkshire & Battle, P Malone, C McCormick; Stoke Mandeville, J Greenland, A Padel
Welsh Cancer Intelligence & Surveillance Unit: John Steward*, Shelagh Reynolds, Lynda Roberts, Judith Adams; Ceredigion and Mid Wales, J Edwards, CGB Simpson; Conwy & Denbighshire, A Dalton, V Srinivasan; NE Wales, A De Bolla, C Burdge; Gwent Healthcare, W Bowsher, M Rashid; Swansea, M Lucas, C O’Brien; Cardiff & Vale, M Varma.
Scottish Cancer Registry: David Brewster*; The Lothian University Hospitals, J Royle, K Grigor; North Glasgow University Hospitals, D Kirk, A Milano, R Reid.
Merseyside & Cheshire Cancer Registry: Lyn Williams*, R Iddenden; Royal Liverpool University Hospital, CS Foster, P Cornford.
Memorial Sloan Kettering Cancer Center: H Lilja*, S Eggener*.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Cuzick, J., Fisher, G., Kattan, M. et al. Long-term outcome among men with conservatively treated localised prostate cancer. Br J Cancer 95, 1186–1194 (2006). https://doi.org/10.1038/sj.bjc.6603411
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6603411
Keywords
This article is cited by
-
Identification of FBXL4 as a Metastasis Associated Gene in Prostate Cancer
Scientific Reports (2017)
-
Validation of an RNA cell cycle progression score for predicting death from prostate cancer in a conservatively managed needle biopsy cohort
British Journal of Cancer (2015)
-
DNA methylation gene-based models indicating independent poor outcome in prostate cancer
BMC Cancer (2014)
-
An expression signature at diagnosis to estimate prostate cancer patients’ overall survival
Prostate Cancer and Prostatic Diseases (2014)
-
Focal amplification of the androgen receptor gene in hormone-naive human prostate cancer
British Journal of Cancer (2014)