Abstract
In a population-based study of 613 cases and 1082 controls, alcohol dehydrogenase 1B (ADH1B) genotype was not an independent risk factor for breast cancer, athough the possibility was raised that it modifies risk associated with high levels of alcohol consumption (OR 1.1, 95% confidence interval (CI) 0.8–1.6 for ADH1B*1/*1 genotype vs 0.2, 95% CI 0.1–1.0 for ADH1B*2 carriers).
Similar content being viewed by others
Main
Alcohol consumption is one of the few modifiable risk factors for breast cancer (Singletary and Gapstur, 2001; Collaborative Group on Hormonal Factors in Breast Cancer, 2002), and we also observed a dose-dependent effect of alcohol intake on breast cancer risk in a case–control study of women up to age 50 years in Germany (Kropp et al, 2001). However, drinking behaviour as well as susceptibility to alcohol-induced carcinogenesis may be influenced by individual genetic make-up. In this context, class I alcohol dehydrogenases (ADHs), which are important enzymes in the major pathway of alcohol metabolism in vivo and are expressed in normal mammary epithelium (Triano et al, 2003), may be relevant. The alcohol dehydrogenase 1B (ADH1B) gene (formerly called ADH2) exhibits genetic polymorphisms resulting in altered functional and catalytic properties in vitro (Agarwal, 2001). A strongly increased oxidation capability has been associated with the *2 allele (Bosron et al, 1983; Eriksson et al, 2001), an Arg47His substitution with reported allele frequencies ranging between 0 and 6.8% in Europeans (Brennan et al, 2004).
Previously, a significant inverse association between the ADH1B*2 allele and frequency of alcohol consumption was observed in a case-only study (Sturmer et al, 2002). We employed a population-based case–control study of women up to age 50 years to examine the potential effect of ADH1B genotype on the association between alcohol consumption and breast cancer risk.
Materials and methods
Study subjects and data collection
A detailed description of the underlying case–control study has been provided elsewhere (Chang-Claude et al, 2000). Patients up to age 50 years with a diagnosis of primary incident in situ or invasive breast cancer were recruited between 1 January 1992 and 31 December 1995. Controls were selected randomly from lists of residents supplied by population registries; for each patient, two controls were matched according to exact age and study region. Written informed consent from all participants was obtained. The study was approved by the ethics committee of the University of Heidelberg.
In total, 706 (70.2%) women of the 1005 breast cancer patients who were alive when identified completed the study questionnaire. Of all 2257 eligible controls, 1381 (61.2%) participated. Detailed information on demographic characteristics and various risk factors was elicited by means of a self-administered questionnaire. Alcohol consumption was assessed for three time periods, that is, 15–20, 20–30 and 30–50 years, and for different types of beverages (beer, wine, aperitifs, liquor and spirits). The detailed method for the calculation of average daily alcohol intake has been described previously (Kropp et al, 2001).
Menopausal status was defined as the reported state half a year before the reference date, which was the date of diagnosis for cases and the date of completion of the questionnaire for controls. The status of women with previous hysterectomy not accompanied by bilateral oophorectomy was classified as unknown.
The present analysis was restricted to 613 cases and 1082 controls with at least one parent of German nationality and who could be successfully genotyped (three and five failures, respectively).
Genotyping ADH1B by TaqMan PCR
Genomic DNA was extracted from peripheral blood using the QIAamp DNA Blood Kit (Qiagen, Hilden, Germany). Primer and hybridisation probes were designed with Primer Express. Sense primer 5′-CTCTTTATTCTGTAGATGGTGGCTGTAG-3′ and antisense primer 5′-GGGTCACCAGGTTGCCACTA-3′ were used to amplify a 76 bp fragment containing the G47A polymorphism of the ADH1B gene. Two minor-groove-binding (MGB) DNA probes were synthesised. The probe corresponding to the wild type (5′-FAM-TCTGTCGCACAGATG-MGB-3′) was labelled with 6-FAM, and the probe corresponding to the mutation (5′-VIC-AATCTGTCACACAGATGA-MGB-3′) was labelled with VIC at the 5′-end. The genotypes were analysed in software ‘Sequence Detector’ version 1.7 by procedure allelic discrimination after PCR.
Amplification was performed in a final volume of 25 μl containing 40 ng of DNA, 300 nM of each primer, 200 nM of each probe and 12.5 μl of TaqMan Universal PCR Master Mix (Perkin-Elmer, Weiterstadt, Germany).
In every assay, negative controls as well as controls for the wild type, mutant type and heterozygote were included. The PCR conditions were as follows: 2 min at 50°C plus 95°C for 10 min, followed by 40 cycles of denaturation at 92°C for 15 s, annealing and extension in one step at 60°C for 1 min. Genotyping was performed blinded to case–control status of the blood sample providers.
Statistical analysis
χ2 tests were used to assess deviation from Hardy–Weinberg equilibrium. Multivariate conditional logistic regression analysis with 5-year age strata was carried out using the PHREG procedure of the statistical software package SAS release 8.2 (SAS Institute, Cary, NC, USA).
In the multivariate model, we included several relevant variables influencing breast cancer risk (see Table 2). Variables that did not alter the estimates substantially, such as study region, body mass index, use of oral contraceptives and age at menarche, were not included in the analyses presented. Statistical interaction between ADH1B genotype and alcohol consumption was tested by using multiplicative interaction terms and evaluated by the likelihood ratio test.
Results
Selected characteristics of the study population are depicted in Table 1. In all, 65 breast cancer patients (10.6%) and 109 controls (10.1%) were heterozygous or homozygous carriers of the ADH1B*2 allele, corresponding to allele frequencies of 0.06 and 0.05, respectively. The distribution of ADH1B genotypes was in Hardy–Weinberg equilibrium (P=0.4 for cases and P=0.6 for controls).
We did not observe an association between ADH1B genotype and several risk factors, including first-degree family history of breast cancer, body mass index, parity, breastfeeding or smoking status (data not shown). However, alcohol consumption was found to differ significantly by ADH1B genotype among controls, with a mean average daily alcohol intake of 7.2 g (standard deviation (s.d.) 9.1) in women with ADH1B*1/*1 genotype and 5.8 g (s.d. 7.8) in carriers of the *2 allele (Wilcoxon's rank-sum test P=0.01). Results were virtually identical when all study subjects were considered (data not shown).
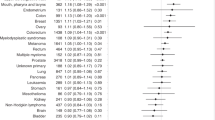
The analysis revealed no main effect of ADH1B genotype on breast cancer risk (adjusted OR for carriers of ADH1B*2 allele vs ADH1B*1/*1 genotype being 1.0, 95% confidence interval (CI) 0.7–1.4). However, multivariate analysis separately for carriers and noncarriers of the ADH1B*2 allele yielded differences in breast cancer risk associated with increasing levels of alcohol intake (Table 2). Among carriers of the *2 allele, there was a significant decreasing trend in breast cancer risk with increasing alcohol consumption (P-value for linear trend 0.04), although the odds ratio (OR) was significant only for the category of 12 g or more alcohol per day. In contrast, among women with ADH1B*1/*1 genotype, breast cancer risk increased with increasing alcohol consumption (P=0.03). The interaction between ADH1B genotype and alcohol intake was borderline statistically significant for the highest category of alcohol consumption (P=0.05) but not for low or moderate levels.
Discussion
Our data raise the possibility of an effect modification of the association between alcohol consumption and breast cancer risk by ADH1B genotype in our study population, which was apparent only at the highest consumption category of 12 g or more alcohol per day. We showed previously that breast cancer risk increased significantly with high daily alcohol intake of ⩾19 g in this study population (Kropp et al, 2001). Owing to the small number of ADH1B*2 carriers, we were not able to further subdivide the highest alcohol intake category of ⩾12 g day−1. Corresponding to a previous case-only study (Sturmer et al, 2002), a case-only analysis of our data would yield a statistically significant interaction OR (OR 0.2, 95% CI 0.1–0.6 for ⩾12 g alcohol day−1). However, since ADH1B genotype and alcohol intake are not independent in our study population, the modifying effect of the ADH1B genotype on breast cancer risk associated with alcohol consumption is overestimated in the case-only analysis, partly due to residual confounding by differences in alcohol consumption caused by the genotype (Albert et al, 2001). Indeed, indications for an association between ADH1B genotype and alcohol consumption, alcoholism or adverse reactions such as flushing were observed in previous studies (Whitfield et al, 1998; Borras et al, 2000; Loew et al, 2003; Neumark et al, 2004).
There is still controversy in the literature regarding the effect of ADH1B genotype on alcohol pharmacokinetics in vivo. Most studies failed to detect differences in blood alcohol or acetaldehyde levels by ADH1B genotype (Yamamoto et al, 1993; Mizoi et al, 1994; Whitfield et al, 2001); only one recent study reported a significantly higher alcohol elimination rate in carriers of the ADH1B*2 allele (Neumark et al, 2004).
The reduction in breast cancer risk associated with high consumption levels in carriers of the ADH1B*2 allele in our study could therefore be explained by a higher alcohol elimination rate in these subjects. Owing to the low allele frequency of the ADH1B*2 allele in Caucasians, our study had limited power to detect a gene–environment interaction for high alcohol consumption levels and our findings about ADH1B genotype as an effect modifier of breast cancer risk associated with high alcohol consumption need confirmation in larger studies.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Agarwal DP (2001) Genetic polymorphisms of alcohol metabolizing enzymes. Pathol Biol (Paris) 49: 703–709
Albert PS, Ratnasinghe D, Tangrea J, Wacholder S (2001) Limitations of the case-only design for identifying gene–environment interactions. Am J Epidemiol 154: 687–693
Borras E, Coutelle C, Rosell A, Fernandez-Muixi F, Broch M, Crosas B, Hjelmqvist L, Lorenzo A, Gutierrez C, Santos M, Szczepanek M, Heilig M, Quattrocchi P, Farres J, Vidal F, Richart C, Mach T, Bogdal J, Jornvall H, Seitz HK, Couzigou P, Pares X (2000) Genetic polymorphism of alcohol dehydrogenase in Europeans: the ADH2*2 allele decreases the risk for alcoholism and is associated with ADH3*1. Hepatology 31: 984–989
Bosron WF, Crabb DW, Li TK (1983) Relationship between kinetics of liver alcohol dehydrogenase and alcohol metabolism. Pharmacol Biochem Behav 18 (Suppl 1): 223–227
Brennan P, Lewis S, Hashibe M, Bell DA, Boffetta P, Bouchardy C, Caporaso N, Chen C, Coutelle C, Diehl SR, Hayes RB, Olshan AF, Schwartz SM, Sturgis EM, Wei Q, Zavras AI, Benhamou S (2004) Pooled analysis of alcohol dehydrogenase genotypes and head and neck cancer: a HuGE review. Am J Epidemiol 159: 1–16
Chang-Claude J, Eby N, Kiechle M, Bastert G, Becher H (2000) Breastfeeding and breast cancer risk by age 50 among women in Germany. Cancer Causes Control 11: 687–695
Collaborative Group on Hormonal Factors in Breast Cancer (2002) Alcohol, tobacco and breast cancer – collaborative reanalysis of individual data from 53 epidemiological studies, including 58, 515 women with breast cancer and 95, 067 women without the disease. Br J Cancer 87: 1234–1245
Eriksson CJ, Fukunaga T, Sarkola T, Chen WJ, Chen CC, Ju JM, Cheng AT, Yamamoto H, Kohlenberg-Muller K, Kimura M, Murayama M, Matsushita S, Kashima H, Higuchi S, Carr L, Viljoen D, Brooke L, Stewart T, Foroud T, Su J, Li TK, Whitfield JB (2001) Functional relevance of human adh polymorphism. Alcohol Clin Exp Res 25: 157S–163S
Kropp S, Becher H, Nieters A, Chang-Claude J (2001) Low-to-moderate alcohol consumption and breast cancer risk by age 50 years among women in Germany. Am J Epidemiol 154: 624–634
Loew M, Boeing H, Sturmer T, Brenner H (2003) Relation among alcohol dehydrogenase 2 polymorphism, alcohol consumption, and levels of gamma-glutamyltransferase. Alcohol 29: 131–135
Mizoi Y, Yamamoto K, Ueno Y, Fukunaga T, Harada S (1994) Involvement of genetic polymorphism of alcohol and aldehyde dehydrogenases in individual variation of alcohol metabolism. Alcohol 29: 707–710
Neumark YD, Friedlander Y, Durst R, Leitersdorf E, Jaffe D, Ramchandani VA, O'Connor S, Carr LG, Li TK (2004) Alcohol dehydrogenase polymorphisms influence alcohol-elimination rates in a male Jewish population. Alcohol Clin Exp Res 28: 10–14
Singletary KW, Gapstur SM (2001) Alcohol and breast cancer: review of epidemiologic and experimental evidence and potential mechanisms. JAMA 286: 2143–2151
Sturmer T, Wang-Gohrke S, Arndt V, Boeing H, Kong X, Kreienberg R, Brenner H (2002) Interaction between alcohol dehydrogenase II gene, alcohol consumption, and risk for breast cancer. Br J Cancer 87: 519–523
Triano EA, Slusher LB, Atkins TA, Beneski JT, Gestl SA, Zolfaghari R, Polavarapu R, Frauenhoffer E, Weisz J (2003) Class I alcohol dehydrogenase is highly expressed in normal human mammary epithelium but not in invasive breast cancer: implications for breast carcinogenesis. Cancer Res 63: 3092–3100
Whitfield JB, Nightingale BN, Bucholz KK, Madden PA, Heath AC, Martin NG (1998) ADH genotypes and alcohol use and dependence in Europeans. Alcohol Clin Exp Res 22: 1463–1469
Whitfield JB, Zhu G, Duffy DL, Birley AJ, Madden PA, Heath AC, Martin NG (2001) Variation in alcohol pharmacokinetics as a risk factor for alcohol dependence. Alcohol Clin Exp Res 25: 1257–1263
Yamamoto K, Ueno Y, Mizoi Y, Tatsuno Y (1993) Genetic polymorphism of alcohol and aldehyde dehydrogenase and the effects on alcohol metabolism. Arukoru Kenkyuto Yakubutsu Ison 28: 13–25
Acknowledgements
We wish to thank the many gynaecologists and oncologists of the 38 clinics of the study region; U Eilber for competent data management; M Schlaier and S Hees for technical assistance on genotyping. The epidemiologic study was supported by the Deutsche Krebshilfe and genotyping was funded by the Medical Faculty of the University of Ulm (P.685). C Lilla is recipient of a scholarship from the Deutsche Forschungsgemeinschaft (Graduiertenkolleg 793).
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Lilla, C., Koehler, T., Kropp, S. et al. Alcohol dehydrogenase 1B (ADH1B) genotype, alcohol consumption and breast cancer risk by age 50 years in a German case–control study. Br J Cancer 92, 2039–2041 (2005). https://doi.org/10.1038/sj.bjc.6602608
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602608
Keywords
This article is cited by
-
Loss of alcohol dehydrogenase 1B in cancer-associated fibroblasts: contribution to the increase of tumor-promoting IL-6 in colon cancer
British Journal of Cancer (2023)
-
The prognostic and clinical significance of IFI44L aberrant downregulation in patients with oral squamous cell carcinoma
BMC Cancer (2021)
-
Systems biology comprehensive analysis on breast cancer for identification of key gene modules and genes associated with TNM-based clinical stages
Scientific Reports (2020)
-
Role of aldehyde dehydrogenases, alcohol dehydrogenase 1B genotype, alcohol consumption, and their combination in breast cancer in East-Asian women
Scientific Reports (2020)
-
Alcohol Intake and Breast Cancer Risk: Weighing the Overall Evidence
Current Breast Cancer Reports (2013)