Abstract
We investigated a series of 122 cases of small cell lung carcinomas and non-small cell lung carcinomas for the presence of several viruses that are known to be oncogenic in humans. Thus, viral genomes (DNA) and/or RNA transcripts and/or proteins of human papillomaviruses (HPV) 16, 18, 31, 33, 51, Epstein–Barr virus (EBV), human herpesvirus 8 (HHV-8), human cytomegalovirus (HCMV) and simian virus 40 (SV40) were investigated on tissue sections (prepared in tissue microarrays) with different techniques of immunohistochemistry and in situ hybridisation. None of the cases displayed a single positive tumour cell for all the viruses tested whatever the technique applied. Of note, in five cases of tumours with lymphoid infiltrates, we detected scattered EBV (EBER)-positive bystander lymphocytes. In three cases, a faint nuclear staining was found with the anti-latent nuclear antigen/LANA1 (HHV-8) antibody. These cases were checked by PCR with two sets of primers (orf 26 and orf 75) and remained negative for this latter virus. Taken together, our data strongly suggest that the conventional human oncogenic viruses (HPV, EBV, HCMV, HHV-8 and SV40) are unlikely to play some role in the development of lung carcinomas.
Similar content being viewed by others
Main
A few virus species have been detected in human cancers. In some human tumours, these viruses probably play a critical role in carcinogenesis since they are present early during the process of cancer development and are constantly detectable in the tumour cells. Among these, human T-cell leukaemia virus-1 (HTLV-1) (Matsuoka, 2003), Epstein–Barr virus (EBV) (Macsween and Crawford, 2003), human herpesvirus-8 (HHV-8) (Ganem, 1997) and human papillomaviruses (HPV) (zur Hausen, 2000) are now well recognised as oncogenic and are specifically associated with different types of tumours. Other viruses have been incriminated in human carcinogenesis but there is still a hard debate regarding their direct implication in cancer, in particular concerning simian virus 40 (SV40) (Carbone et al, 2003) and human cytomegalovirus (HCMV) (Cobbs et al, 2002).
Large body of data have demonstrated the presence of SV40 in different tumours in humans, but the majority of the studies have relied on PCR detection of the viral genome (Bergsagel et al, 1992; Galateau-Salle et al, 1998; Martini et al, 1996). There are still controversies as to whether SV40 is directly linked to cancer development. Early studies have shown that SV40 genome was present in mesothelioma (Carbone et al, 1997), but immunodetection of SV40 as a diagnostic marker of human mesothelioma is not carried out in routine pathology (Carbone et al, 2003).
Recent results have implicated HCMV in the pathogenesis of malignant gliomas (Cobbs et al, 2002), prostate cancers (Samanta et al, 2003) and colon cancers (Harkins et al, 2002; Samanta et al, 2003). The human cytomegalovirus is a β-herpesvirus able to infect various types of human cells, including glial cells, endothelial cells and epithelial cells (Hummel and Abecassis, 2002). As other herpesviruses, HCMV infects 80% of the adult human population and persists in reservoir cells throughout life. Nevertheless, this virus is not yet recognised as an oncogenic factor, in particular in vivo (Hsu et al, 2004).
The epidemiology of lung cancers remains partially unresolved since the vast majority of tobacco users do not develop such tumours while at least 10–15% of lung cancers occur in non smokers (Alberg and Samet, 2003). Thus, factors other than smoking may also have an impact as aetiological and risk factors for lung cancer. Different studies have suggested that the HPVs (Syrjanen, 2002), EBV (Grinstein et al, 2002) and to a less extent SV40 (Galateau-Salle et al, 1998) may be involved in lung cancer development, but the results are discrepant or underline some geographical variations. A viral aetiology of lung tumours is tantalising since the virus can be regarded as a main oncogenic event (like HPV in genital tract) or as an important cofactor as in human mesotheliomas (SV40 plus asbestosis).
In this study, we tried to address the question of a viral aetiology of lung cancers by investigating a series of 122 cases of small cell lung carcinomas (SCLC) and non-small cell lung carcinomas (NSCLC) with immunohistochemistry and in situ hybridisation for the presence of five different virus species (HPV, EBV, HHV-8, SV40, HCMV).
Materials and methods
Tissue samples
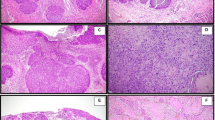
Two tissue microarrays (TMAs) were used for this study. The array blocks were constructed using a technique previously described (Charafe-Jauffret et al, 2003) with a tissue arrayer from Beecher Instruments (Beecher Instruments, Micro-array technology, Sun Prairie, WI, USA). Cores (0.6 mm) were taken from paraffin-embedded SCLC and NSCLC retrieved from our files at the Purpan Hospital in Toulouse between 1999 and 2002. Each tumour was represented by two cores. A total of 40 tumour samples were classified as squamous cell carcinoma (SCC), 31 as adenocarcinoma (AC), five as AC-SCC, four as large-cell lung cancer, nine as small-cell lung cancer, 13 as large-cell neuroendocrine carcinoma, seven as bronchioloalveolar carcinoma, three as atypical bronchial carcinoid, six as typical bronchial carcinoid and four as pleomorphic carcinoma.
The approval of the French equivalent of the Institutional Review Board (Comité Consultatif de Préservation des Personnes en Recherche Biologique/CCPPRB) was not required for such an investigation based on archived paraffin blocks that have been routinely used for diagnostic purposes.
Immunohistochemistry
Antibodies
Anti-CMV: We used an anti-HCMV monoclonal antibody (clone E13, Argene-Biosoft, Varihes, France). It recognises an immediate early antigen of HCMV (IE1) and does not cross react with EBV, adenovirus, varicella-zoster virus and HSV. It works very well in positive controls (working dilution 1 : 100) and gives a strong nuclear staining in tissues (colitis) with active HCMV infection. In addition, a weak cytoplasmic staining is seen in virtually all infected cells. The staining of the positive controls was obtained after standard antigen retrieval and/or after amplification of the signal by catalysed system amplification (CSA, Dako, Carpintera, CA, USA).
Anti-SV40: An anti-Tag antibody from Oncogene Research Products (San Diego, CA, USA) was used. This antibody (Ab-2, Clone Pab416) worked well on paraffin sections of tissues fixed either in 10% buffered formalin or in Bouin's liquid. The staining of the positive control cell line was obtained after standard antigen retrieval and/or after amplification of the signal by CSA. One hepatocellular carcinoma cell line from T-Ag transgenic mice (Weber-Benarous et al, 1993) and a case of renal infection (Li et al, 2002) were used as positive controls. For negative controls (DNA negative), five tissue sections from T-Ag PCR-negative lung tumours and non-neoplastic tissues were used.
Anti-HHV-8: The rat monoclonal anti-LANA-1 antibody (LN53) (ABI, Columbia, MD, USA) was used at a dilution of 1 : 2000 according to a previously published protocol (Brousset et al, 2001). This antibody stains latently infected HHV-8-positive cells (Kaposi's sarcoma) and the signal is nuclear with a stippling pattern.
Anti-EBV: Two monoclonal antibodies (anti-EBNA2, clone PE2, and anti-LMP1, clone CS1-4, Dako, Carpinteria, CA, USA) were used as described in detail elsewhere (Brousset et al, 1994). Lymphatic tissue from a patient with infectious mononucleosis was used as positive control.
Anti-HPV: We used the anti-VP1 capsid protein (clone K1H8) monoclonal antibody (Dako, Carpinteria, CA, USA). This antibody recognises a nonconformational internal linear epitope of the major capsid protein VP1. K1H8 antibody works well on paraffin section and in thin layers of cervical smears, and detects various types of viral strains (in particular, HPV type 6, 11, 16, 18, 31, 33, 42, 51, 52, 56 and 58) (Rouyer et al, 2004).
Immunohistochemical procedure
Immunostaining on paraffin sections was performed using the method described elsewhere with little modifications (Brousset et al, 2001). Briefly, paraffin sections were mounted on glass slides coated with silane (Sigma Chemical Co, Saint Quentin, France). Sections were deparaffinized, placed in 10 mmol L−1 Na-citrate buffer (pH 6) and heated in a microwave oven (Whirlpool model; Philips, Eindhoven, Holland) at 900 W for cycles of 20 min and 10 min. The slides were removed from the oven and allowed to cool for 30 min at room temperature. After washing in water, endogenous peroxidase was blocked with 1% hydrogen peroxide in methanol for 30 min. Slides were then rinsed in PBS before staining with a streptavidin–biotin three-stage technique, with the DAKO Strept ABC complex/HRP Duet kit (Dako, code no. K492, Carpinteria, CA, USA). In parallel, amplification with catalysed system amplification (CSA, Dako, Carpinteria, CA, USA) was applied according to the supplier's recommendations. The Dako CSA system HRP is an extremely sensitive immunohistochemical staining procedure incorporating a signal amplification method based on the peroxidase catalyzed deposition of a biotinylated compound followed by a secondary reaction with streptavidin peroxidase (Dako, Carpinteria, CA, USA).
In situ hybridisation
Human cytomegalovirus: This technique has been described elsewhere (Brousset et al, 1992). A biotinylated DNA probe from a commercial source (Enzo, PathoGene DNA probe assay, CMV DNA probe pack, part no. 32802, Enzo Life Sciences Inc., Faimingdale, NY, USA) was used according to the manufacter's recommendations with some modifications. In our hands, there was a clearcut correlation between in situ hybridisation and immunohistochemistry for control tissues.
Epstein–Barr virus: We used the peptidic nucleic acid (PNA) EBER1 probes from Dako (Carpinteria, CA, USA) according to the manufacturer's recommendations.
Human papillomavirus: Probes against strains 16-18-31-33-51 (from Enzo Life Sciences Inc., Faimingdale, NY, USA) were used and applied with the same procedure as for HCMV.
PCR
For PCR detection of HHV-8, amplification was performed with standard protocols with DNA extracted from formalin-fixed paraffin-embedded tissues. We chose the primer sets within orf 26 and orf 75 as previously described (Brousset et al, 2001). The other viruses were not tested since they are ubiquitous and detectable as bystanders in virtually all tissues tested.
Results
Immunohistochemistry
All the antibodies against the specific proteins of the five viruses tested in this study gave negative results in lung tumour tissues. All controls tested in the same conditions stained reproducibly. Two lymph nodes with infectious mononucleosis contained EBNA2 (PE2)- and LMP1 (CS1-4)-positive immunoblasts. Two lung biopsies from patients with active HCMV replication contained numerous IE1 (E13)-positive cells. Two cases of Kaposi's sarcoma and one case of multicentric Castleman's disease were repeatedly positive with anti-LNA1 antibody. Three cervical biopsies with condyloma were used as positive controls for anti-HPV (K1H8) antibody. Lastly, the two controls used to validate the anti-SV40 Tag antibody were positive in each experiment without using the amplification (CSA) technique.
None of the cases of lung cancer included in this study contained a single positive tumour cell with all the above-referenced antibodies. In three cases of SCC, we found a faint nuclear staining with the anti-LANA1 (HHV-8) antibody. This signal was weak and diffuse and lacked the characteristic stippling pattern. Nevertheless, the absence of viral infection was confirmed by PCR with two sets of primers (orf 26 and orf 75) (not shown).
In situ hybridisation
The results were very close to those of the immunohistochemistry in that no tumour cell was detected with any of the probes. Of note, in five cases with important lymphoid infiltrates (three AC, two SCC), a few scattered small bystander lymphocytes were detected with the EBER1 probes. We failed to detect a single positive case with the several anti-HPV probes we used.
Discussion
Besides some cases associated with HPV and rare cases infected by EBV, the incidence of viral infection in lung carcinomas remains marginal. We developed different techniques of detection of viruses already incriminated in lung tumours (HPV and EBV) and we extended our survey to viruses more recently implicated in cancer (SV40, HCMV and HHV-8). We have been unable to detect a single case (out of 122) positive for any of the five different viruses tested.
To be suspected to play some role in human tumours, an oncogenic virus should be specifically detected in the tumour cells. This theory also implies that the virus is present in all cells of a tumour in a monoclonal fashion, suggesting that the viral infection is an early event consistent with a clonal expansion of the tumour cells (Brousset et al, 1994) . In addition, a few viruses like EBV, HCMV and sometimes HPV are ubiquitous and infect a high percentage of people, rendering PCR investigations of the tumours poorly reliable as PCR products can be yielded from bystander infected cells. This is frequently the case with EBV (Meggetto et al, 1997) and also with HPV (Pett et al, 2004) and possibly SV40.
The detection rates of HPV in lung carcinomas are subject to wide variations. In a recent review of 85 studies recording about 2500 cases, Syrjanen (2002) described a detection rate varying from 0 to 100%. We failed to reproduce results obtained by other groups who used the same techniques as ours, that is, immunohistochemistry and in situ hybridisation. This discrepancy may be explained at least in part by geographical epidemiological variations since most studies with positive results for HPV were performed in Asia (Miyagi et al, 2000; Cheng et al, 2001). However, our results are also discrepant with those of the Finnish group of Syrjanen et al (1989), who found a detection rate of 7% for HPV among 131 patients with lung cancers. In order to clarify this difference, it may be useful to look for the presence of HPV in lung cancers of nonsmoking patients, where HPV could be found more frequently as cocarcinogen. In our study, only four out of 122 patients were nonsmokers.
Epstein–Barr virus probably plays a sporadic role in lung cancers (Grinstein et al, 2002). Only a few cases of EBV-associated tumours have been reported in the literature. We failed to detect EBV antigens in epithelial cells of our samples. EBV antigens were investigated with the anti-EBNA2 and anti-LMP1 antibodies because of a good sensibility and reproducibility of staining in control slides with an adapted technique of antigen retrieval. Moreover, the negativity of in situ hybridisation with EBER is the strongest argument for the absence of the latently infected cells in our tumours. Although our series is possibly biased since we had only two cases with lymphoepithelial architecture, we can deduce from our data that EBV is not at play in the most frequent types of lung cancers.
Simian virus 40 genome and gene products have been detected by some groups in mesotheliomas (Carbone et al, 2003). From an epidemiological point of view, variation in positivity between studies may be related to great geographical variation of SV40 contamination of people through poliomyelitis vaccination. Indeed, it is not possible to identify precisely individuals who were exposed to SV40, as few vaccine batches were tested for contamination, not all batches were contaminated and distribution of contaminated batches from one country to another was not controlled (Gazdar et al, 2002). Some authors have suggested that the viral genes, in particular Tag, were weakly expressed in mesotheliomas (Butel and Lednicky, 1999). However, immunodetection of SV40 Tag is not commonly recognised as a diagnostic marker enabling the distinction between mesothelioma and adenocarcinoma, or between mesothelioma and reactive mesothelial hyperplasia (Jasani, 1999). The lack of reproducibility of immunohistochemistry is difficult to explain since there are specific anti-Tag monoclonal antibodies that work well on paraffin sections making it possible the detection of the virus in physiological conditions. All of our cases have been tested in parallel with a highly sensitive amplification method of the immunohistochemical signal (CSA method), and a signal was obtained with the positive controls only. Galateau-Salle et al (1998) have reported the presence of SV40 DNA sequences in mesotheliomas and also in lung cancers and in benign (inflammatory) conditions as well. By immunohistochemistry, we have investigated four cases of SV40-positive lung tumours from this latter study and we obtained negative results in all instances (data not shown). Last but not least, Lopez-Rios et al recently published against a role for SV40 infection in human mesothelioma. In more than 70 mesothelioma samples, there lacked T-Ag-positive staining, such as in our experiments. The authors also performed DNA extraction and PCR, and found positive results only when primers were in the region of T-Ag gene (nucleotides 4100–4713) that is present in laboratory plasmids. Conversely, PCR were negative when primers were not included within that region (Lopez-Rios et al, 2004).
The negativity we found for HHV-8 is expected since so far this virus has not been associated with epithelial tumours. Human cytomegalovirus is not a good candidate in lung carcinogenesis as well. Indeed, one group only has reported on the detection of this virus in CNS tumours (Cobbs et al, 2002) and also in colonic (Harkins et al, 2002) and prostate cancers (Samanta et al, 2003). As far as the CNS tumours are concerned, we have been unable to reproduce the results of the study by Cobbs et al. We have found that the virus could be detected in only a few cases of CNS tumours not in malignant cells but rather in putative stromal cells (Sabatier et al, 2005; data not shown).
The major conclusion of our study is that the main oncogenic viruses usually found in solid tumours in humans are not implicated in the vast majority of lung carcinomas.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Alberg AJ, Samet JM (2003) Epidemiology of lung cancer. Chest 123: 21S–49S
Bergsagel DJ, Finegold MJ, Butel JS, Kupsky WJ, Garcea RL (1992) DNA sequences similar to those of simian virus 40 in ependymomas and choroid plexus tumors of childhood. N Engl J Med 326: 988–993
Brousset P, Butet V, Chittal S, Selves J, Delsol G (1992) Comparison of in situ hybridization using different nonisotopic probes for detection of Epstein–Barr virus in nasopharyngeal carcinoma and immunohistochemical correlation with anti-latent membrane protein antibody. Lab Invest 67: 457–464
Brousset P, Cesarman E, Meggetto F, Lamant L, Delsol G (2001) Colocalization of the viral interleukin-6 with latent nuclear antigen-1 of human herpesvirus-8 in endothelial spindle cells of Kaposi's sarcoma and lymphoid cells of multicentric Castleman's disease. Hum Pathol 32: 95–100
Brousset P, Schlaifer D, Meggetto F, Bachmann E, Rothenberger S, Pris J, Delsol G, Knecht H (1994) Persistence of the same viral strain in early and late relapses of Epstein–Barr virus-associated Hodgkin's disease. Blood 84: 2447–2451
Butel JS, Lednicky JA (1999) Cell and molecular biology of simian virus 40: implications for human infections and disease. J Natl Cancer Inst 91: 119–134
Carbone M, Pass HI, Miele L, Bocchetta M (2003) New developments about the association of SV40 with human mesothelioma. Oncogene 22: 5173–5180
Carbone M, Rizzo P, Grimley PM, Procopio A, Mew DJ, Shridhar V, de Bartolomeis A, Esposito V, Giuliano MT, Steinberg SM, Levine AS, Giordano A, Pass HI (1997) Simian virus-40 large-T antigen binds p53 in human mesotheliomas. Nat Med 3: 908–912
Charafe-Jauffret E, Bertucci F, Ramuz O, Devilard E, Gaulard P, Brousset P, Houlgatte R, Hassoun J, Birnbaum D, Xerri L (2003) Characterization of Hodgkin's lymphoma-like undifferentiated carcinoma of the nasopharyngeal type as a particular UCNT subtype mimicking Hodgkin's lymphoma. Int J Oncol 23: 97–103
Cheng YW, Chiou HL, Sheu GT, Hsieh LL, Chen JT, Chen CY, Su JM, Lee H (2001) The association of human papillomavirus 16/18 infection with lung cancer among nonsmoking Taiwanese women. Cancer Res 61: 2799–2803
Cobbs CS, Harkins L, Samanta M, Gillespie GY, Bharara S, King PH, Nabors LB, Cobbs CG, Britt WJ (2002) Human cytomegalovirus infection and expression in human malignant glioma. Cancer Res 62: 3347–3350
Galateau-Salle F, Bidet P, Iwatsubo Y, Gennetay E, Renier A, Letourneux M, Pairon JC, Moritz S, Brochard P, Jaurand MC, Freymuth F (1998) Detection of SV40-like DNA sequences in pleural mesothelioma, bronchopulmonary carcinoma and other pulmonary diseases. Dev Biol Stand 94: 147–152
Ganem D (1997) KSHV and Kaposi's sarcoma: the end of the beginning? Cell 91: 157–160
Gazdar AF, Butel JS, Carbone M (2002) SV40 and human tumours: myth, association or causality? Nat Rev Cancer 2: 957–964
Grinstein S, Preciado MV, Gattuso P, Chabay PA, Warren WH, De Matteo E, Gould VE (2002) Demonstration of Epstein-Barr virus in carcinomas of various sites. Cancer Res 62: 4876–4878
Harkins L, Volk AL, Samanta M, Mikolaenko I, Britt WJ, Bland KI, Cobbs CS (2002) Specific localisation of human cytomegalovirus nucleic acids and proteins in human colorectal cancer. Lancet 360: 1557–1563
Hsu CH, Chang MD, Tai KY, Yang YT, Wang PS, Chen CJ, Wang YH, Lee SC, Wu CW, Juan LJ (2004) HCMV IE2-mediated inhibition of HAT activity downregulates p53 function. EMBO J 23: 2269–2280
Hummel M, Abecassis MM (2002) A model for reactivation of CMV from latency. J Clin Virol 25 (Suppl 2): S123–S136
Jasani B (1999) Simian virus 40 and human pleural mesothelioma. Thorax 54: 750–751
Li RM, Mannon RB, Kleiner D, Tsokos M, Bynum M, Kirk AD, Kopp JB (2002) BK virus and SV40 co-infection in polyomavirus nephropathy. Transplantation 74: 1497–1504
Lopez-Rios F, Illei PB, Rusch V, Ladanyi M (2004) Evidence against a role for SV40 infection in human mesotheliomas and high risk of false-positive PCR results owing to presence of SV40 sequences in common laboratory plasmids. Lancet 364: 1157–1166
Macsween KF, Crawford DH (2003) Epstein–Barr virus-recent advances. Lancet Infect Dis 3: 131–140
Martini F, Iaccheri L, Lazzarin L, Carinci P, Corallini A, Gerosa M, Iuzzolino P, Barbanti-Brodano G, Tognon M (1996) SV40 early region and large T antigen in human brain tumors, peripheral blood cells, and sperm fluids from healthy individuals. Cancer Res 56: 4820–4825
Matsuoka M (2003) Human T-cell leukemia virus type I and adult T-cell leukemia. Oncogene 22: 5131–5140
Meggetto F, Brousset P, Selves J, Delsol G, Mariame B (1997) Reed–Sternberg cells and ‘bystander’ lymphocytes in lymph nodes affected by Hodgkin's disease are infected with different strains of Epstein–Barr virus. J Virol 71: 2547–2549
Miyagi J, Tsuhako K, Kinjo T, Iwamasa T, Hirayasu T (2000) Recent striking changes in histological differentiation and rate of human papillomavirus infection in squamous cell carcinoma of the lung in Okinawa, a subtropical island in southern Japan. J Clin Pathol 53: 676–684
Pett MR, Alazawi WO, Roberts I, Dowen S, Smith DI, Stanley MA, Coleman N (2004) Acquisition of high-level chromosomal instability is associated with integration of human papillomavirus type 16 in cervical keratinocytes. Cancer Res 64: 1359–1368
Rouyer N, Butet V, Brousset P (2004) Correlation of immunocytochemistry and hybrid capture for human papillomavirus detection in cervical smears. Diagn Cytopathol 31: 196–197
Sabatier J, Uro-Coste E, Pommepuy I, Labrousse F, Tremoulet M, Delisle MB, Brousset P (2005) Detection of human cytomegalovirus genome and gene products in central nervous system tumours. Br J Cancer (in press)
Samanta M, Harkins L, Klemm K, Britt WJ, Cobbs CS (2003) High prevalence of human cytomegalovirus in prostatic intraepithelial neoplasia and prostatic carcinoma. J Urol 170: 998–1002
Syrjanen K, Syrjanen S, Kellokoski J, Karja J, Mantyjarvi R (1989) Human papillomavirus (HPV) type 6 and 16 DNA sequences in bronchial squamous cell carcinomas demonstrated by in situ DNA hybridization. Lung 167: 33–42
Syrjanen KJ (2002) HPV infections and lung cancer. J Clin Pathol 55: 885–891
Weber-Benarous A, Decaux JF, Bennoun M, Allemand I, Briand P, Kahn A (1993) Retroviral infection of primary hepatocytes from normal mice and mice transgenic for SV40 large T antigen. Exp Cell Res 205: 91–100
zur Hausen H (2000) Papillomaviruses causing cancer: evasion from host-cell control in early events in carcinogenesis. J Natl Cancer Inst 92: 690–698
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by La Ligue contre le Cancer, Comité de la Haute-Garonne
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Brouchet, L., Valmary, S., Dahan, M. et al. Detection of oncogenic virus genomes and gene products in lung carcinoma. Br J Cancer 92, 743–746 (2005). https://doi.org/10.1038/sj.bjc.6602409
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6602409
Keywords
This article is cited by
-
Human papillomavirus and lung cancer: an overview and a meta-analysis
Journal of Cancer Research and Clinical Oncology (2019)
-
High seroprevalence of human herpesvirus type 8 infection in males with advanced lung carcinoma
Medical Microbiology and Immunology (2015)
-
Detection of Merkel cell polyomavirus with a tumour-specific signature in non-small cell lung cancer
British Journal of Cancer (2013)
-
Mouse mammary tumor virus-like gene sequences are present in lung patient specimens
Virology Journal (2011)
-
HPV in exhaled breath condensate of lung cancer patients
British Journal of Cancer (2011)