Abstract
In response to DNA damage, the cell cycle checkpoint kinase 2 (CHEK2) may phosphorylate p53, Cdc25A and Cdc25C, and regulate BRCA1 function, leading to cell cycle arrest and DNA repair. The truncating germline mutation CHEK2*1100delC abrogates kinase activity and confers low-penetrance susceptibility to breast cancer. We found CHEK2*1100delC in 0.5% of 190 oesophageal squamous cell carcinomas and in 1.5% of 196 oesophageal adenocarcinomas. In addition, we observed the mutation in 3.0% of 99 Barrett's metaplasias and 1.5% of 66 dysplastic Barrett's epithelia, both known precursor lesions of oesophageal adenocarcinoma. Since CHEK2*1100delC mutation frequencies did not significantly differ among oesophageal squamous cell carcinomas, adenocarcinomas and (dysplastic) Barrett's epithelia, as compared to healthy individuals, we conclude that the CHEK2*1100delC mutation has no major contribution in oesophageal carcinogenesis.
Similar content being viewed by others
Main
Oesophageal carcinoma is the ninth most common tumour type worldwide. Despite surgical intervention, 5-year overall survival is less than 20%, mainly due to the fact that patients often present with an advanced tumour stage. Alcohol and tobacco use are established risk factors for the development of oesophageal squamous cell carcinomas (Muir and McKinney, 1992). The presence of Barrett's oesophagus is the main risk factor for adenocarcinoma formation, being 30–125 times higher in patients with Barrett's oesophagus, as compared to the general population. Barrett's oesophagus is defined as a columnar cell metaplasia of the native distal oesophageal squamous cell epithelium (Spechler and Goyal, 1986), accompanied by the presence of Goblet cells, as a result of chronic gastro-oesophageal reflux. Barrett's metaplasia can progress to low- and high-grade dysplasia, and ultimately to invasive and metastasising adenocarcinoma. Patients with Barrett's oesophagus receive endoscopic surveillance to detect dysplasia and to diagnose carcinoma at an early and possibly treatable stage. The identification of genes that confer susceptibility for adenocarcinoma formation in Barrett's oesophagus would imply improved manageability of patients with Barrett's oesophagus. Familial cases of oesophageal cancer are however rare, and susceptibility genes for oesophageal cancer are thus unlikely to be found by linkage analysis. Consequently, screening of candidate susceptibility genes may be a more feasible approach for oesophageal cancer.
CHEK2 (also known as CHK2) is the mammalian homologue of Saccharomyces cerevisiae Rad53 and Schizosaccharomyces pombe Cds1 genes (Matsuoka et al, 1998; Chaturvedi et al, 1999). The CHEK2 gene, located on human chromosome 22q12, encodes a cell cycle checkpoint kinase that is implicated in DNA damage responses. Phosphorylation of the p53, Cdc25A and Cdc25C protein results in arrests in various phases of the cell cycle (Zhou and Elledge, 2000; Bartek et al, 2001). In addition, CHEK2 has been implicated in the regulation of DNA repair by the BRCA1 protein (Zhou and Elledge, 2000; Bartek et al, 2001). CHEK2*1100delC is a truncating germline variant of CHEK2 that abrogates kinase activity (Lee et al, 2001; Wu et al, 2001) and has initially been reported in families suffering from the Li–Fraumeni syndrome without p53 mutations (Bell et al, 1999). In familial gastric cancers, which are known to cluster in Li–Fraumeni families, germline CHEK2 mutations were absent (Kimura et al, 2000). In sporadic (osteo)sarcomas, lung cancers, breast cancers, ovarian cancers, colon cancers and haematopoietic neoplasms, CHEK2 was found to be rarely mutated (Bell et al, 1999; Haruki et al, 2000; Hofmann et al, 2001; Tavor et al, 2001; Aktas et al, 2002; Hangaishi et al, 2002; Ingvarsson et al, 2002; Miller et al, 2002). From recent publications, it appeared that the germline CHEK2*1100delC mutation in fact confers low-penetrance susceptibility to breast cancer (Meijers-Heijboer et al, 2002; Vahteristo et al, 2002). An increased frequency of CHEK2*1100delC was found among breast carcinoma families without BRCA1 or BRCA2 mutations, associated with an approximately two-fold increase of breast cancer risk in female carriers (Meijers-Heijboer et al, 2002).
The p53 protein is one of the downstream targets of CHEK2 kinase. Mutations of the p53 gene result in a variety of disturbances in growth control involving DNA replication, DNA repair and apoptosis. Like in breast carcinoma, mutations of the p53 gene appear to play an important role in the development of oesophageal squamous cell carcinoma, dysplastic Barrett's epithelium and the progression to oesophageal adenocarcinoma (Casson et al, 1991; Neshat et al, 1994; Wu et al, 1998). Ample studies have reported mutations in p53 in oesophageal carcinomas, with mutation frequencies varying from 40 to 90% (Jankowski et al, 1999; Mandard et al, 2000; Wijnhoven et al, 2001; Jenkins et al, 2002). As CHEK2 and p53 are thought to be participants of the same biological pathway, we aimed to establish whether CHEK2*1100delC confers susceptibility to oesophageal cancer, by determining the frequency of the mutation among an unselected series of oesophageal cancers and precursor lesions.
Materials and methods
Tissue specimens and controls
We investigated a cohort of 190 oesophageal squamous cell cancer patients, 196 oesophageal adenocarcinoma patients, 99 patients with Barrett's metaplasia and 66 patients with dysplastic Barrett's epithelium. Tissue samples were obtained from resection specimens (carcinomas) or endoscopic biopsies (Barrett's metaplasia and dysplasia), all derived from different patients. We microscopically confirmed that the endoscopic biopsy specimens did not exhibit any tumour cell invasion. Tissue fragments were digested from routine formalin-fixed, paraffin-embedded tissue blocks, without deparaffinisation, in 180 μl of 50mM l−1 Tris/HCl (pH=8.0), and 20 μl of Proteinase K (20 mg μl−1) was added. After overnight incubation at 56°C, the lysates were boiled for 10 min and subsequently centrifuged. The two series of Dutch control individuals consisted of: (A) 184 spouses of individuals heterozygous with respect to cystic fibrosis from the Southwest Netherlands, and (B) 460 individuals at ages 55 and older, ascertained through the Erasmus Rotterdam Health and the Elderly Study (ERGO) (Meijers-Heijboer et al, 2002).
Methods
Allele-specific oligonucleotide hybridisation assay
CHEK2 exon 10 was amplified using forward CHEK2 primer (5′-CAACATTATTCCCTTTTGTACTG-3′) and reverse CHEK2 primer (5′-GTTCCACATAAGGTTCTCATG-3′). DNA samples (1 μl) were subjected to PCR analysis in a total volume of 50 μl containing 1 × Promega buffer, 1.5 mM MgCl2-solution, 4 μ M dGTP, dTTP, dCTP and dATP, 3 U Taq DNA polymerase (Promega, Madison, USA), and 0.2 μg of forward and reverse CHEK2 primers. PCR amplification consisted of 35 cycles (95°C for 30 s, 55°C for 45 s and 72°C for 45 s), followed by a final extension at 72°C for 10 min. We detected the CHEK2*1100delC mutation by application of diluted PCR products to nylon filters and hybridisation under a high stringency of [32P]-labelled oligonucleotides complementary to CHEK2*1100delC and the wild-type sequence (5′-TTAGATTATGATTTTGGG-3′ and 5′-TTAGATTACTGATTTTGG-3′, respectively).
Polymorphic marker analysis
DNA was radioactively amplified essentially, as described above, using forward primer (5′-TAAGGTGGGAGGTTCACTTG-3′) and reverse primer (5′-ACCCATCCTCCTGCCTTAG-3′) for the D22S275 locus. PCR products were separated on a 6% polyacrylamide denaturing gel. After electrophoresis, gels were dried on blotting paper and exposed to X-ray films. Films were evaluated by visual inspection.
Immunohistochemistry
From formalin-fixed paraffin-embedded tissue blocks, 4-μm thick sections were mounted on 3-aminopropyl-triethoxysilane (APES)-coated glass slides. The sections were incubated with a mouse monoclonal antibody DCS 270.1 against the human CHEK2 protein (Novocastra Laboratories, Newcastle, UK; at a dilution of 1 : 50). Immunoreactivity was visualised by a standard avidin biotin immunoperoxidase technique, using a commercially available kit (Labvision, Fremont, USA) (Bartkova et al, 2001; Lukas et al, 2001).
Statistics
Differences of the CHEK2*1100delC mutation frequency between patients and controls were expressed in terms of odds ratios (OR) and 95% confidence intervals (95% CI), and tested with the χ2-test.
Results and discussion
We analysed tumour and biopsy samples obtained from 551 Dutch patients by a CHEK2*1100delC allele-specific oligonucleotide hybridisation assay. CHEK2*1100delC mutations were detected in 0.5% of 190 squamous cell carcinomas, 1.5% of 196 adenocarcinomas, 3.0% of 99 Barrett's metaplasias and in 1.5% of 66 dysplasias (Table 1). χ2 analysis revealed no significant differences between patient groups and the CHEK2*1100delC mutation frequency of 1.4% among 644 control individuals (P=0.94), and the odds ratio of the total patient group compared to the controls was 1.04 (95% CI 0.35–3.06, Table 1). These results suggest that CHEK2*1100delC does not substantially contribute to the development of oesophageal carcinoma. CHEK2*1100delC could still confer a three-fold risk, which is greater than the estimated two-fold risk associated with breast cancer, and CHEK2*1100delC thus may still be a low-penetrance susceptibility gene to oesophageal cancer. Given the low frequency of the mutation, however, even the maximal possible three-fold risk conferred by CHEK2*1100delC would only marginally contribute to the overall incidence of oesophageal cancer.
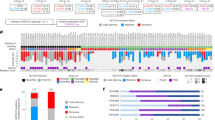
Examples of the hybridisation assay are shown in Figure 1. The median ages of patient groups at diagnosis were 59.6, range 14–86 years (Barrett's metaplasias), 60.3, range 32–84 years (dysplasias), 63.9, range 36–84 years (adenocarcinomas) and 60.9, range 31–79 years (squamous cell carcinomas). Ages at diagnosis of CHEK2*1100delC mutation carriers were 48, 73 and 77 years (Barrett's metaplasias), 59 years (dysplasia), 44, 50 and 63 years (adenocarcinomas) and 73 years (squamous cell carcinoma), which were not different from noncarriers and, again, not supporting a major role of CHEK2*1100delC in oesophageal cancer predisposition.
Allele-specific oligonucleotide hybridisation assay of 94 adenocarcinomas. Blot (A), hybridisation with wild-type oligonucleotide. Blot (B), hybridisation with mutant oligonucleotide. Adenocarcinoma samples T1, T2 and T3 are positive for the CHEK2*1100delC mutation, sample ‘+C’ represents a control individual with CHEK2*1100delC, and sample ‘−C’ represents a control individual negative for CHEK2*1100delC.
All mutations were confirmed and proven to be germline-derived by investigating patients' normal tissues. Only paraffin-embedded samples of tumour-negative lymph nodes were available, precluding confirmation of mutations by sequencing of long-range PCR products (Sodha et al, 2002). The CHEK2*1100delC germline mutation has, however, been found to be linked to one specific allele of the D22S275 polymorphic marker, that is located in intron 4 of CHEK2, which is present in 13% of the Dutch population (Meijers-Heijboer et al, 2002). All eight mutation-positive cases were demonstrated to carry the D22S275 allele linked to the CHEK2 mutation, which supports the detected mutations (Figure 2). Comparison of allele patterns in mutated tumours with their normal tissues revealed LOH in only one of the three informative carcinomas (T1 without LOH in Figure 2B, T4 with LOH in Figure 2C). LOH was also observed in three out of 14 informative nonmutated tumour samples. Limited data are, however, available on LOH of CHEK2 in tumours, and the possible tumour-suppressing role of CHEK2 therefore awaits further studies.
D22S275 polymorphic marker analysis in samples with CHEK2*1100delC. (A), the allele (arrow), known to be present in all carriers of CHEK2*1100delC (18), is present in all samples with the CHEK2*1100delC mutation (T1–T3 mutated adenocarcinoma samples, T4 mutated squamous cell carcinoma, D1 mutated dysplastic tissue, M1–M3 mutated metaplastic tissue), ‘+C’ represents a control individual with CHEK2*1100delC. (B, C), LOH patterns from two mutated tumours (T1 adenocarcinoma and T4 squamous cell carcinoma) compared with the corresponding normal tissues (N1 and N4) are shown. The arrowhead points to the deleted allele in T4.
Immunohistochemistry using monoclonal antibody DCS 270.1 on a series of mutated and nonmutated tumour tissues showed clear nuclear staining in all cases (Figure 3). Since the DCS 270.1 epitope lies within the N-terminus of CHEK2, staining of both wild-type and mutant protein may be expected. We observed no differences in CHEK2 protein levels, that is, neither lower intensity nor a lower percentage of CHEK2-positive cells, between CHEK2*1100delC mutated and nonmutated cancers. This was also true for the single-mutated tumour with LOH (T4 in Figure 3f), suggesting that a theoretical two-fold reduction in CHEK2 protein level cannot be detected by the applied immunohistochemistry method. This appears to contrast the results of Vahteristo et al, who reported loss of expression in three of the four CHEK2*1100delC tumours and reduction of CHEK2 protein expression in the fourth, using the same antibody (Vahteristo et al, 2002). Comparison of the two studies is, however, difficult, as they did not indicate the precise level of reduction in protein expression (Vahteristo et al, 2002). Since only few CHEK2*1100delC tumours have currently been reported, both the data of Vahteristo et al and the present data should be interpreted with caution.
CHEK2 protein expression. Nonmutated squamous cell carcinoma in (A), nonmutated adenocarcinoma in (B). The remaining samples are from the four mutated tumours: adenocarcinomas T1, T2 and T3 shown in (C–E), squamous cell carcinoma T4 shown in (F). Magnification × 100 (B, E), × 50 (A, C, D, F). Note the strong nuclear CHEK2 immunoreactivity in the tumour cells.
In summary, our study of a large and unselected series of Barrett's metaplasias and dysplasias, oesophageal adenocarcinomas and squamous cell carcinomas suggests that the germline CHEK2*1100delC mutation has no major contribution in oesophageal carcinogenesis.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Aktas D, Arno M, Rassool F, Mufti G (2002) Analysis of CHK2 in patients with myelodysplastic syndromes. Leuk Res 26: 985–987
Bartek J, Falck J, Lukas J (2001) CHK2 kinase–a busy messenger. Nat Rev Mol Cell Biol 2: 877–886
Bartkova J, Falck J, Rajpert-De Meyts E, Skakkebaek NE, Lukas J, Bartek J (2001) Chk2 tumour suppressor protein in human spermatogenesis and testicular germ-cell tumours. Oncogene 20: 5897–5902
Bell DW, Varley JM, Szydlo TE, Kang DH, Wahrer DC, Shannon KE, Lubratovich M, Verselis SJ, Isselbacher KJ, Fraumeni JF, Birch JM, Li FP, Garber JE, Haber DA (1999) Heterozygous germ line hCHK2 mutations in Li-Fraumeni syndrome. Science 286: 2528–2531
Casson AG, Mukhopadhyay T, Cleary KR, Ro JY, Levin B, Roth JA (1991) p53 gene mutations in Barrett's epithelium and esophageal cancer. Cancer Res 51: 4495–4499
Chaturvedi P, Eng WK, Zhu Y, Mattern MR, Mishra R, Hurle MR, Zhang X, Annan RS, Lu Q, Faucette LF, Scott GF, Li X, Carr SA, Johnson RK, Winkler JD, Zhou BB (1999) Mammalian Chk2 is a downstream effector of the ATM-dependent DNA damage checkpoint pathway. Oncogene 18: 4047–4054
Hangaishi A, Ogawa S, Qiao Y, Wang L, Hosoya N, Yuji K, Imai Y, Takeuchi K, Miyawaki S, Hirai H (2002) Mutations of Chk2 in primary hematopoietic neoplasms. Blood 99: 3075–3077
Haruki N, Saito H, Tatematsu Y, Konishi H, Harano T, Masuda A, Osada H, Fujii Y, Takahashi T (2000) Histological type-selective, tumor-predominant expression of a novel CHK1 isoform and infrequent in vivo somatic CHK2 mutation in small cell lung cancer. Cancer Res 60: 4689–4692
Hofmann WK, Miller CW, Tsukasaki K, Tavor S, Ikezoe T, Hoelzer D, Takeuchi S, Koeffler HP (2001) Mutation analysis of the DNA-damage checkpoint gene CHK2 in myelodysplastic syndromes and acute myeloid leukemias. Leuk Res 25: 333–338
Ingvarsson S, Sigbjornsdottir BI, Huiping C, Hafsteinsdottir SH, Ragnarsson G, Barkardottir RB, Arason A, Egilsson V, Bergthorsson JT (2002) Mutation analysis of the CHK2 gene in breast carcinoma and other cancers. Breast Cancer Res 4: R4
Jankowski JA, Wright NA, Meltzer SJ, Triadafilopoulos G, Geboes K, Casson AG, Kerr D, Young LS (1999) Molecular evolution of the metaplasia-dysplasia-adenocarcinoma sequence in the esophagus. Am J Pathol 154: 965–973
Jenkins GJ, Doak SH, Parry JM, D'Souza FR, Griffiths AP, Baxter JN (2002) Genetic pathways involved in the progression of Barrett's metaplasia to adenocarcinoma. Br J Surg 89: 824–837
Kimura K, Shinmura K, Yoshimura K, Shimizu K, Katai H, Beppu Y, Moriya H, Yokota J (2000) Absence of germline CHK2 mutations in familial gastric cancer. Jpn J Cancer Res 91: 875–879
Lee SB, Kim SH, Bell DW, Wahrer DC, Schiripo TA, Jorczak MM, Sgroi DC, Garber JE, Li FP, Nichols KE, Varley JM, Godwin AK, Shannon KM, Harlow E, Haber DA (2001) Destabilization of CHK2 by a missense mutation associated with Li-Fraumeni Syndrome. Cancer Res 61: 8062–8067
Lukas C, Bartkova J, Latella L, Falck J, Mailand N, Schroeder T, Sehested M, Lukas J, Bartek J (2001) DNA damage-activated kinase Chk2 is independent of proliferation or differentiation yet correlates with tissue biology. Cancer Res 61: 4990–4993
Mandard AM, Hainaut P, Hollstein M (2000) Genetic steps in the development of squamous cell carcinoma of the esophagus. Mutat Res 462: 335–342
Matsuoka S, Huang M, Elledge SJ (1998) Linkage of ATM to cell cycle regulation by the Chk2 protein kinase. Science 282: 1893–1897
Meijers-Heijboer H, van den Ouweland A, Klijn J, Wasielewski M, de Snoo A, Oldenburg R, Hollestelle A, Houben M, Crepin E, van Veghel-Plandsoen M, Elstrodt F, van Duijn C, Bartels C, Meijers C, Schutte M, McGuffog L, Thompson D, Easton D, Sodha N, Seal S, Barfoot R, Mangion J, Chang-Claude J, Eccles D, Eeles R, Evans DG, Houlston R, Murday V, Narod S, Peretz T, Peto J, Phelan C, Zhang HX, Szabo C, Devilee P, Goldgar D, Futreal PA, Nathanson KL, Weber B, Rahman N, Stratton MR (2002) Low-penetrance susceptibility to breast cancer due to CHEK2(*)1100delC in noncarriers of BRCA1 or BRCA2 mutations. Nat Genet 31: 55–59
Miller CW, Ikezoe T, Krug U, Hofmann WK, Tavor S, Vegesna V, Tsukasaki K, Takeuchi S, Koeffler HP (2002) Mutations of the CHK2 gene are found in some osteosarcomas, but are rare in breast, lung, and ovarian tumors. Genes Chromosomes Cancer 33: 17–21
Muir CS, McKinney PA (1992) Cancer of the oesophagus: a global overview. Eur J Cancer Prev 1: 259–264
Neshat K, Sanchez CA, Galipeau PC, Blount PL, Levine DS, Joslyn G, Reid BJ (1994) p53 mutations in Barrett's adenocarcinoma and high-grade dysplasia. Gastroenterology 106: 1589–1595
Sodha N, Houlston RS, Williams R, Yuille MA, Mangion J, Eeles RA (2002) A robust method for detecting CHK2/RAD53 mutations in genomic DNA. Hum Mutat 19: 173–177
Spechler SJ, Goyal RK (1986) Barrett's esophagus. N Engl J Med 315: 362–371
Tavor S, Takeuchi S, Tsukasaki K, Miller CW, Hofmann WK, Ikezoe T, Said JW, Koeffler HP (2001) Analysis of the CHK2 gene in lymphoid malignancies. Leuk Lymphoma 42: 517–520
Vahteristo P, Bartkova J, Eerola H, Syrjakoski K, Ojala S, Kilpivaara O, Tamminen A, Kononen J, Aittomaki K, Heikkila P, Holli K, Blomqvist C, Bartek J, Kallioniemi OP, Nevanlinna H (2002) A CHEK2 genetic variant contributing to a substantial fraction of familial breast cancer. Am J Hum Genet 71: 432–438
Wijnhoven BP, Tilanus HW, Dinjens WN (2001) Molecular biology of Barrett's adenocarcinoma. Ann Surg 233: 322–337
Wu TT, Watanabe T, Heitmiller R, Zahurak M, Forastiere AA, Hamilton SR (1998) Genetic alterations in Barrett esophagus and adenocarcinomas of the esophagus and esophagogastric junction region. Am J Pathol 153: 287–294
Wu X, Webster SR, Chen J (2001) Characterization of tumor-associated Chk2 mutations. J Biol Chem 276: 2971–2974
Zhou BB, Elledge SJ (2000) The DNA damage response: putting checkpoints in perspective. Nature 408: 433–439
Acknowledgements
We are grateful to Dr Anneke van der Wurff (Department of Pathology, Elisabeth Hospital Tilburg) for kindly providing biopsy samples, and to Dr Wim van Putten (Department of Statistics, Daniël den Hoed Cancer Clinic, Rotterdam) for statistical analyses. We wish to thank Marijke Wasielewski, Antoinette Hollestelle and Fons Elstrodt for technical assistance, Frieda van der Ham for performing immunohistochemistry and Frank van der Panne for photographic work.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Koppert, L., Schutte, M., Abbou, M. et al. The CHEK2*1100delC mutation has no major contribution in oesophageal carcinogenesis. Br J Cancer 90, 888–891 (2004). https://doi.org/10.1038/sj.bjc.6601551
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6601551
Keywords
This article is cited by
-
Variant allele of CHEK2 is associated with a decreased risk of esophageal cancer lymph node metastasis in a Chinese population
Molecular Biology Reports (2012)
-
CHK2 kinase: cancer susceptibility and cancer therapy – two sides of the same coin?
Nature Reviews Cancer (2007)