Abstract
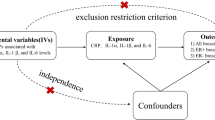
Serum and tissue levels of interleukin-6 (IL-6) have been implicated in the biological phenotype of breast carcinoma. A common G/C polymorphism at position −174 of the IL-6 promoter can influence the expression level of this gene. We therefore investigated for associations between this polymorphism and various phenotypic features in a series of 256 breast cancers. Individuals who were homozygous for the C allele (n=55) were more likely to have higher-grade tumours (P=0.039) with ductal histology (P=0.030) compared to those harbouring at least one wild-type G allele (n=201). Homozygosity for the C allele was also associated with significantly worse overall survival (P=0.031). We conclude that the −174 C allele of IL-6 is associated with a more aggressive breast cancer phenotype.
Similar content being viewed by others
Main
Interleukin-6 (IL-6) is a pleiotropic growth factor involved in many physiological and pathological processes including carcinogenesis (Ishihara and Hirano, 2002). High serum levels of IL-6 have been associated with advanced stage disease and worse prognosis for several cancer types including ovarian, breast and colorectal (Berek et al, 1991; Zhang and Adachi, 1999; Belluco et al, 2000; Bachelot et al, 2003). In contrast, however, high levels of IL-6 protein and mRNA expression within the breast carcinoma tissue have been linked to better prognosis and to a less malignant phenotype (Basolo et al, 1996; Fontanini et al, 1999; Karczewska et al, 2000).
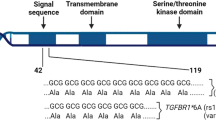
A common G/C polymorphism located within the IL-6 promoter at position −174 has been reported to influence IL-6 expression, with the G allele being associated with higher expression levels (Fishman et al, 1998; Terry et al, 2000; Vickers et al, 2002). This polymorphism has been implicated in a number of chronic disease conditions including arthritis, coronary heart disease and diabetes (Fishman et al, 1998; Fernandez-Real et al, 2000; Yudkin et al, 2000). In human cancer, the −174 G/C IL-6 polymorphism does not appear to be a risk factor for the development of multiple myeloma or melanoma (Zheng et al, 2000; Martinez-Escribano et al, 2002). Recent data, however, suggest that the C allele is associated with an increased risk of colorectal cancer (Landi et al, 2003). Furthermore, in ovarian cancer, the C allele is associated with an earlier stage of disease and with significantly better survival (Hefler et al, 2003). In light of the earlier studies linking serum and tissue IL-6 levels to breast cancer outcomes, the aim of the present study was to investigate for possible associations between the −174 G/C IL-6 polymorphism and phenotypic characteristics of breast cancer.
Materials and methods
Breast cancers
Consecutive cases of breast cancer treated surgically between 1992 and 1993 at the Sir Charles Gairdner or Royal Perth Hospitals in Perth, Australia, were selected for study. Genomic DNA was extracted from surgical specimens using standard techniques. The median age of patients at surgery was 59 years (range 18–93 years) and the median follow-up time was 57 months (range 2–96 months). Clinical and pathological features of this tumour series have been described earlier (Soong et al, 1997). Approximately 92% of node-positive and 23% of node-negative patients received some form of systemic adjuvant therapy. The majority of patients (>95%) were of European Caucasian descent. Successful genotyping of the −174 G/C IL-6 polymorphism was achieved for 256 cases. Of these, information on nodal status was unavailable for 61 cases, histological grade for 54 cases, histological type for 23 cases, tumour size for 27 cases, oestrogen and progesterone receptor status for five cases, ploidy for 98 cases, vascular invasion for 45 cases and erbB2 status for 25 cases. An institutional ethics committee approved the study.
Genotyping for the −174 G/C IL-6 polymorphism
Genotyping for the −174 G/C IL-6 polymorphism was carried out using a PCR-based fluorescence (F)-SSCP protocol, essentially as described earlier by our laboratory for other single-nucleotide polymorphisms (Powell et al, 2002; Grieu et al, 2004). HEX-labelled fluorescent primers (Geneworks, Australia) were designed to span the polymorphism and give rise to a PCR product of 165 bp in size. The forward primer sequence was 5′-AGGAAGAGTGGTTCTGCTTC-3′ and the reverse primer sequence 5′-CTTTGTTGGAGGGTGAGGGTG-3′. PCR was carried out in a volume of 15 μl comprising a mix of 1 × reaction buffer, 0.2 mM dioxynucleotide triphosphates, 2.5 mM MgCl2, 0.4 μ M of each primer and 0.3 U Taq polymerase (Qiagen, Australia). Samples were heated to 94°C before addition of DNA template 200 (200 ng). PCR comprised 10 min of denaturation at 94°C followed by 32 cycles of 45 s at 94°C, 45 s at the 64°C annealing temperature and 45 s at 72°C. Final extension was at 72°C for 5 min.
For F-SSCP, 2 μl of PCR product was mixed with 4 μl of deionised formamide-loading buffer and denatured at 94°C for 3 min. A volume of 1 μl of this mix was then loaded onto a nondenaturing 10% polyacrylamide gel and run on the Gel-Scan 2000 DNA fragment analyzer, according to the manufacturer's instructions (Corbett Research, Australia). The sample was pulse loaded for 20 s at 1200 V, the wells rinsed and the gel run for 90 min at 1200 V in 0.8 × TBE buffer at a constant temperature of 22°C. Sequencing of four DNA samples displaying homozygous banding patterns on F-SSCP gels was carried out in order to identify the three possible −174G/C IL-6 genotypes.
Statistical analysis
The χ2 test (Pearson statistic) was used to determine associations between the −174 G/C IL-6 polymorphism and various clinical and pathological features of the breast tumours. Kaplan–Meier analysis was used to assess the cumulative survival probabilities and differences were evaluated using the log-rank test. Cox regression was used in univariate survival analysis of various established prognostic factors and for the −174G/C IL-6 genotype. All P-values are derived from two-tailed statistical tests. Analyses were carried out using the SPSS statistical software package (Chicago, IL, USA).
Results
Three distinct banding patterns could be seen for the −174 G/C IL-6 polymorphism using the F-SSCP genotyping method (Figure 1). DNA sequencing identified these as CC homozygotes (pattern 1), GG homozygotes (pattern 3) and the GC heterozygote (pattern 2). Frequencies for the C and G alleles were 0.43 and 0.57, respectively, and were in Hardy–Weinberg equilibrium. The C allele frequency has previously been reported as 0.41 in a large (n=1109) community-based Australian study (Chapman et al, 2003), 0.43 in a UK study of 588 individuals (Vickers et al, 2002), 0.40 in another UK study of 383 healthy individuals (Fishman et al, 1998) and 0.43 in a study of 121 ovarian cancer patients from Austria (Hefler et al, 2003).
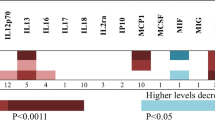
Tumours showing nonductal histology or well-differentiated morphology were significantly under-represented in patients who were homozygous for the C allele (Table 1). Only one out of 25 (4%) tumours with nonductal histology were found in CC homozygous patients compared to 47 out of 208 (23%) tumours with ductal histology (P=0.03). CC homozygous patients also showed trends for association with larger tumour size, low oestrogen receptor content, aneuploidy and amplified ErbB2 status, all of which are known features of poor prognosis. No associations were seen, however, with two other features of poor prognosis: positive nodal status and the presence of mutant p53.
Kaplan–Meier survival analysis revealed the IL-6 −174 CC genotype was associated with significantly worse overall survival compared to the GG or GC genotypes (P=0.031, Figure 2). The increased relative risk of death associated with homozygosity for the C allele was shown in univariate survival analysis to be 1.99 (95% confidence interval: 1.05–3.77; Table 2). The established features of nodal involvement, poor histological grade, large tumour size and ErbB2 amplification were all found to be associated with poor outcome in this tumour series (Table 2). Interestingly, the CC genotype was over-represented in patients whose tumours showed the three latter characteristics (Table 1). The CC genotype was not an independent factor for poor survival, however, in a multivariate model that included nodal status, histological grade, tumour size and ErbB2 amplification.
Discussion
Epithelial cells of the normal mammary gland constitutively produce several cytokines including IL-6 (Basolo et al, 1993). These have been proposed to play a role in the growth and differentiation of mammary epithelial tissue. The levels of IL-6 mRNA and protein are strongly reduced in invasive ductal carcinomas, suggesting an inverse relationship between tumour aggressiveness and the expression of this cytokine (Basolo et al, 1996; Fontanini et al, 1999; Karczewska et al, 2000). Since the common −174 G/C polymorphism has been linked to reduced production of IL-6 (Fishman et al, 1998), we hypothesised that this genetic variant may be associated with a more aggressive breast cancer phenotype.
We observed that homozygosity for the −174 C allele was significantly associated with poor histological grade and with ductal histology, and showed trends for association with larger tumour size and low oestrogen receptor content (Table 1). In keeping with this, CC homozygous patients also showed worse overall survival compared to the GC/GG patient group (Figure 2), although this was not independent of other established prognostic factors. Our results indirectly support the earlier observations of Basolo and co-workers, who showed that a low tumour level of IL-6 correlated with a more aggressive phenotype (Basolo et al, 1996; Fontanini et al, 1999). The C allele of the −174 G/C polymorphism has been shown to have lower IL-6 transcription rates and to be associated with lower expression levels compared to the G allele (Fishman et al, 1998; Terry et al, 2000; Vickers et al, 2002). This might explain our observation of an association between the CC genotype and a more aggressive breast cancer phenotype. Confirmation of this will require direct comparison between the −174 G/C genotype and tumour IL-6 expression levels.
At least two other studies have reported an association between low tissue expression of IL-6 and aggressive tumour behaviour (Gandour-Edwards et al, 1995; Basolo et al, 1998). Apart from the current study, however, there has been only one report of an association between the IL-6 −174 G/C polymorphism and tumour phenotype (Hefler et al, 2003). In contrast to the present results on breast cancer, these workers found that the C allele was associated with low stage and good prognosis in ovarian cancer patients. A possible explanation may be that IL-6 has different roles in carcinogenesis according to the tumour type.
Elevated serum levels of IL-6 have been associated with increased tumour burden and more advanced disease in several cancer types including colorectal (Belluco et al, 2000), ovarian (Berek et al, 1991) and breast (Zhang and Adachi, 1999; Bachelot et al, 2003). In a recent study of colorectal cancer, high serum IL-6 levels were linked to the −174 GG genotype, but only in patients with advanced disease (Belluco et al, 2003). It is therefore unclear whether elevated serum levels of IL-6 are a consequence of or a contributory cause to advanced tumour stage. Further prospective studies will be required to elucidate the relationships between the −174 G/C polymorphism, serum IL-6 levels, normal and tumour tissue IL-6 levels, and the biological phenotype for different cancers. It will also be interesting to determine whether the −174 C allele is a risk factor for breast cancer, as was shown recently for colorectal cancer (Landi et al, 2003).
We have previously shown significant associations in this breast tumour cohort between polymorphisms in the p53, p21 and luteinising hormone receptor genes and various phenotypic features including histological grade, steroid receptor level and tumour size (Powell et al, 2002,2003). The present results provide further evidence that genetic variants associated with known functional alterations can influence tumour phenotype.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Bachelot T, Ray-Coquard I, Menetrier-Caux C, Rastkha M, Duc A, Blay JY (2003) Prognostic value of serum levels of interleukin 6 and of serum and plasma levels of vascular endothelial growth factor in hormone-refractory metastatic breast cancer patients. Br J Cancer 88: 1721–1726
Basolo F, Conaldi PG, Fiore L, Calvo S, Toniolo A (1993) Normal breast epithelial cells produce interleukins 6 and 8 together with tumor-necrosis factor: defective IL6 expression in mammary carcinoma. Int J Cancer 55: 926–930
Basolo F, Fiore L, Fontanini G, Conaldi PG, Calvo S, Falcone V, Toniolo A (1996) Expression of and response to interleukin 6 (IL6) in human mammary tumors. Cancer Res 56: 3118–3122
Basolo F, Fiore L, Pollina L, Fontanini G, Conaldi PG, Toniolo A (1998) Reduced expression of interleukin 6 in undifferentiated thyroid carcinoma: in vitro and in vivo studies. Clin Cancer Res 4: 381–387
Belluco C, Nitti D, Frantz M, Toppan P, Basso D, Plebani M, Lise M, Jessup JM (2000) Interleukin-6 blood level is associated with circulating carcinoembryonic antigen and prognosis in patients with colorectal cancer. Ann Surg Oncol 7: 133–138
Belluco C, Olivieri F, Bonafe M, Giovagnetti S, Mammano E, Scalerta R, Ambrosi A, Franceschi C, Nitti D, Lise M (2003) −174 g>c polymorphism of interleukin 6 gene promoter affects interleukin 6 serum level in patients with colorectal cancer. Clin Cancer Res 9: 2173–2176
Berek JS, Chung C, Kaldi K, Watson JM, Knox RM, Martinez-Maza O (1991) Serum interleukin-6 levels correlate with disease status in patients with epithelial ovarian cancer. Am J Obstet Gynecol 164: 1038–1042
Chapman CM, Beilby JP, Humphries SE, Palmer LJ, Thompson PL, Hung J (2003) Association of an allelic variant of interleukin-6 with subclinical carotid atherosclerosis in an Australian community population. Eur Heart J 24: 1494–1499
Fernandez-Real JM, Broch M, Vendrell J, Gutierrez C, Casamitjana R, Pugeat M, Richart C, Ricart W (2000) Interleukin-6 gene polymorphism and insulin sensitivity. Diabetes 49: 517–520
Fishman D, Faulds G, Jeffery R, Mohamed-Ali V, Yudkin JS, Humphries S, Woo P (1998) The effect of novel polymorphisms in the interleukin-6 (IL-6) gene on IL-6 transcription and plasma IL-6 levels, and an association with systemic-onset juvenile chronic arthritis. J Clin Invest 102: 1369–1376
Fontanini G, Campani D, Roncella M, Cecchetti D, Calvo S, Toniolo A, Basolo F (1999) Expression of interleukin 6 (IL-6) correlates with oestrogen receptor in human breast carcinoma. Br J Cancer 80: 579–584
Gandour-Edwards R, Kapadia SB, Gumerlock PH, Barnes L (1995) Immunolocalization of interleukin-6 in salivary gland tumors. Hum Pathol 26: 501–503
Grieu F, Joseph D, Norman P, Iacopetta B (2004) Development of a rapid genotyping method for single nucleotide polymorphisms and its application in cancer studies. Oncol Rep, (in press)
Hefler LA, Grimm C, Ackermann S, Malur S, Radjabi-Rahat AR, Leodolter S, Beckmann MW, Zeillinger R, Koelbl H, Tempfer CB (2003) An interleukin-6 gene promoter polymorphism influences the biological phenotype of ovarian cancer. Cancer Res 63: 3066–3068
Ishihara K, Hirano T (2002) IL-6 in autoimmune disease and chronic inflammatory proliferative disease (review). Cytokine Growth Factor Rev 13: 357–368
Karczewska A, Nawrocki S, Breborowicz D, Filas V, Mackiewicz A (2000) Expression of interleukin-6, interleukin-6 receptor, and glycoprotein 130 correlates with good prognoses for patients with breast carcinoma. Cancer 88: 2061–2071
Landi S, Moreno V, Gioia-Patricola L, Guino E, Navarro M, de Oca J, Capella G, Canzian F, for the Bellvitge Colorectal Cancer Study Group (2003) Association of common polymorphisms in inflammatory genes Interleukin (IL)6, tumor necrosis factor alpha, NFKB1, and peroxisome proliferator-activated receptor delta with colorectal cancer. Cancer Res 63: 3560–3566
Martinez-Escribano JA, Moya-Quiles MR, Muro M, Montes-Ares O, Hernandez-Caselles T, Frias JF, Alvarez-Lopez MR (2002) Interleukin-10, interleukin-6 and interferon-gamma gene polymorphisms in melanoma patients. Melanoma Res 12: 465–469
Powell BL, Piersma D, Kevenaar ME, van Staveren IL, Themmen AP, Iacopetta B, Berns EM (2003) Luteinizing hormone signaling and breast cancer: polymorphisms and age of onset. J Clin Endocrinol Metab 88: 1653–1657
Powell BL, van Staveren IL, Roosken P, Grieu F, Berns EM, Iacopetta B (2002) Associations between common polymorphisms in TP53 and p21WAF1/Cip1 and phenotypic features of breast cancer. Carcinogenesis 23: 311–315
Soong R, Iacopetta BJ, Harvey JM, Sterrett GF, Dawkins HJ, Hahnel R, Robbins PD (1997) Detection of p53 gene mutation by rapid PCR-SSCP and its association with poor survival in breast cancer. Int J Cancer 74: 642–647
Terry CF, Loukaci V, Green FR (2000) Cooperative influence of genetic polymorphisms on interleukin 6 transcriptional regulation. J Biol Chem 275: 18138–18144
Vickers MA, Green FR, Terry C, Mayosi BM, Julier C, Lathrop M, Ratcliffe PJ, Watkins HC, Keavney B (2002) Genotype at a promoter polymorphism of the interleukin-6 gene is associated with baseline levels of plasma C-reactive protein. Cardiovasc Res 53: 1029–1034
Yudkin JS, Kumari M, Humphries SE, Mohamed-Ali V (2000) Inflammation, obesity, stress and coronary heart disease: is interleukin-6 the link? (review). Atherosclerosis 148: 209–214
Zhang GJ, Adachi I (1999) Serum interleukin-6 levels correlate to tumor progression and prognosis in metastatic breast carcinoma. Anticancer Res 19: 1427–1432
Zheng C, Huang DR, Bergenbrant S, Sundblad A, Osterborg A, Bjorkholm M, Holm G, Yi Q (2000) Interleukin 6, tumour necrosis factor alpha, interleukin-1-beta and interleukin-1 receptor antagonist promoter or coding gene polymorphisms in multiple myeloma. Br J Haematol 109: 39–45
Acknowledgements
The Gel-Scan 2000 instrument used in this work was purchased from a generous grant provided by the Lotteries Commission of Western Australia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Iacopetta, B., Grieu, F. & Joseph, D. The −174 G/C gene polymorphism in interleukin-6 is associated with an aggressive breast cancer phenotype. Br J Cancer 90, 419–422 (2004). https://doi.org/10.1038/sj.bjc.6601545
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6601545
Keywords
This article is cited by
-
STAT3 polymorphisms and IL-6 polymorphism are associated with the risk of basal cell carcinoma in patients from northern Poland
Archives of Dermatological Research (2019)
-
IL6 genotype, tumour ER-status, and treatment predicted disease-free survival in a prospective breast cancer cohort
BMC Cancer (2014)
-
Genetic modifiers of cancer risk in Lynch syndrome: a review
Familial Cancer (2013)
-
Genetic variation in proinflammatory cytokines IL6, IL6R, TNF-region, and TNFRSF1A and risk of breast cancer
Breast Cancer Research and Treatment (2011)
-
The −174 G/C Polymorphism in Interleukin-6 (IL-6) Promoter Region is Associated with Serum IL-6 and Carcinoembryonic Antigen Levels in Patients with Colorectal Cancers in Taiwan
Journal of Clinical Immunology (2010)