Abstract
Cancer survival in England and Wales has improved over the last 30 years. However, cohort survival estimates delay recognition of these improvements. Here we show that period survival estimates, based on survival in a recent time period, suggest a more optimistic pattern for England and Wales than cohort-based measures for most cancers.
Similar content being viewed by others
Main
Cancer survival in England and Wales has generally improved over the last 30 years. However, conventional survival estimates, based on following-up patient cohorts, delay identification of these improvements. Period analysis is a method of obtaining more up-to-date estimates of survival, calculated using only survival experience in a recent time period (Brenner and Gefeller, 1996). US and European data have shown these estimates to be good predictors of long-term survival (Brenner and Hakulinen, 2001; Brenner, 2002). Here cancer registry data are used to compare 5- and 10-year relative survival estimates for England and Wales using standard cohort methods and period analysis.
Materials and methods
Data were analysed from the public-use data set of all England and Wales registrations for 1 January 1981 to 31 December 1990 of the 26 most common cancers (Coleman et al, 1999) (followed until 31 December 1995). We present 5- and 10-year relative survival estimates for all ages using conventional cohort-based methods and period analyses. Results are presented for males and females combined, apart from results for prostate, testis and gynaecological cancers.
A cohort-based analysis is defined by the time interval in which patients are diagnosed. These patients (and only these) are followed up for 5 or 10 years and survival estimates are calculated. Here cohort estimates for 5 and 10 years are based on patients diagnosed between 1986–1990 and 1981–1985, respectively, and followed up until 1995 (see Table 1). In contrast, period analyses are defined by a recent time interval in which patients' survival experience is observed. It excludes short-term survival of patients diagnosed before the start of the period but includes their long-term survival within the period. Short-term survival of more recently diagnosed patients is included (see Brenner and Gefeller (1996)). Period estimates for 5 and 10 years are based on patients diagnosed between 1986–1990 and 1981–1990, respectively, but only include survival experience from 1990 to 1995 (Table 1).
Survival rates presented here are relative survival rates, adjusting for the general population background mortality. We calculated the expected survival using Hakulinen's (1982) method with 95% confidence intervals. A publicly available macro was used to calculate both cohort and period estimates (Brenner et al., 2002).
Results
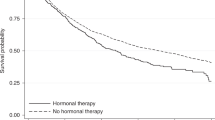
Table 2 shows that period estimates were higher than cohort estimates for 22 (85%) of the 26 cancers for 10-year survival and 18 (69%) of the 26 cancers for 5-year survival. This indicates recent changes in survival that are not detected by standard cohort analyses. At 10 years, period estimates exceeded cohort estimates by over 4% for colon, melanoma of the skin, breast, cervix, thyroid and Hodgkin's disease. Differences at 5 years were less marked but largest differences were seen for thyroid and Hodgkin's disease. Larger differences between cohort and period estimates were seen among cancers with better outcomes (10-year survival >50%). In contrast, where survival was poor (10-year survival <10%), differences between the estimates were smaller and for four of these six cancers, survival estimates were lower for period analysis.
Discussion
These results provide the most up-to-date estimates of cancer survival in England and Wales. Period survival estimates suggest a more optimistic pattern of cancer survival than cohort-based measures for the majority of cancers despite variations in survival. These differences appear greater for cancers with better outcomes. Our results show similar increases in survival estimates using period analysis as seen in the USA (Brenner, 2002), but with differing site-specific patterns.
Period estimates are similar to cohort estimates where cancer survival patterns have not changed over time. Where survival has changed, period estimates are more up-to-date. Cohort estimates are more influenced by short-term survival of patients diagnosed earlier in a study. If short-term survival changes over time, period analysis allows for these differences.
Since these data represent cancers diagnosed a decade ago, patterns of cancer survival are likely to have changed further. Period analyses of more recent data, when available, are likely to provide the earliest estimates of these developing patterns.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Brenner H (2002) Long-term survival rates of cancer patients achieved by the end of the 20th century: a period analysis. Lancet 360: 1131
Brenner H, Gefeller O (1996) An alternative approach to monitoring cancer patient survival. Cancer 78: 2004–2010
Brenner H, Gefeller O, Hakulinen T (2002) A computer program for period analysis of cancer patient survival. Eur J Cancer 38: 690–695
Brenner H, Hakulinen T (2001) Long-term cancer patient survival achieved by the end of the 20th century: most up-to-date estimates from the nationwide Finnish cancer registry. Br J Cancer 85: 367–371
Coleman MP, Babb P, Mayer D, Quinn MJ, Sloggett A (1999) Cancer survival trends in England and Wales, 1971–1995: deprivation and NHS Region (CDROM). London: Office for National Statistics
Hakulinen T (1982) Cancer survival corrected for heterogeneity in patient withdrawal. Biometrics 38: 933–942
Acknowledgements
Dr Smith is funded as an MRC/Trent Region training fellow in Health Services Research while undertaking this research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Smith, L., Lambert, P. & Jones, D. Up-to-date estimates of long-term cancer survival in England and Wales. Br J Cancer 89, 74–76 (2003). https://doi.org/10.1038/sj.bjc.6600976
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600976
Keywords
This article is cited by
-
Cancer patient survival in Sweden at the beginning of the third millennium – predictions using period analysis
Cancer Causes and Control (2004)
-
Recent increase in cancer survival according to age: higher survival in all age groups, but widening age gradient
Cancer Causes and Control (2004)
-
Combining cohort and period methods for retrospective time trend analyses of long-term cancer patient survival rates
British Journal of Cancer (2003)