Abstract
The clinical management of pancreatic disease is often hampered by a lack of tissue diagnosis. Endoscopic pancreatography offers the opportunity to investigate exfoliated cells. However, the significance of mere cytological investigation is compromised by an insufficient sensitivity. The evaluation of the molecular background of carcinogenesis hopefully is capable of providing more sensitive diagnostic markers. The p16INK4a-/retinoblastoma tumour-suppressive pathway has been shown to be involved in the development of near to all pancreatic neoplasms. p14ARF is another tumour suppressor located in the immediate neighbourhood of p16INK4a. Promoter methylation has been demonstrated to be a major inactivating mechanism of both genes. We sought to further evaluate the role of the gene locus INK4a methylation status in the endoscopic differentiation of chronic inflammatory and neoplastic pancreatic disease. Pancreatic fluid specimens of 61 patients with either pancreatic carcinoma (PCA: 39), chronic pancreatitis (CP: 16) or a normal pancreatogram (NAD: 6) were retrieved. In order to detect methylation of either the p14ARF or the p16INK4a promoter a methylation-specific PCR protocol was applied. While 19 out of 39 patients with PCA showed p16 promoter methylation (49%), none of the 16 patients with CP revealed p16 promoter methylation. p14ARF methylation was found in a lower percentage of PCA specimens and in none of the samples of patients with CP. These results suggest a specific significance of INK4a for the development of malignant pancreatic disease. Our data further indicate a potential role for INK4a methylation as a diagnostic marker in the endoscopic differentiation of benign and malignant pancreatic disease.
Similar content being viewed by others
Main
The diagnosis of pancreatic cancer in time for cure is still difficult. Clinical symptoms generally only occur in advanced stages of the disease, while no efficient screening tests are available. Furthermore, malignant and benign diseases of the pancreas are difficult to distinguish by even sophisticated imaging procedures or biochemical means requiring surgical diagnosis in a substantial portion of cases. Thus, the prognosis of pancreatic cancer, in spite of improvements, is still fatal, with less than 5% of patients surviving more than 5 years (Niederhuber et al, 1995; Parker et al, 1996).
Pancreatic carcinoma being a ductal disease, sheddering tumour cells with physiological pancreatic secretions into the accessible duodenum has inspired cytology-based diagnostic concepts for decades (Lemon and Byrnes, 1949; Gibbs, 1963). Retrograde pancreatography by a duodenoscope for the first time offered the opportunity to obtain directly ductal juice and to achieve tissue diagnosis in pancreatic disease in a minimal invasive manner (Endo et al, 1974; Hatfield et al, 1976). A multitude of studies have demonstrated that the joint application of endoscopy and cytotechniques has the capability to contribute to an improved clinical management (Tatsuta et al, 1983; Venu et al, 1990; Ryan, 1991; Nakaizumi et al, 1995; Enayati et al, 1996). However, while being characterised by a near 100% specificity, the sensitivity of pancreatic juice cytology proved to be unsatisfying because of an often low cell count or cell disintegration (Ferrari et al, 1994).
Hence, there is a considerable interest in molecular markers that might complement conventional cytotechniques. The demands a molecular candidate marker had to meet were (1) a high prevalence in the tumour under investigation, (2) a high specificity for malignant disease and (3) the methodological possibility to detect reliably those alterations in routinely obtained fluid specimens.
In pancreatic cancer, point mutations of the k-ras oncogene have been shown with a prevalence of up to 90% (Almoguera et al, 1988; Hruban et al, 1993; Urban et al, 1993). Several studies have demonstrated the possibility to detect these mutations in pancreatic juice specimens or duodenal fluid (Tada et al, 1993; Trümper et al, 1994; Berthelemy et al, 1995; Van Laethem et al, 1995). However, further work revealed that k-ras mutations are also associated with benign or precancerous ductal lesions of unclear prognostic significance, thus limiting the clinical significance of detected k-ras mutations (Yanagisawa et al, 1993; Tada et al, 1996; Furuya et al, 1997).
Most human cancer cells are characterised by a disruption of p53- and Rb-tumour suppressive pathways (Sherr, 1996). The uniquely organised ARF/INK4a locus on chromosome 9p harbours two distinct genes, p14ARF and p16INK4a, each one encoding a key member of both pathways, respectively (Chin et al, 1998). Both genes share a common exon, but are under the control of their own specific promoters. The first exon of p14ARF, designated as exon 1β, is located approximately 23 kb upstream of the first exon 1α of p16INK4a (Quelle et al, 1995; Kamijo et al, 1997). In a variety of human malignancies, p16INK4a alterations apparently are a major cause of Rb pathway impairment. The p16INK4a tumour suppressor gene encodes a cyclin-dependent kinase inhibitor, preferentially binding to CDK4 and CDK6, preventing the coupling of those kinases with d-type cyclins and thus the activating phosphorylation of Rb. Therefore, the functional impairment of p16INK4a is suggested to lead to uncontrolled cell cycle progression and neoplastic transformation (Sherr, 1996; Chin et al, 1998). p14ARF, on the other hand, by accumulating evidence is suggested to act as a tumour suppressor by neutralising MDM2-mediated degradation of p53 (Pomerantz et al, 1998; Stott et al, 1998; Zhang et al, 1998). For pancreatic carcinoma, it has been reported that the Rb tumour-suppressive pathway is abrogated in near to all studied cases and that this disruption is caused exclusively by inactivation of the p16INK4a gene. Herein, aberrant promoter methylation proved to be a major inactivating mechanism (Schutte et al, 1997). While de novo promoter methylation of p14ARF has been reported to occur in some gastrointestinal malignancies like stomach and colorectal cancer and precancerous conditions (Barrett et al, 1996; Hsieh et al, 1998; Klump et al, 1998; Esteller et al, 2000; Song et al, 2000; Iida et al, 2000), only a few data exist regarding the situation in pancreatic adenocarcinoma.
The present study sought to further evaluate the significance of aberrant p16INK4a and p14ARF promoter methylation as detected in endoscopically obtained fluid specimens in the differential diagnosis of pancreatic disease. Pancreatic or biliary fluid samples of patients with chronic pancreatitis, pancreatic cancer or missing alterations were analysed with respect to the methylation status of the ARF/INK4a locus in order to define the prevalence and specificity of those epigenetic alterations.
Patients and methods
Patients and specimens
In all, 57 patients in four endoscopic units, who were routinely investigated by endoscopic retrograde cholangiopancreatography (ERCP), were enrolled into this study (37 pancreatic carcinoma (PCA), 14 chronic pancreatitis (CP), six nothing abnormal detected (NAD)). The study was approved by the local ethical committees. The median age of patients with PCA and CP was 70.2 years (39–90 years) and 51.6 years (23–74 years), respectively. The individual diagnosis of pancreatic disease was based on unequivocal histological, biochemical, radiological results and the immediate clinical course. Owing to the often mere palliative treatment of patients with pancreatic adenocarcinoma tissue diagnosis was not available in 18 patients diagnosed to have pancreatic cancer. If a malignant disease other than of pancreatic origin could not definitely be ruled out, samples were excluded from further molecular analysis. Since no standardised protocol in regard to cytological diagnosis was applied and some patients already had a confirmed diagnosis of malignancy when endoscopy was performed, aspirates for cytology were not retrieved in all patients. Thus, malignancy was confirmed in just four patients by cytology. Investigators were asked to try to cannulate the pancreatic duct and aspire pancreatic fluid; in case of technical difficulties it was allowed to either aspire secretions from the Ampulla vateri or—in the case of a supposed infiltration–of the common bile duct. After wire-guided cannulation of the pancreatic duct, between 1 and 3 ml of pancreatic secretion was aspirated. No stimulation by intravenous administration of secretin was performed. No standardised strategy with regard to the exact localisation of the catheter tip was followed. In a few cases, pancreatic fluid was aspired through a prior inserted external drainage of the major pancreatic duct. Immediately after aspiration, obtained specimens were stored without any further processing at −20°C. Additionally, 12 tissue specimens of pancreatic cancer were included. In some patients who were submitted to surgery or had diagnostic biopsy archival tissue specimens, both pancreatic secretions and tissue specimens were analysed.
DNA extraction
Genomic DNA was extracted from thawed specimens. A volume of 1 ml of secretion was digested for 3 days at 55°C using a proteinase K/sodium dodecyl sulphate (SDS) solution. DNA was extracted using the conventional phenol/chloroform method.
Methylation-specific PCR amplification
A slight modification of the protocol suggested by Herman et al (1996) has been implemented. In brief, DNA modification by bisulphite converts exclusively unmethylated cytosines to uracil. Subsequent PCR amplification with primers specific for unmethylated vs methylated DNA reveals the methylation status of investigated DNA sections. Initially, 1 μg of DNA was denatured in a volume of 50 μl (final NaOH concentration 0.2 M) for 20 min at 37°C. A total of 30 μl hydroquinone (Sigma, Deisenhofen, Germany) (10 mM) and 520 μl of 3 M sodium bisulphite (Sigma, Deisenhofen, Germany) at pH 5.5 were added and mixed. Samples were incubated at 55°C for 21 h. Modified DNA was purified using a commercially available PCR-Purification Kit according to the manufacturer's recommendations (Qiagen, Hilden, Germany). Finally, a second NaOH treatment was performed (20 min, room temperature, final concentration 0.3 M). Modified and purified DNA was precipitated by ethanol for 12 h and resuspended in 100 μl of water. Primer pairs for PCR amplification are given in Table 1 and were purchased (MWG-Biotech, Ebersberg, Germany). A volume of 100 μl PCR mixtures contained 10 μl buffer (10 mM Tris-HCl, 50 mM KCl, 0.1% Triton X-100), 1 μl of MgCl2, 1.5 μl of dNTPs (1.25 mM), primers, 2 U of Taq polymerase (PAN-Systems, Aidenbach, Germany), and 0.1 μg of DNA. Amplification was performed in a thermal cycler (Biometra, Göttingen, Germany) for 35 cycles (95°C/5 min, annealing temperature/90 s, 72°C/60 s) and concluded by a final 8 min extension at 72°C. A control without the addition of DNA was performed for each PCR set. A volume of 20 μl of PCR product was loaded onto nondenaturing polyacrylamide gels (8%) and visualised by silver staining. A methylation was confirmed if at least two experiments had demonstrated an unequivocal amplification product of methylation-specific PCR. Around 10 consecutive specimens were analysed as common slots without clinical information on singular specimens.
Statistical analysis
The association of p16INK4a and p14ARF promoter methylation in malignant vs nonmalignant pancreatic disease and patients with a normal pancreatogram was tested by χ2 test and Yates' correction.
Results
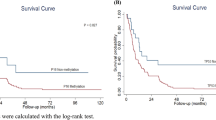
p16-promoter methylation
In total, 43.2% of specimens obtained from patients with pancreatic carcinoma revealed p16 promoter methylation (16 out of 37). However, none out of 16 specimens obtained from patients with chronic pancreatitis (n=14) or missing alterations (n=6) showed p16 promoter methylation. Thus, a sensitivity of 43.2% and a specificity of 100% in regard to the detection of malignancy has been found for p16 promoter methylation (Figure 1, Table 2 and Table 3).
p14-promoter methylation
Methylation of the p14 promoter was detected in 20.6% of specimens of patients with pancreatic carcinoma (seven out of 34). Promoter methylation of p14ARF could neither be detected in specimens obtained from patients with chronic pancreatitis nor in those samples from patients with missing alterations. Thus, a sensitivity of 20.6% and a specificity of 100% in regard to the detection of malignancy has been shown for p14 promoter methylation (Figure 1, Table 2 and Table 3).
Relation of p14 and p16 promoter methylation
A simultaneous promoter methylation of p14ARF and p16INK4a was seen in 14.7% of the specimens from patients with pancreatic carcinoma. A simultaneous methylation of the adjacent p14ARF promoter was seen in 22% of those specimens with positive p16INK4a methylation (Table 2). An exclusive methylation of either the p16INK4a or the p14ARF promoter region was observed in 72 and 43% of methylation-positive carcinoma specimens, respectively.
Discussion
Molecular approaches keep the promise of complementing cytotechniques in the noninvasive diagnosis of pancreaticobiliary disease. The potential sensitivity of any molecular alteration, however, is defined by its prevalence in pancreatic cancer, its specificity for malignant alterations and the technical options to detect it reliably.
The methodological success of PCR-based approaches towards the molecular analysis of pancreatic fluids is limited by polymerase inhibitors. Like other groups, we observed the frequent failure of PCR analysis in pilot studies (Saurin et al, 2000). In our experience, it is essential to find out the least possible amount of DNA allowing PCR amplification. However, our preliminary studies revealed that methylation analysis, even though requiring additional processing steps and being a gradual process, is even more reproducible in endoscopically obtained secretions than mutational screening assays as PCR-SSCP or PCR-RFLP. The present study is the first to demonstrate the diagnostic potential of INK4a methylation in pancreatic secretions obtained during routine endoscopic retrograde pancreatography. Methylation status of both the p14ARF and the p16INK4a promoter was successfully assessed in all samples enclosed. Surprisingly, unlike the results of a previous preliminary analysis, the localisation of the catheter tip did not influence the prevalence of detected methylation. We speculate that exfoliated cells were not only present in the pancreatic duct or Ampulla vateri, but also in the common bile duct due to an infiltration of the biliary system with a ‘double duct sign’ detectable in most cases. However, it is to be assumed that due to a very small number of patients in our study a difference in technical approaches towards aspiration of secretions was missed.
Interestingly, the methylation rates detected in tissue proved to be somewhat lower than those detected in endoscopically retrieved pancreatic secretions. While it seems intriguing to speculate on whether fluid samples retrieved from the pancreatic duct might be even more representative than tissue slices from tumour blocks, it has to be taken into consideration that (1) the numbers of patients in whom tissue could be analysed were small and (2) no standardised protocol in regard to the retrieval and storage of tissue specimens was followed; detected methylation rates could be lower due to degradation of DNA and/or contamination with benign ductal or stromal cells in archival paraffin blocks.
De novo p16INK4a promoter methylation was detected in 43.2% of specimens from patients with pancreatic carcinoma. These data parallel those recently reported by Schutte et al (1997), who detected p16INK4a promoter methylation in six out of 17 primary pancreatic carcinoma specimens or pancreatic carcinoma cell lines (35%). Similarly, a prevalence of p16INK4a methylation of 38% has recently been reported by Esteller et al (2001). In this context, it needs to be emphasised that exclusively exocrine pancreatic adenocarcinomas of ductal origin have been included. A recent study published by Moore et al (2001) has addressed p16 alterations in primary neoplasms of the pancreas, and these data have shown that in exocrine and endocrine tumourigenesis of the pancreas different molecular pathways may be involved.
The situation for p14ARF is more controversial. As far as we know, up to this end the only data regarding the role of p14ARF in pancreatic carcinoma have been published also by Esteller et al (2000): in none out of 20 randomly selected pancreatic carcinomas p14ARF promoter methylation was detected. This is in apparent contrast to our findings, showing a prevalence of at least 20.6% in 36 pancreatic fluid specimens. While it is well recognised that promoter methylation is a gradual process, our results could reflect a weak methylation of unknown functional significance. In addition, a ‘background level of methylation’ had also been reported by Schutte et al (1997) in normal duodenal tissue. Moreover, there is an ongoing controversy as to whether age-related methylation possibly may also involve promoter regions of tumour-suppressive genes. It is to be acknowledged that patients with pancreatic carcinoma tend to be older than patients with chronic pancreatitis. Thus, a contribution of age-related methylation may not be ruled out when higher rates of promoter methylation are detected in neoplasms. And indeed in this study, for p16 promoter methylation a lower frequency in patients 63 years and younger was detected, while patients of 80 years and older revealed a methylated promoter more frequently than the group as a whole. However, for p14 methylation in older patients an even lower frequency of methylation was detected (data not shown).
Taken together, at the moment it may be postulated that p14ARF promoter methylation is at least rarer than p16INK4a methylation in pancreatic carcinoma and that further evaluation of p14ARF's exact role in the development and course of pancreatic carcinoma requires further studies in greater patient cohorts, bringing together methylation data with functional findings.
In none of the specimens obtained from patients with chronic pancreatitis, either p16INK4a or p14ARF promoter methylation was detected in this study. This further supports the results of our own previous work and the data reported by others indicating that the tumour-suppressive function of p16INK4a is exclusively abrogated in (pre-)neoplastic but not in merely inflammatory or hyperproliferative conditions (Barrett et al, 1996; Hsieh et al, 1998; Klump et al, 1998). However, it is well recognised from epidemiological and histopathological studies that chronic pancreatitis may predispose for the development of pancreatic cancer. Thus, the prevalence of INK4a methylation in preneoplastic ductal lesions requires further evaluation. For pancreatic disease our findings are in fortunate contrast to the situation found for k-ras mutations and suggest the further evaluation of INK4a methylation in the management of unclear pancreatic disease.
Taken together, our findings for the first time demonstrate the technical feasibility to detect INK4a's methylation in pancreatic secretions. Moreover, the high prevalence of p16INK4a methylation found in pancreatic carcinoma tissues is confirmed by these data. INK4a methylation revealed a 100% specificity for malignant pancreatic disease in this study. p14ARF methylation apparently is of subordinate significance in pancreatic carcinoma while its exact role needs to be further evaluated.
We would conclude, therefore, that INK4a methylation is a promising candidate marker for the endoscopic differential diagnosis of malignant and benign pancreatic disease.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Almoguera C, Shibata D, Forrester K, Martin J, Arnheim N, Perucho M (1988) Most human carcinomas of the exocrine pancreas contain mutant c-K-ras genes. Cell 53: 549–554
Barrett MT, Sanchez CA, Galipeau PC, Neshat K, Emond M, Reid BJ (1996) Allelic loss of 9p21 and mutation of the CDKN2/p16 gene develop as early lesions during neoplastic progression in Barrett's esophagus. Oncogene 13: 1867–1873
Berthelemy P, Boisson M, Escourrou J, Vaysse N, Rumeau JL, Pradayrol L (1995) Identification of K-ras mutations in pancreatic juice in the early diagnosis of pancreatic cancer. Ann Intern Med 123: 188–191
Chin L, Pomerantz J, DePinho RA (1998) The INK4a/ARF tumour suppressor: one gene–two products–two pathways. Trends Biochem Sci 23: 291–296
Enayati PG, Traverso LW, Galagan K, Thirlby RC, Larson J, Hauptman EM, Kozarek RA (1996) The meaning of equivocal pancreatic cytology in patients thought to have pancreatic cancer. Am J Surg 171: 525–528
Endo Y, Morii T, Tamura H, Okuda S (1974) Cytodiagnosis of pancreatic malignant tumours by aspiration, under direct vision, using a duodenal fiberscope. Gastroenterology 67: 944–951
Esteller M, Tortola S, Toyota M, Capella G, Peinado MA, Baylin SB, Herman JG (2000) Hypermethylation-associated inactivation of p14ARF is independent of p16INK4a methylation and p53 mutational status. Cancer Res 60: 129–133
Esteller M, Corn P, Baylin SB, Herman JG (2001) A gene hypermethylation profile of human cancer. Cancer Res 61: 3225–3229
Ferrari AP, Lichtenstein DR, Slivka A (1994) Brush cytology during ERCP for the diagnosis of biliary and pancreatic malignancies. Gastrointes Endosc 40: 140–145
Furuya N, Kawa S, Akamatsu T, Furihata K (1997) Long-term follow-up of patients with chronic pancreatitis and k-ras gene mutation detected in pancreatic juice. Gastroenterology 113: 593–598
Gibbs DD (1963) Degenerating cells in bile-stained gastric aspirates. Acta Cytol 7: 311–314
Hatfield ARW, Smithies A, Wilkins R, Levi AJ (1976) Assessment of endoscopic retrograde cholangiopancreatography (ERCP) and pure pancreatic juice cytology in patients with pancreatic disease. Gut 17: 14–21
Herman JG, Graff JR, Myohänen S, Nelkin BD, Baylin SB (1996) Methylation-specific PCR: a novel PCR assay for methylation status of CpG islands. Proc Natl Acad Sci USA 93: 9821–9826
Hruban RH, van Mansfeld ADM, Offerhaus GJA, van Weering DH, Allison DC, Goodman SN, Kensler TW, Bose KK, Cameron JL, Bos JL (1993) K-ras oncogene activation in adenocarcinoma of the human pancreas. Am J Pathol 143: 545–554
Hsieh CJ, Klump B, Holzmann K, Borchard F, Gregor M, Porschen R (1998) Hypermethylation of the p16INK4a promoter in colectomy specimen of patients with long-standing and extensive ulcerative colitis. Cancer Res 58: 3942–3945
Iida S, Akiyama Y, Nakajima T, Ichikawa W, Nihei Z, Sugihara K, Yuasa Y (2000) Alterations and hypermethylation of the p14(ARF) gene in gastric cancer. Int J Cancer 87: 654–658
Kamijo T, Zindy F, Roussel MF, Quelle DE, Downing JR, Ashmun RA, Grosveld G, Sherr CJ (1997) Tumour suppression at the mouse INK4a locus mediated by the alternative reading frame product p19ARF. Cell 91: 649–659
Klump B, Hsieh CJ, Holzmann K, Gregor M, Porschen R (1998) Promoter hypermethylation of the CDKN2/p16INK4a tumour suppressor gene during neoplastic progression in Barrett's esophagus. Gastroenterology 115: 1381–1386
Lemon HM, Byrnes WW (1949) Cancer of the biliary tract and pancreas. Diagnosis from cytology of duodenal aspirations. JAMA 141: 254–257
Moore PS, Orlandini S, Zamboni G, Capelli P, Rigaud G, Falconi M, Bassi C, Lemoine NR, Scarpa A (2001) Pancreatic tumours: molecular pathways implicated in ductal cancer are involved in ampullary but not in exocrine nonductal or endocrine tumourigenesis. Br J Cancer 84 (2): 253–262
Nakaizumi A, Tatsuta M, Uehara H, Takenaka A, Iishi H, Kitamra T, Ohigashi H, Ishikawa O, Okuda S, Wada A (1995) Effectiveness of the cytologic examination of pure pancreatic juice in the diagnosis of early neoplasia of the pancreas. Cancer 76: 750–757
Niederhuber JE, Brennan MF, Menck HR (1995) The national cancer data base report on pancreatic cancer. Cancer 76: 1671–1677
Parker SL, Tong T, Bolden S, Wingo PA (1996) Cancer statistics 1996. CA Cancer J Clin 65: 5–27
Pomerantz J, Schreiber-Agus N, Liegois NJ, Silverman A, Alland L, Chin L, Potes J, Chen K, Orlow I, Lee HW, Cordon-Cardo C, DePinho RA (1998) The INK4a tumour suppressor gene product, p19ARF, interacts with MDM2 and neutralizes MDM2's inhibition of p53. Cell 92: 713–723
Quelle DE, Zindy F, Ashmun RA, Sherr CJ (1995) Alternative reading frames of the INK4a tumour suppressor gene encode two unrelated proteins capable of inducing cell cycle arrest. Cell 83: 993–1000
Ryan ME (1991) Cytologic brushings of ductal lesions during ERCP. Gastrointes Endosc 37: 139–142
Saurin JC, Joly Pharaboz MO, Pernas P, Henry L, Ponchon T, Madjar J (2000) Detection of ki-ras gene point mutations in bile specimens for the differential diagnosis of malignant and benign biliary strictures. Gut 473: 357–361
Schutte M, Hruban RH, Geradts J, Maynard R, Hilgers W, Rabindran SK, Moskaluk CA, Hahn SA, Schwarte-Waldhoff I, Schmiegel W, Baylin SB, Kern SE, Herman JG (1997) Abrogation of the Rb/p16 tumour-suppressive pathway in virtually all pancreatic carcinomas. Cancer Res 57: 3126–3130
Sherr CJ (1996) Cancer cell cycles. Science 276: 1672–1677
Song SH, Jong HS, Choi HH, Kang SH, Ryu MH, Kim NK, Kim WH, Bang YJ (2000) Methylation of specific CpG sites in the promoter region could significantly downregulate p16INK4a expression in gastric adenocarcinoma. Int J Cancer 87: 236–240
Stott FJ, Bates S, James M, McConnell BB, Starborg M, Brookes S, Palmero I, Ryan K, Hara E, Vousden KH, Peters G (1998) The alternative product from the human CDKN2a locus, p14(ARF), participates in a regulatory feedback loop with p53 and MDM2. EMBO J 17: 5001–5014
Tada M, Ohashi M, Shiratori Y, Okudaira T, Komatsu Y, Kawabe T, Yoshida H, Machinami R, Kishi K, Omata M (1996) Analysis of K-ras gene mutation in hyperplastic duct cells of the pancreas without pancreatic disease. Gastroenterology 110: 227–231
Tada M, Omata M, Kawai S, Saisho H, Ohto M, Saiki RK, Sninsky J (1993) Detection of ras gene mutations in pancreatic juice and peripheral blood of patients with pancreatic adenocarcinoma. Cancer Res 53: 2472–2474
Tatsuta M, Yamamura H, Yamamoto R, Okano Y, Morii T, Okuda S, Tamura H (1983) Significance of carcinoembryonic antigen levels and cytology of pure pancreatic juice in diagnosis of pancreatic cancer. Cancer 52: 1880–1885
Trümper LH, Bürger B, von Bonin F, Hintze A, von Blohn G, Pfreundschuh M, Daus H (1994) Diagnosis of pancreatic adenocarcinoma by polymerase chain reaction from pancreatic secretions. Br J Cancer 70: 278–284
Urban T, Ricci S, Grange JD, Lacave R, Boudghene F, Breittmayer F, Languille O, Roland J, Bernaudin JF (1993) Detection of c-Ki-ras mutation by PCR/RFLP analysis and diagnosis of pancreatic adenocarcinomas. J Natl Cancer Inst 85: 2008–2012
Van Laethem JL, Vertongen P, Deviere J, Van Rampelbergh J, Rickaert F, Cremer M, Robberecht P (1995) Detection of c-Ki-ras gene codon 12 mutations from pancreatic duct brushings in the diagnosis of pancreatic tumours. Gut 36: 781–787
Venu RP, Geenen JE, Kini M, Hogan WJ, Payne M, Johnson GK, Schmalz MJ (1990) Endoscopic retrograde brush cytology. Gastroenterology 99: 1474–1479
Yanagisawa A, Ohtake K, Ohashi K, Hori M, Kitagawa T, Sugano H, Kato Y (1993) Frequent c-Ki-ras oncogene activation in mucous cell hyperplasias of pancreas suffering from chronic inflammation. Cancer Res 53: 953–956
Zhang Y, Xiong Y, Yarbrough WG (1998) ARF promotes MDM2 degradation and stabilizes p53: ARF-INK4a locus deletion impairs both the Rb and p53 tumour suppression pathways. Cell 92: 725–734
Acknowledgements
This study was supported by a grant from the Interdisciplinary Clinical Research Center Tübingen (IZKF IIIB2) and the German Competence Network for Inflammatory Bowel Disease. BK is supported by the Deutsche Krebshilfe (70-2601).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Klump, B., Hsieh, C., Nehls, O. et al. Methylation status of p14ARF and p16INK4a as detected in pancreatic secretions. Br J Cancer 88, 217–222 (2003). https://doi.org/10.1038/sj.bjc.6600734
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bjc.6600734
Keywords
This article is cited by
-
An overview of genetic mutations and epigenetic signatures in the course of pancreatic cancer progression
Cancer and Metastasis Reviews (2021)
-
Clinicopathological Significance of CDKN2A Promoter Hypermethylation Frequency with Pancreatic Cancer
Scientific Reports (2015)
-
High-frequency aberrantly methylated targets in pancreatic adenocarcinoma identified via global DNA methylation analysis using methylCap-seq
Clinical Epigenetics (2014)
-
Correlation between T-cadherin gene expression and aberrant methylation of T-cadherin promoter in human colon carcinoma cells
Medical Oncology (2012)
-
The role of epigenetic alterations in pancreatic cancer
Journal of Hepato-Biliary-Pancreatic Surgery (2006)