Abstract
Data sources
Medline (and PubMed), Web of Science, the Cochrane Library and Sumsearch.
Study selection
Randomised and pseudo-randomised controlled trials (RCTs), longitudinal, cohort and case–control studies, and well-designed cross-sectional studies in English or Dutch were included if they reported on an association between periodontal disease and nutrient dietary intake or serum levels, included participants older than 50 years, with preference given to studies reporting separate outcomes for specific age groups. Year of publication was limited to between January 1990 and May 2007.
Data extraction and synthesis
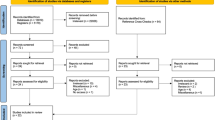
The search was run and retrieved articles screened by the first two review authors. Potentially relevant studies were assessed for quality on the basis of: clearly defined study population, adequate randomisation (intervention study), selection bias assessment, adequate participant and observer blinding, adequate follow-up and evaluating confounding aspects, mainly diabetes mellitus, alcohol consumption and smoking. Weighted mean differences and standard deviations of periodontal disease scores between control and intervention groups, odds ratios (ORs), relative risk and their corresponding 95% confidence intervals (CIs) were extracted from all individual publications.
Results
Eight articles were included in the review, all of which were cross-sectional studies and did not include any institutionalised elderly participants. Reported studies found that low serum folate levels (vitamin B9) gave an OR for periodontal disease of 0.74 (95% CI 0.59–0.93), decreased Vitamin C was associated with a small increased risk of periodontal disease (OR 1.19, 95% CI 1.05–1.33), 0.53 (95% CI 0.42–0.68), calcium levels appeared not to have any effect on periodontal disease, OR 1.11 (95% CI 0.71–1.71) and OR 1.13 (95% CI 0.86–1.48) in men and women respectively, vitamin D deficiency increased clinical attachment loss by 0.39 mm (95% CI 0.17–0.60) and 0.26 mm (95% CI 0.09–0.43) in men and women respectively.
Conclusions
The quality of the studies was too low to make reliable conclusions and therefore an association of vitamin B complex, vitamin C, vitamin D, calcium and magnesium deficiencies with periodontal disease in elderly people is not evident.
Similar content being viewed by others
Commentary
Historically, periodontal disease was seen as an inflammatory disease with little link to nutrition, and many early epidemiological studies failed to show associations between nutritional status and periodontal disease. These studies, however, used inappropriate nutritional methodologies, failed to control for confounding variables and employed poor case definitions, which may account for their inconsistent results.1
This paper systematically reviewed published literature on possible associations between different nutrient deficiencies and periodontal disease in elderly people. Overall, the studies included were limited due to restricted selection and information bias. No RCTs or relevant longitudinal cohort studies were found. All included studies were cross-sectional studies. Furthermore, studies focusing on specific age groups were rarely found, and information on the dietary intake of populations studied was incomplete in several publications.
In general, cross-sectional studies provide a lower level of evidence supporting a causal effect than RCTs and cohort or case-control studies. Following the publication of this systematic review, a six-year longitudinal study in the non-institutionalised elderly population has demonstrated that the total serum calcium levels were significantly associated with the progression of periodontal disease regardless of other potential confounding factors including smoking, random blood sugar levels and gingival bleeding as well as the levels of immunoglobulin and the number of teeth present at baseline.2
In a recent published longitudinal study, Garcia et al.3 reported that calcium and vitamin D supplementation had a modest positive effect on periodontal health. Vitamin D supplements may reduce the severity of periodontal disease if used at doses higher than 800-1000 IU daily, thus supporting the rationale for testing the potential beneficial role of vitamin D on periodontal disease in RCTs. As the authors said, this study has several limitations: the sample size was small; between-group differences in vitamin D intakes were relatively small; subjects were relatively periodontally healthy and serum levels of 25-hydroxyvitamin D3 were not determined.
Although it is reasonable to consume a nutritionally adequate diet to maintain host resistance and maintain the integrity of the periodontal tissues, insufficient evidence is available to justify treatment with vitamin and mineral supplementation in the adequately nourished individual. Periodontal disease is an infectious disease caused by bacterial infection and can be treated and prevented by the elimination of bacterial plaque in the adequately nourished individual. In patients who have inadequate nutrition, it may be reasonable to suggest a vitamin or mineral supplement.
Indeed, more well-designed, confounding-controlled, longitudinal studies and better periodontal disease criteria are needed to produce conclusive evidence on this subject.4
Practice point
-
Dental professionals should concentrate on plaque control rather than vitamin and mineral supplementation to prevent and control periodontal disease in their patients.
References
Moynihan P . Nutrition & oral health: update on nutrition and periodontal disease. Quintessence Int 2008; 39: 326–330.
Amarasena N, Yoshihara A, Hirotomi T, Takano N, Miyazaki H . Association between serum calcium and periodontal disease progression in non-institutionalized elderly. Gerodontology 2008; 25: 245–250.
Garcia MN, Hildebolt CF, Miley DD, et al. One-year effects of vitamin D and calcium supplementation on chronic periodontitis. J Periodontol 2011; 82: 25–32.
Meisel P, Springmann C, Kocher T . Comment on “Association of some specific nutrient deficiencies with periodontal disease in elderly people: a systematic literature review”. Nutrition 2010; 26: 137; author reply 138.
Author information
Authors and Affiliations
Additional information
Address for correspondence: G-J van der Putten, Zorgaccent Amersfoort Medical Services, Amersfoort, The Netherlands. E-mail: gjvdputten@hetnet.nl
van der Putten GJ, Vanobbergen J, De Visschere L, Schols J, de Baat C. Association of some specific nutrient deficiencies with periodontal disease in elderly people: a systematic literature review. Nutrition 2009; 25: 717–722.
Rights and permissions
About this article
Cite this article
Yeung, C. Nutrients and periodontal disease. Evid Based Dent 13, 14–15 (2012). https://doi.org/10.1038/sj.ebd.6400840
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400840