Abstract
Data Sources
Medline and hand searching of bibliographies of identified articles.
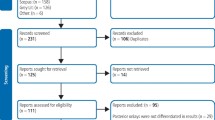
Study Selection
Studies were selected independently by two reviewers. Prospective and retrospective cohort studies with a mean follow-up period of five or more years with clinical examination at follow-up that reported details of the characteristics of the superstructures were included.
Data Extraction and Synthesis
Information on survival and on biological and technical complications was retrieved. Survival was defined as the RBBs remaining in situ at the examination without multiple debonding, but irrespective of its condition. Failure was defined as the RBBs that were lost and required refabrication, or multiple recementations. Biological complications included caries on abutment teeth, and periodontal disease progression. Technical complications analyzed included loss of retention, with or without loss of the reconstruction, and fractures of veneers with or without loss of the reconstruction veneers, with or without loss of the reconstruction.
Results
17 studies that met the inclusion criteria. Meta-analysis of these studies indicated an estimated survival of RBBs of 87.7% (95% confidence interval (CI): 81.6–91.9%) after 5 years. The most frequent complication was debonding (loss of retention), which occurred in 19.2% (95% CI: 13.8–26.3%) of RBBs over an observation period of 5 years. The annual debonding rate for RBBs placed on posterior teeth (5.03%) tended to be higher than that for anterior-placed RBBs (3.05%). This difference, however, did not reach statistical significance (P=0.157). Biological complications, like caries on abutments and RBBs lost due to periodontitis, occurred in 1.5% of abutments and 2.1% of RBBs, respectively.
Conclusions
Despite the high survival rate of RBBs after 5 years, technical complications such as debonding are frequent. This, in turn, means that substantial amounts of extra chair time may by needed following the incorporation of RBBs. Thus, there is an urgent need for prospective studies with a follow-up time of 10 years or more, to evaluate the long-term outcomes of RBBs.
Similar content being viewed by others
Commentary
This study was a systematic review examining the 5-year survival and complication rates of resin-bonded bridges (RBBs). The main study results were presented as estimated failure rate per 100 RBB years and estimated 5-year survival rate. The estimated failure rate per 100 RBB years at risk was 2.61 (95% CI 1.68–4.06) and 5-year survival was estimated at 87.7% (95% CI 81.6–91.9).
Systematic reviews provide an excellent vehicle for summarizing the evidence on a particular topic. They differ from their narrative counterparts by focusing on a narrow topic, performing an exhaustive search for evidence, maintaining strict methods for study inclusion/exclusion criteria and data extraction, and are typically reproducible. Systematic reviews can be done on either interventional (trials) or observational studies such as cohort and case-control designs. Reviews on observational studies can be negatively affected by confounding and selection bias1.
This study was a systematic review that originally searched for randomized controlled trials (RCTs) comparing resin-bonded bridges (RBB) to fixed partial dentures, but subsequently reported on observational studies on RBB survival. The authors claimed that no RCTs were found, yet a description of included studies mentioned that groups were randomly assigned to different types of retainers and cements. There was no mention of controlled (non-randomized) clinical trials on RBBs in the literature. The authors stated that the systematic review would be based on prospective and retrospective cohort studies, yet it appeared as if some of the included studies were case series. This is relevant as case series differ from cohort designs in that the former have no comparator group and are thought to provide relatively weak scientific evidence2. Thus, it appears as if this was a systematic review of trials, cohorts, and case series which deviated from the stated study inclusion criteria. That said, these designs can provide data on prosthesis survival rates, although systematic reviews are typically limited to one type of study.
The statistical analysis used was rather interesting. A Poisson distribution was used to calculate the number of occurrences (failures or complications) during a period of time, and Poisson regression modeling was used to evaluate whether covariates such as arch type or position affected survival rates. The Poisson distribution can be used when events occur independently and are random. One could question the independence of these events, as one de-bonding event could make subsequent events more likely to occur. Life tables or a Kaplan-Meier survival graph may have been helpful in this respect, which would also have accounted for censored observations such as patient attrition.
Exclusion criteria, study selection, and data extraction methods were clearly defined. However, there was no commentary on the quality of studies meeting the inclusion criteria, which is necessary for all study designs. That is, summaries of highly biased studies are likely to provide biased results. Clinical heterogeneity among studies was large with different techniques, materials, and cements used for prosthesis fabrication. Clinical heterogeneity can lead to statistical heterogeneity, and a meta-analysis showed a lack of overlapping confidence intervals for RBB failure rate/100 years. Performing a meta-analysis on observational studies, especially where extreme clinical heterogeneity exists, can produce spurious results. However, systematic reviews on prosthesis longevity typically provide a summary estimate of 5, 10, and 15 year survival rates. Regression analysis showed failure rates lower in the maxilla versus the mandible but these results were not statistically significant, also the case for differences in failure rates between anterior and posterior RBBs.
The 5-year survival estimate for RBBs (87.7%) appears to be lower than for implant FPDs and conventional FPDs for the same time period. One cannot extrapolate 10 and 15 year results for RBBs, however, 5-year success rates for RBBs were poorer than 10 and 15-year success rates for conventional FPDs which are summarized as follows:
-
Longevity on FPDs is approximately 92% at 10 years and 75% at 15 years3
-
FPD survival is 90% at 10 years and 74% at 15 years4
-
Longevity on implant-supported prostheses is approximately 94% at 7 years5
-
Implant-supported prosthesis success rates are 89% at 15 years6
-
Implant studies had smaller confidence intervals as compared with articles on conventional prosthetics
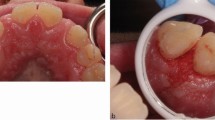
In summary, this systematic review did not strictly adhere to the required standards, such as limiting including studies to one type of design, describing the quality of included studies, and performing a meta-analysis on different designs where clinical heterogeneity exists. Although this does not appear to be a high quality systematic review, it does not differ significantly in quality from other systematic reviews on prosthesis survival. A systematic review of trials may have provided fewer included studies, but greater precision in terms of survival estimates. While this may be the current best evidence on RBBs, clinical judgment and patient preferences should always be important factors in decisions involving individual patients7. For example, in cases with short-span edentulous spaces, adequate clinical crown height, and plenty of occlusal clearance, RBBs can offer a conservative, inexpensive alternative to conventional FPDs and implant-supported prostheses.
References
Egger, M., Davey Smith, G., Altman, D G. Systematic Reviews in Health Care: meta-analysis in context. London: BMJ. Publishing Group, 2003.
Greenhalgh T. How to Read a Paper: The basis of evidence-based medicine London: BMJ Publishing Group, 2001
Scurria, M.S., Bader, J.D., Shugars, D.A. (1998) Meta-analysis of fixed partial denture survival: Prostheses and abutments. Journal of Prosthetic Dentistry, 79: 459–464.
Creugers, N.H.J., Kayser, A. F., Van't Hot, M.A., (1994) A meta-analysis of durability data on conventional fixed bridges. Community Dentistry and Oral Epidemiology, 22: 448–452.
Lindh, T., Gunne, J., Tillberg, A., Molin, M., (1998) A meta-analysis of implants in partial edentulism. Clinical Oral Implants Research, 9: 80–90.
Attard, N.J., and Zarb, G.A. (2003) Implant prosthodontic management of partially edentulous patients missing posterior teeth: The Toronto experience. J Prosth Dent 89:352–359.
Sackett, D.L., Strauss, S.E., Richardson, W.S., Rosenberg, W., and Haynes, R.B. (2000) Evidence-Based Medicine: How to Practice and Teach EBM, Edinburgh. Churchill Livingstone.
Author information
Authors and Affiliations
Additional information
Address for Correspondence; Bjarni E. Pjetursson, Department of Prosthodontics, University of Iceland, Vatnsmyrarvegur 16,IS 101 Reykjavik, Iceland E-mail: bep@hi.is
Pjetursson BE, Tan WC, Tan K, Brägger U, Zwahlen M, Lang NP. A systematic review of the survival and complication rates of resin-bonded bridges after an observation period of at least 5 years. Clin Oral Implants Res. 2008 Feb; 19(2):131–41.
Rights and permissions
About this article
Cite this article
Abt, E. Survival rates for resin bonded bridges. Evid Based Dent 9, 20–21 (2008). https://doi.org/10.1038/sj.ebd.6400567
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400567