Abstract
Data sources
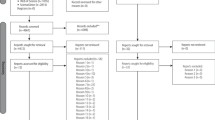
Searches were made using the Cochrane Central Register of Controlled Trials, Medline, Embase, Latin American and Caribbean Health Sciences Literature, Bibliografia Brasileira de Odontologia and SciELO (the Scientific Electronic Library Online).
Study selection
Studies chosen were randomised controlled trials (RCT) or quasi-RCT comparing all types of oral and functional orthopaedic appliances with placebo or no treatment, in children of 15 years old or younger.
Data extraction and synthesis
Data were independently extracted by two review authors. Authors were contacted for additional information. Risk ratios with 95% confidence intervals were calculated for all important dichotomous outcomes.
Results
A total of 384 trials were identified, of which only one, reporting results from a total of 23 patients, was suitable for inclusion in the review. Data provided in the published report did not answer all the questions from this review, but did answer some: the results presented favour treatment.
Conclusions
At present there is not sufficient evidence to state that oral appliances or functional orthopaedic appliances are effective in the treatment of obstructive sleep apnoea (OSA) syndrome in children. Oral appliances or functional orthopaedic appliances may be helpful in the treatment of children with craniofacial anomalies which are risk factors for apnoea.
Similar content being viewed by others
Commentary
Apnoea is a breathing disorder marked by reduced or indeed absence of airflow through the mouth and nose. It is aggravated by adenotonsillar hypertrophy, obesity, neuromuscular disorders and some craniofacial disorders. It is fairly common: up to 10.3% of children have OSA. The most common treatment is adenotonsillectomy but this obviously has significant surgical risks and expense. In addition, the procedure does not always work. Children who do not respond to adenotonsillectomy tend to have a narrower epipharyngeal space, a poorly developed maxilla and mandibular retrusion.
Intra-oral appliances have been used for some time to treat OSA in both adults and children. This review uses, as its indicator of success, a reduction to less than one episode of apnoea per hours as measured by polysomnography (regarded as the gold standard for the diagnosis of OSA). Unfortunately, only one study met the reviewers' selection criteria. In that study, 62.4% of subjects showed at least a 50% improvement in the number of apnoeas and hypopnoeas per hour of sleep (apnoea/ hypopnoea index) although it was impossible to establish in how many of the subjects it dropped below 1.0, which was the primary indicator of success. The review authors conclude, however, that there is “no strong evidence of an effect” rather than “strong evidence of no effect”.
Although this study was well done, in my own practice, patients have responded well to oral appliances via their own subjective assessment or via other outcome indicators such as the Epworth Sleepiness Scale,1 despite no obvious improvement according to polysomnography. I appreciate that polysomnography is the gold standard and can be scientifically measured but it may not be giving us the full story. Fitting an intra-oral appliance for a child is a cheap and risk-free procedure compared with adenotonsillectomy, and I suggest it is a good first line of attack with surgery reserved for the non-responders.
Practice points
Oral appliances do not always work in the treatment of OSA in children, but as they are noninvasive and relatively risk-free, may have a role before adenotonsillectomy is considered.
Some patients respond well to appliances using other assessment criteria which are not always linked to a comparable improvement in polysomnography.
References
Johns MW . A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14:540–545.
Author information
Authors and Affiliations
Additional information
Address for correspondence: Luisa Fernandez, Group Co-ordinator, Cochrane Oral Health Group, MANDEC, Third Floor Dental Hospital, University of Manchester, Higher Cambridge Street, Manchester M15 6FH, UK. E-mail: luisa.fernandez@manchester.ac.uk
Carvalho FR, Lentini-Oliveira D, Machado MAC, Prado GF, Prado LBF, Saconato H. Oral appliances and functional orthopaedic appliances for obstructive sleep apnoea in children. Cochrane Database Syst Rev 2007; issue 2
Rights and permissions
About this article
Cite this article
Fox, N. Insufficient evidence to confirm effectiveness of oral appliances in treatment of obstructive sleep apnoea syndrome in children. Evid Based Dent 8, 84 (2007). https://doi.org/10.1038/sj.ebd.6400513
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ebd.6400513