Abstract
Data obtained from a mouse model indicated that the ectopic expression of the Grm1 gene is sufficient for transforming melanocytes and causing malignant melanoma in vivo. In addition, it has also been documented that the GRM1 gene is aberrantly expressed in human melanomas. Here we have performed a genetic association study to elucidate whether the GRM1 gene contributes to human melanoma susceptibility. To carry out this study, we initially genotyped 250 melanoma patients and 329 nonselected and nonrelated controls with three single nucleotide polymorphisms, rs854145, rs362962 and rs6923492, located in the intron 1, intron 4 and exon 10 of the GRM1 gene, respectively. To perform sample genotyping, we used pyrosequencing techniques. Regarding rs854145 and rs6923492, there were no differences in genotypic distribution or allelic frequency between patients and controls. However, we observed (i) a higher frequency of patients carrying the C allele of rs362962 than in controls (OR=1.40, CI=[1.01–1.95], P=0.045), and (ii) that difference became greater in a subgroup of patients with a low level of sun exposure and tumours located on the trunk and extremities (OR=2.10, CI=[1.26–3.51], P=0.0039). To confirm these observations, the sample size of both patient and control groups was increased. In total, 464 patients and 561 controls were genotyped for the rs362962 polymorphism. Only the second observation was confirmed (OR=1.69, CI=[1.16–2.47], P=0.0064). Our results suggest that the GRM1 gene may contribute to melanoma susceptibility in that specific group of patients.
Similar content being viewed by others
Introduction
Melanoma develops from the malignant transformation of melanocytes, the pigment-producing cells that reside in the basal epidermal layer in human skin. Melanoma represents a significant and growing public health burden worldwide. The incidence of this disease in Caucasian populations is increasing faster than other kind of cancers, except lung cancer in women,1 and it remains one of the most common types of cancer among young adults.2
As in other complex diseases, including other types of sporadic cancer, both genetic and environmental agents are risk factors for melanoma development. Exposure to the sun is generally accepted as a major causative factor.3, 4 However, the role of exposure to the sun is complex and has paradoxical features. In this way, it appears that melanoma risk is typically associated with intermittent sun exposure rather than cumulative sun exposure.5 Thus, the majority of melanomas of light-skinned people occur on the trunk and extremities. These locations are frequently affected in melanoma patients under age 50 years. In contrast, melanomas located on skin subject to chronic sun damage, such as the face or the neck, tend to occur later in life, develop more slowly, appearing at ages over 50 years.6 In addition, melanomas also develop in sun-protected sites such as oral, nasal and anogenital mucosa, and skin of soles and palms. Furthermore, several studies have shown that chronic exposure to ultraviolet (UV) light exerts a protective effect.7, 8
The complex relationship between sun exposure and melanoma could be explained by the genetic heterogeneity between individuals. Some studies confirm the importance of host susceptibility, represented by pigmentary factors and the tendency to develop benign or atypical moles, in the aetiology of this disease.9, 10 During the previous years, some studies have been performed to detect low-risk gene variants for sporadic malignant melanoma susceptibility. Candidate genes selected include those related to melanin synthesis,11 DNA repair,12 cell cycle13, 14 and some metabolic pathways related to control of mitosis.15, 16
Induced mouse mutants are tools for uncovering new genes and pathways implicated in a particular disease. One of these models generated by Zhu et al17 spontaneously developed melanomas in the absence of any known chemical carcinogen or UV radiation. Specifically, those animals were predisposed to develop multiple melanomas primarily affecting the pinnae of the ears, perianal region, eyelid, snout, trunk and legs. Several years later, they demonstrated that the susceptibility to melanoma was due to an upregulation of the Grm1 gene expression.18 Extending these studies to human melanomas, they also observed that the GRM1 gene was aberrantly expressed in 7 of 19 melanoma samples and 12 of 18 melanoma cell lines but not in normal human melanocytes or benign moles.
The GRM1 gene is located at 6q24 in humans. It encodes the metabotropic glutamate receptor 1 (mGluR1), expressed at high levels in the central nervous system. In general, metabotropic receptors are coupled to intracellular signal-transduction pathways through G proteins. They are members of the family of seven transmembrane domain G protein-coupled receptors (GPCRs). GPCRs and G proteins have been implicated in tumorigenesis through either mutational activation or overexpression.19 In addition, glutamate has been associated with tumour growth in both neuronal and non-neuronal cancers.20, 21
In this work, we have investigated whether the GRM1 gene is related to sporadic malignant melanoma susceptibility in humans. Initially, we performed a case–control study using 250 melanoma patients, 329 nonselected controls and 3 single nucleotide polymorphisms (SNPs), rs854145, rs362962 and the rs6923492, located in the intron 1, intron 4 and exon 10 of the GRM1 gene, respectively. To confirm the positive associations detected, we performed a joint analysis extending our cohort to 464 melanoma patients and 561 nonselected controls.
Materials and methods
Patients
The study consisted of 464 patients diagnosed with malignant melanoma and 561 nonselected and nonrelated individuals (control group). All of them were obtained from the outpatient clinics of the following hospitals in Madrid: 12 de Octubre Hospital, Clínico San Carlos Hospital, Fundación Alcorcón Hospital and Ramon y Cajal Hospital. The ethnicity of all patients and controls was Caucasian (white Europeans).
We classified patients according to sun exposure using a similar criterion to the one described by Berwick et al.22 Specifically, we considered patients with a low level of sun exposure, those patients who had never had sunburns, who had never sunbathed during the summertime, who had spent less than 10 days per year doing outdoor recreational or occupational activities and who had never lived in tropical countries. All patients were interviewed by the same interviewer using a standardized questionnaire.
The study was approved by the Institutional Review Boards of all participant hospitals. Written consent was obtained from all individuals before sampling.
DNA extraction, SNP selection and genotyping
We obtained 5 ml of peripheral blood from all patients to isolate germline DNA from leucocytes. DNA extraction was performed automatically according to standard procedures using the Magnapure DNA isolation system (Roche Diagnostics, Mannheim, Germany). To perform PCRs, we prepared aliquots of DNA at a concentration of 10 ng/μl. The rest of the stock was cryopreserved at −20°C.
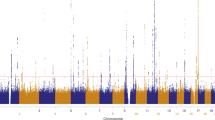
The SNPs used in the study were rs854145, rs362962 and the rs6923492 within intron 1, intron 4 and exon 10 of the GRM1 gene, respectively (Figure 1). All of them were selected from the database of the ‘UCSC Genome Bioinformatics’ (http://www.genome.ucsc.edu/). Validations of the polymorphisms were carried out in a pool of DNA from 40 unrelated individuals using PCR and bi-directional automated DNA sequencing (data not shown). According to the SNPbrowser software version 3.1 (Applied Biosystems, Foster City, CA, USA), the SNPs were located in different linkage disequilibrium blocks in Caucasians. Primers used to amplify the segment of the GRM1 gene that contains those polymorphisms and PCR conditions are shown in Table 1. PCRs were performed in a GeneAmp PCR System 9700 thermal cycler (Applied Biosystems) using standard PCR chemical conditions. Briefly, a final volume of 20 μl containing 20 ng of genomic DNA, 0.5 μ M of each amplification primer, 1.5 mM MgCl2, 100 μ M of each dNTP, 2 μl of PCR-buffer 10 × (Roche Diagnostics) and 2 IU Taq DNA polymerase (Roche Diagnostics). Genotyping was performed using a PSQ96 Pyrosequencer (Biotage AB, Uppsala, Sweden) and the sequencing primers described in Table 1 according to the manufacturer's instructions. Figure 2 shows examples of genotypic results using the pyrosequencing techniques.
To test the accuracy of our genotyping data, genomic DNA from 10% of all peripheral blood samples included in this study were freshly extracted and genotyped. A minimum of 99% of genotype coincidence was demanded for all genetic markers.
Statistical analysis
To test Hardy–Weinberg equilibrium and compare allelic and genotypic frequencies between groups, we used tests adapted from Sasieni.23 These calculations were performed using the online resource at the Institute for Human Genetics, Munich, Germany (http://ihg.gsf.de).
Linkage disequilibrium value (d′) between two studied genetic markers, haplotypic frequencies and haplotype-based association analysis were calculated using Thesias software available at http://genecanvas.ecgene.net/.
To compare quantitative variables among genotypic groups, we used Kruskall–Wallis tests (data not normally distributed).
The estimation of power to detect risk to melanoma was calculated for the rs362962 polymorphism using Episheet software available at http://members.aol.com/krothman.
Unconditional logistic regression models were used to obtain odds ratio estimates adjusted by age and sex. These calculations were carried out using SPSS software (Leeds, England, UK).
For multiple testing correction, we established a cutoff P-value of 0.0083 (P=0.05/6), taking into account the three genetic markers used in the two phenotypic groups studied.
Results
Single SNPs analysis
First, we studied 250 melanoma patients and 329 nonselected controls from the Spanish geographical area (Table 2). All of them were genotyped for the rs854145, rs362962 and rs6923492 SNPs in the intron 1, intron 4 and exon 10 of the GRM1 gene, respectively. The genotypic distributions for each polymorphism were in accordance with the Hardy–Weinberg equilibrium (HWE) law (all P-values >0.05) in both patient and control groups (data not shown).
No differences were observed in the allelic or genotypic distribution of the rs854145 and rs6923482 SNPs between patients and controls. However, the frequency of individuals carrying the C allele of rs362962 in the patient group was slightly higher than that observed in the control group (OR=1.40, CI=[1.01–1.95], P=0.045 – allele positivity test from Sasieni23; Table 2). This result suggests that only the C allele of the rs362962 polymorphism might be a very low-risk allele for melanoma susceptibility. However, the previous result may also mean that the C allele of rs362962 might be a genetic factor of melanoma susceptibility in a subgroup of patients.
Owing to the fact that the Grm1 ‘knock in’ mouse model develops melanoma in the absence of UV radiation,17, 18 we decided to investigate whether the C allele of rs362962 could be a susceptibility genetic factor for human melanoma tumours that do not appear to be dependent on sun exposure. Therefore, we selected those patients whose tumours were located on skin zones that are not usually exposed to sunlight such as the trunk and extremities, and who reported a low level of sun exposure, as described in the Materials and methods section. Interestingly, these patients (n=75) showed a higher frequency of CC and CT genotypes than those observed in the control group (OR=2.10, CI=[1.26–3.51], P=0.0039, allele positivity test). This was not observed when the rs854145 or rs6923482 polymorphisms were studied.
Haplotypic analysis
To test a combined effect of the three polymorphisms of GRM1 regarding melanoma susceptibility, we performed a haplotype analysis using the Thesias software. This program calculated the linkage disequilibrium value between genetic markers (Figure 1) and the frequencies of specific haplotypes under linkage disequilibrium. As mentioned above, we confirmed that the SNPs selected were in different linkage disequilibrium blocks (−1<d′<1). According to our previous results, haplotypes carrying the C allele of rs362962 were more abundant in the patient group than in the control group; however, we did not observe significant differences in haplotypic distribution between patients and controls (data not shown). Similarly, the haplotypes carrying the C allele of rs362962 were more abundant in the patient subgroup who reported a low level of sun exposure and whose tumours were located on trunk or extremities than in the control group, but no one of them reached significant differences between the two groups. Taking into account that the three polymorphisms are in different LD blocks, these results strongly suggest that the causative mutation must be in the genetic background of rs362962 polymorphisms, but not in the background of the others SNPs.
Joint analysis
To confirm the results obtained with the rs362962 polymorphism, we decided to increase the size of both patient and control groups. In total, 464 patients and 561 controls were genotyped for the rs362962 polymorphism (Table 3). Again, the genotypic distributions for this marker were in accordance with the HWE law (all P-values >0.05) in both patient and control groups (data not shown). In this study, however, we did not find significant differences between patients and controls. According to the patient/control ratio, sample size and allele prevalence for the marker, we should be able to detect positive OR≥1.4 with a power of 80%. Therefore, we conclude that the effect of the C allele of rs362962 in general on melanoma susceptibility, if present, would be very low.
By contrast, a higher frequency of CC and CT genotypes was observed in the patient group that reported a low level of sun exposure and whose tumours were located on the trunk and extremities (n=136), compared to those observed in the control group (OR=1.69, CI=[1.16–2.47], P=0.00644, allele positivity test, Table 3). This result was not substantially modified when the analysis was adjusted by age and sex (OR=1.65, CI=[1.13–2.43], P=0.010). Taken together, our results suggest that the C allele of rs362962 polymorphism could not be a susceptibility genetic factor for melanoma, in general, but for a specific kind of melanoma not related to sun exposure.
Discussion
The main objective of this study was to investigate whether the GRM1 gene contributes to human melanoma susceptibility since Pollock et al18 reported that this gene is expressed in a large proportion of human melanomas, and they demonstrated that alterations in the expression of Grm1 are sufficient to promote mouse melanocytes transformation. In addition, the transgenic mouse described by Pollock et al develops melanoma in the absence of UV radiation. Interestingly, we found an association of rs362962 with melanoma susceptibility in patients who reported a low level of sun exposure and whose tumours were located on skin zones that are not usually exposed to the sun. This suggests that, as in the case of the mouse model, the GRM1 gene may also be related to human melanoma susceptibility independent of sun exposure.
That finding is dependent on the criteria used to define a low level of sun exposure. The criterion used in this study was similar to those reported by Berwick et al.22 This might be one of the most crucial points of this study since the level of sun exposure has always been particularly difficult to quantify. Taking into account that the patients were born and raised in Spain, a sunny country, it is possible that some periods of sun exposure may have been unintentionally omitted by the patients. On the other hand, the low number of patients who reported a low level of sun exposure and whose tumours were located on the trunk or extremities is a critical point in our study. This could increase the possibility of a type I error in our study. According to that, we observed a lower OR value in the joint study than in the previous study. However, our results are (i) in accordance with those found in the mouse model, (ii) robust enough to pass the joint analysis that we carried out, and, (iii) after multiple testing correction, we find that the association is maintained (P=0.0064<0.0083). In any case, it would be very particularly interesting to investigate whether the same association would be observed in other populations from countries that receive less radiation such as those located in Central Europe and, also, in other melanoma patients whose tumours are located in completely unexposed zones such as the anal, oral, nasal or genital mucosa areas. If this is the case, our finding might also explain the ambiguous relation observed between melanoma susceptibility and sun exposure as was indicated in the Introduction section.
Several reports have indicated that melanoma location could depend on genetic factors as well as sun exposure pattern.6, 9, 10 Consequently to that, Bastian et al24 observed that the pattern of chromosomal aberration found in melanomas depend on anatomical location influenced by the sun exposure pattern. Furthermore, Curtin et al25 reported that these changes include specific alteration in the mitogen-activated protein kinase (MAPK) pathway and the phosphatidylinositol 3′-kinase (PI3K) pathway. In their series, the 81% of melanomas on skin without chronic sun-induced damage had mutations in BRAF, as was reported previously,26 or N-RAS, whereas melanomas on skin with chronic sun-induced damage had infrequent mutations in BRAF and frequent increases in the number of copies of the CCND1 gene. On the other hand, they also found that CDK4 amplification and CDKN2A losses were more common in melanomas located on sun-protected skin and mucosa. All those genes are downstream components of the MAPK pathway. All those findings indicate that alterations activating RAS/mitogen-activated protein kinase pathway are important events on melanoma development,27 but also, that tumorigenesis mechanisms are different in different individuals depending on the their sun exposure pattern. mGluR1 is a GCPR, and, therefore, stimulation of this receptor might lead to the activation of MAPK pathway (revised by Marin and Chen28). Until now, there is no evidence of which cascades could be triggered through the activation of this receptor in human melanocytes. However, it has been reported recently that stimulation of Grm1 by a specific receptor agonist in cell lines from tumours of a mouse model expressing this gene, results in inositol triphosphate accumulation, and ERK1/2 activation via PRKCepsilon.29 If aberrant GRM1 expression would occur in normal human melanocytes, and if this expression would trigger MAPK pathways to promote tumour progression remains unknown. However, if this event occurs, it could be independent of the existence of mutations in the MAPK pathway. Therefore, it could partially explain the susceptibility to develop melanoma in the absence of UV radiation exposure. Whether our results are confirmed in other series, it will be necessary to study if the level of expression of GRM1 gene is increased in people bearing the C allele of rs362962 in GRM1-expressing tissues as well as tumour tissues.
In conclusion, we have presented the first genetic association study evaluating the role of GRM1 gene in human melanoma susceptibility. Our results suggest that this gene could be related with melanoma susceptibility at least in a subgroup of patients. However, this preliminary finding must be confirmed by others in different series and using more genetic markers within the GRM1 gene. In addition, molecular studies will be necessary to understand the role of the expression of GRM1 gene in human melanoma cells. If our studies are confirmed they should affect the design of future studies involving the treatment and prevention of melanoma.
References
Parkin DM, Pisani P, Ferlay J : Estimates of the world-wide incidence of eighteen major cancers in 1985. Int J Cancer 1993; 54: 594–606.
Weinstock MA : Epidemiology, etiology, and control of melanoma. Med Health R I 2001; 84: 234–236.
Marks R : Epidemiology of melanoma. Clin Exp Dermatol 2000; 25: 459–463.
Whiteman DC, Whiteman CA, Green AC : Childhood sun exposure as a risk factor for melanoma: a systematic review of epidemiologic studies. Cancer Causes Control 2001; 12: 69–82.
Elwood JM : Melanoma and sun exposure. Semin Oncol 1996; 23: 650–666.
Elwood JM, Gallagher RP : Body site distribution of cutaneous malignant melanoma in relationship to patterns of sun exposure. Int J Cancer 1998; 78: 276–280.
Beral V, Robinson N : The relationship of malignant melanoma, basal and squamous skin cancers to indoor and outdoor work. Br J Cancer 1981; 44: 886–891.
Vagero D, Ringback G, Kiviranta H : Melanoma and other tumours of the skin among office, other indoor and outdoor workers in Sweden 1961–1979. Br J Cancer 1986; 53: 507–512.
Titus-Ernstoff L, Perry AE, Spencer SK, Gibson JJ, Cole BF, Ernstoff MS : Pigmentary characteristics and moles in relation to melanoma risk. Int J Cancer 2005; 116: 144–149.
Fargnoli MC, Piccolo D, Altobelli E, Formicone F, Chimenti S, Peris K : Constitutional and environmental risk factors for cutaneous melanoma in an Italian population. A case–control study. Melanoma Res 2004; 14: 151–157.
Kennedy C, ter Huurne J, Berkhout M et al: Melanocortin 1 receptor (MC1R) gene variants are associated with an increased risk for cutaneous melanoma which is largely independent of skin type and hair color. J Invest Dermatol 2001; 117: 294–300.
Millikan RC, Hummer A, Begg C et al: Polymorphisms in nucleotide excision repair genes and risk of multiple primary melanoma: the Genes Environment and Melanoma Study. Carcinogenesis 2006; 27: 610–618.
Kumar R, Smeds J, Berggren P et al: A single nucleotide polymorphism in the 3′untranslated region of the CDKN2A gene is common in sporadic primary melanomas but mutations in the CDKN2B, CDKN2C, CDK4 and p53 genes are rare. Int J Cancer 2001; 95: 388–393.
Konishi R, Sakatani S, Kiyokane K, Suzuki K : Polymorphisms of p21 cyclin-dependent kinase inhibitor and malignant skin tumours. J Dermatol Sci 2000; 24: 177–183.
Meyer P, Sergi C, Garbe C : Polymorphisms of the BRAF gene predispose males to malignant melanoma. J Carcinog 2003; 2: 7–11.
Amend KL, Elder JT, Tomsho LP et al: EGF gene polymorphism and the risk of incident primary melanoma. Cancer Res 2004; 64: 2668–2672.
Zhu H, Reuhl K, Zhang X et al: Development of heritable melanoma in transgenic mice. J Invest Dermatol 1998; 110: 247–252.
Pollock PM, Cohen-Solal K, Sood R et al: Melanoma mouse model implicates metabotropic glutamate signaling in melanocytic neoplasia. Nat Genet 2003; 34: 108–112.
Dhanasekaran N, Heasley LE, Johnson GL : G protein-coupled receptor systems involved in cell growth and oncogenesis. Endocr Rev 1995; 16: 259–270.
Takano T, Lin JH, Arcuino G, Gao Q, Yang J, Nedergaard M : Glutamate release promotes growth of malignant gliomas. Nat Med 2001; 7: 1010–1015.
Rzeski W, Turski L, Ikonomidou C : Glutamate antagonists limit tumour growth. Proc Natl Acad Sci USA 2001; 98: 6372–6377.
Berwick M, Armstrong BK, Ben-Porat L et al: Sun exposure and mortality from melanoma. J Natl Cancer Inst 2005; 97: 195–199.
Sasieni PD : From genotypes to genes: doubling the sample size. Biometrics 1997; 53: 1253–1261.
Bastian BC, Olshen AB, LeBoit PE, Pinkel D : Classifying melanocytic tumours based on DNA copy number changes. Am J Pathol 2003; 163: 1765–1770.
Curtin JA, Fridlyand J, Kageshita T et al: Distinct sets of genetic alterations in melanoma. N Engl J Med 2005; 353: 2135–2147.
Maldonado JL, Fridlyand J, Patel H et al: Determinants of BRAF mutations in primary melanomas. J Natl Cancer Inst 2003; 95: 1878–1890.
Cohen C, Zavala-Pompa A, Sequeira JH et al: Mitogen-activated protein kinase activation is an early event in melanoma progression. Clin Cancer Res 2002; 8: 3728–3733.
Marin YE, Chen S : Involvement of metabotropic glutamate receptor 1, a G protein coupled receptor, in melanoma development. J Mol Med 2004; 82: 735–749.
Marin YE, Namkoong J, Cohen-Solal K et al: Stimulation of oncogenic metabotropic glutamate receptor 1 in melanoma cells activates ERK1/2 via PKCepsilon. Cell Signal 2006; 18: 1279–1286.
Acknowledgements
We thank the melanoma patients and controls for their participation in this study. We also thank Ana Salinas and Carmen Rivero for their technical support. Neocodex have been partially funded by the Ministerio de Ciencia y Tecnología of Spain (FIT-010000-2004-68, FIT-010000-2004-69 and PTQ2004-0718).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ortiz, P., Vanaclocha, F., López-Bran, E. et al. Genetic analysis of the GRM1 gene in human melanoma susceptibility. Eur J Hum Genet 15, 1176–1182 (2007). https://doi.org/10.1038/sj.ejhg.5201887
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejhg.5201887
Keywords
This article is cited by
-
Metabotropic glutamate receptor 1 acts as a dependence receptor creating a requirement for glutamate to sustain the viability and growth of human melanomas
Oncogene (2015)
-
Glutamate and its receptors in cancer
Journal of Neural Transmission (2014)
-
Systematic analysis of somatic mutations in phosphorylation signaling predicts novel cancer drivers
Molecular Systems Biology (2013)
-
A polymorphism (rs2073287) of glutamate receptor, metabotropic 1 (GRM1) is associated with an increased risk of stroke in Korean population
Molecular & Cellular Toxicology (2011)