Key Points
-
In general a significant decrease in marginal accuracy should be taken into consideration for partial coverage restorations after adhesive cementation.
-
Adhesive luted partial coverage restorations appear to have a moderate increase in marginal gap width under masticatory ageing.
-
The introduced new preparation designs fulfil the technical demands to fabricate accurate fitting all ceramic partial coverage restorations.
Abstract
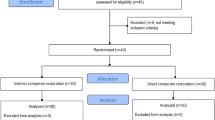
Objectives To determine the influence of the preparation design and the dimensions of all-ceramic partial coverage restorations (PCR) on the marginal accuracy before and after masticatory simulation.
Methods In this in vitro study 80 extracted human maxillary molars were restored with MOD inlay restorations and four different modified PCR restorations using a new press ceramic IPS e.max® Press (IPS e.max® Press VP 1989). The teeth were divided into five groups of 16 specimens each and prepared as follows: Group A received an MOD inlay preparation and Group B, C, D and E received modified PCR. The restorations were adhesively luted and exposed to a mastication simulator. The discrepancies of the marginal fit were examined on epoxy replicas before and after luting as well as after masticatory simulation at 200× magnification.
Results The mean (geometrical) [95% confidence limits] marginal gap decreased from Group A to E before cementation (A-83[77-90]μm, B-68[65-70]μm, C-59[55-64]μm, D-56[52-61]μm, E-50[45-55]μm). Group A had significantly higher marginal gap values than group B (p = 0.017) and the other groups (p<0.0001). After cementation the marginal accuracy was recorded as following: A-103[93-114]μm, B-101[94-108]μm, C-93[89-98]μm, D-102[98-105]μm and E-99[96-102]μm. Cementation increased the marginal gap in groups B-E significantly (p<0.00001), not significantly in group A (p = 0.059). Artificial ageing (A-116[106-127]μm, B-114[109-120]μm, C-106[103-110]μm, D-109[100-118]μm and E-109[105-112]μm) led to further significant decrease of marginal accuracy in Group B (p = 0.029) and C (p = 0.026) only. After cementation and masticatory simulation of the ceramic restorations, the marginal gap values of Groups A, B, C, D and E did not significantly differ from each other (p = 1.00).
Conclusions The result of this in vitro study showed that IPS e.max® Press can be used to fabricate all-ceramic inlays and PCR which meet the requirements in terms of a clinically acceptable marginal gap, irrespective of the preparation design used. However, the preparation design and dimensions of the restorations appeared to affect the initial marginal fit and flowing off of luting material during the cementation process. The factors responsible for these findings require further substantiation.
Similar content being viewed by others
Introduction
The increasing awareness of aesthetics among patients and the growing concerns about amalgam restorations have led to an increase in the demand for alternative restorative materials in the posterior region as well as in the anterior region. Innovative dental ceramic systems provide such an alternative, because they can fulfil both functional and aesthetic requirements. These systems often involve new processing technologies and not all of them have yet been conclusively evaluated in terms of their clinical performance. Dental ceramic materials provide essential advantages over metal-ceramic and gold restorations. Not only do they offer superior aesthetic properties but also increased biocompatibility with tissues of the periodontium and pulp1 as well as a radiopacity which is similar to that of the natural tooth structure. At present, five different categories of fabrication techniques for creating all-ceramic partial crowns are known: form sintering (eg In-Ceram Spinell), casting (eg Dicor), heat pressing (eg IPS Empress), copy milling (eg Celay) and CAD/CAM processing (eg Cerec). The present study used a new all-ceramic material IPS e.max® Press. The material in question is a pressed ceramic from Ivoclar Vivadent AG, Schaan, Liechtenstein (IPS e.max® Press VP 1989). This pressed ceramic is intended to expand the range of indications of Empress® 2 (Ivoclar Vivadent AG, Schaan, Liechtenstein). While it features similar physical properties as the latter, its translucency has been improved. The IPS e.max® Press system encompasses a high-stability framework material which consists of lithium disilicate (2 SiO-Li2O). The restorations can be customised either by using a layering technique based on fluorapatite glass ceramic or by using the staining technique. The marginal fit of restorations is of particular interest and is a quality criteria for the evaluation of dental restorative materials.2,3 A method for determining the marginal fit is to measure the marginal gap, i.e. the distance between the restoration margin and preparation margin. The methods and measurement units to determine the marginal gap of restorations are not validated.4 Furthermore, the definition of marginal fit scatters widely. To facilitate the comparison of the various studies described in the literature, Holmes5 postulated a standardised terminology to describe the various measurable marginal areas. The clinically acceptable values defined for marginal gaps vary between 20 μm and 200 μm.2,4,6,7,8,9 Table 1 provides an overview of the current studies on marginal gap formation in all-ceramic inlay restorations and partial crowns. Studies focusing only on partial crowns are currently in short supply. The goal of this in vitro study was to examine the marginal adaptation of pressed all-ceramic MOD inlay restorations and different PCR before and after adhesive cementation as well as after thermal cycling in an artificial oral environment. A standardised preparation protocol was used to prepare the teeth.
Material and method
Eighty extracted caries-free maxillary molars were used to do this study. After extraction, the teeth were stored in 0.1% thymol solution at room temperature for no longer than three months. Sixteen teeth were randomly allocated to one of the five test groups. The teeth were prepared according to a standardised protocol. Primary preparation was done with 80-μm grit preparation diamonds (837KR.314.012, 847KR.314.016), while finishing was done with finer diamonds (30-40-μm grain size, 8837KR.314.012, 8847KR.314.016, 8390204016, Komet, Dental, Gebr. Brasseler, Lemgo, Germany).
In none of the groups was a bevel, or a retentive preparation pattern, used. The angle between the reduced cusp surface and the uncut outer tooth edge was on average 100 degrees. All internal angles were slightly rounded out (Figs 1,2,3,4 to 5). Preparations were done freehand by one practitioner.
Group A: MOD inlay preparation. Width and depth: 3 mm. Overall preparation angle: 6 degrees. The proximal boxes ended 1 mm short of the cemento-enamel junction (basic preparation).
Group B: Basic preparation and reduction of the mesiopalatal cusp by 2 mm according to the anatomical shape of the occlusal surface.
Group C: Basic preparation and reduction of the mesiopalatal and distopalatal cusps by 2 mm according to the anatomical shape of the occlusal surface.
Group D: Basic preparation and reduction of mesiopalatal, distopalatal and distobuccal cusps by 2 mm according to the anatomical shape of the occlusal surface.
Group E: Basic preparation and reduction of all four cusps by 2 mm according to the anatomical shape of the occlusal surface.
Impressions of the abutment teeth were taken using the double mixing technique with Permagum® Putty Soft (3M Espe, Seefeld, Germany) and Dimension® Garant L (3M Espe, Seefeld, Germany). The impressions were poured with GC FujiRock® EP (Type 4 dental stone, GC Europe, Leuven, Belgium). By the use of die hardener (Margidur®, DUS Dental-U Inc, Richmond, Canada) critical line angles along the preparation margin were strengthened and their mechanical resistance enhanced. Die spacer (Purargent 20mL®, DUS Dental-U Inc, Richmond, Canada) was applied to the cavity surfaces (approximately 10 μm) in 1.5 mm distance to the marginal areas. The all-ceramic restorations were fabricated by Ivoclar Vivadent AG, Schaan, Liechtenstein.
To fabricate the restorations, wax patterns were invested in Empress®2 Speed investment material (Ivoclar Vivadent AG, Schaan, Liechtenstein). The preheating cycle was carried out in a preheating furnace (Type 5636; KaVo Dental GmbH, Biberach, Germany), at a temperature of 850°C for 60 minutes. Subsequently, the moulds were transferred to the EP 500/V2.9 ceramic furnace (Ivoclar Vivadent AG, Schaan, Liechtenstein) and pressure filled with IPS e.max® Press VP1989/4 ingot material, at a temperature of 915°C for 20 minutes. After divestment and separation of the restoration, two glaze firing cycles were done in the Programat P100 furnace. For this purpose, C27688 Empress®2 glazing material (Ivoclar Vivadent AG, Schaan, Liechtenstein) was applied and fired, using a firing temperature of 770±10°C for six minutes. After the dental laboratory had fabricated the restorations, they were placed on the prepared teeth to check the fit using Bite Checker® (GC Europe NV, Leuven, Belgium). Interferences on the internal aspects of the ceramic restorations were removed under water cooling, using a high-speed angled handpiece and fine-grain diamonds. The ceramic restorations were adhesively cemented using Variolink®II dual-curing fine-particle hybrid composite (high viscosity) (Ivoclar Vivadent AG, Schaan, Liechtenstein).
Teeth were etched with Total Etch® and conditioned with Syntac® Classic (Ivoclar Vivadent AG, Schaan, Liechtenstein) for this purpose. The inner surfaces of the ceramic restorations were etched with IPS Ceramic etching gel® for 20 seconds and then silanized with Monobond S® (Ivoclar-Vivadent AG, Schaan, Liechtenstein). The specimens were light-polymerized with at least a 650 mw/cm2 light intensity (Elipar Free Light 2; 3M ESPE, Seefeld, Germany).
Gross excess material was removed using a curette and resin pellets. Liquid Strip® glycerine gel (Ivoclar Vivadent AG, Schaan, Liechtenstein) was applied along the margins of the cement joint to prevent an oxygen inhibition layer forming during the light-curing process. After the polymerization procedure was completed, remaining excess of cement was removed using a 15c scalpel (#371716, Bard-Parker; Becton-Dickinson, Dr Franklin Lakes, NJ, USA), and subsequently flexible polishing discs (Sof-Lex Pop-On®, 3M Medica, St. Paul, USA). To imitate the physiological mobility of teeth and biological width, an artificial periodontal membrane was applied using an anti-slip varnish (Anti-Rutsch Lack, Wenko-Wenslaar GmbH, Hilden, Germany). The varnish was applied in a uniform coating of 0.3-0.5 mm on the entire root surface up to 2 mm below the cemento-enamel junction using a disposable brush. The abutments were affixed to the specimen holders to ensure that they were facing a defined direction in the mastication simulator. The tooth axis was aligned perpendicularly to the specimen holder and the occlusal surfaces were set horizontally to the bottom of the holder. The specimens were inserted into the specimen holders up to 2 mm below the cemento-enamel junction using Technovit 4000® (Heraeus-Kulzer GmbH & Co. KG, Wehrheim, Germany), a fast-curing cold-mounting three-component resin. Subsequently, the teeth were subjected to cyclic thermal mechanical loading. For this purpose, 1.2 million loading cycles were performed at a frequency of 1.6 Hz and a force of 98 N, using steatite balls, which were aligned on the centre of the occlusal surface of the molars. In addition, the specimens were exposed to thermal cycling at temperatures of 5°C and 55°C (5300 cycles in total). This in vitro test simulated five years of clinical service.10,11
An impression of all the ceramic restorations was taken before and after cementation as well as after artificial ageing in the mastication simulator to examine marginal adaptation. Before cementation, the partial coverage restorations were held in place with a small amount of Variolink®II Try-In paste (Ivoclar Vivadent AG, Schaan, Liechtenstein) during the impression procedure. The impressions were created with Permagum® Putty Soft (3M-Espe, Seefeld, Germany) and Dimension® Garant L (3M-Espe, Seefeld, Germany) and poured with expoxy resin (Epon 812, Sigma Chemie, Munich, Germany). The impressions were degassed in a furnace at 60°C for 24 hours to obtain bubble-free replicas. The epoxy resin was processed according to the manufacturer's instructions and the impressions were filled with liquid material, making sure not to incorporate any bubbles. While the epoxy resin was still liquid, the impressions were placed back into the furnace and stored at 60°C for 24 hours until complete polymerisation. Upon completion of the polymerisation process the replicas were removed from the moulds and the basal surfaces and margins trimmed using an acrylic cutter. The replicas were centred and mounted on prefabricated aluminium sample holders using cyanoacrylate adhesive to examine them under a stereo light microscope. The replicas were coated with a thin gold layer of 200 Å in a high-vacuum sputter device (SCD 050, Bal-Tec GmbH, Witten, Ruhr, Germany) to obtain an accurate picture of the marginal gaps (Fig. 6).
Marginal gap analysis was done under a stereo light microscope from Zeiss (Stemi 2000 CS; Carl Zeiss, Jena, Germany) using 200x magnification, a 3 CCD colour video camera from Sony (Cologne, Germany) and an IBM compatible PC equipped with a Microsoft NT 4.0 operating system. Analysis 3.0 (Soft-Imaging Software GmbH, Munich, Germany) served as the image analysis programme. The marginal discrepancies were measured at intervals of 100 μm around the circumference of the restoration margins. The number of points measured in each tooth varied, because human maxillary molars, which slightly differ in shape and size from each other, were used in the present study. For statistical analysis belonging measurements (between 400 and 500 points for each tooth) were averaged for each specimen. Based on these averaged marginal gap values, means and confidence intervals for assessing marginal accuracy were computed for each group and for all stages (initial, cemented, aged) of the investigation. The logarithmic transformation is an approved method for robust statistical inference on location of data that originate from skewed distributions. It leads to a stabilisation of variance estimators. Therefore, location was estimated by geometric means instead of more familiar arithmetic means. Estimation of confidence intervals and t-test were based on logarithmically transformed values also. To achieve a global level of significance (α=0.05) the p-values resulting from pairwise comparisons of unpaired t-tests (between groups) and paired t-tests (between stages) were corrected by the Bonferroni-Holm method. (Statistical software: R Development Core Team (2004). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3-900051-00-3).
Results
Marginal gap analysis of the specimens resulted in the following mean (geometrical) (CI-95%) values before cementation, after cementation and after masticatory simulation: Group A: 83[77-90]μm, 103[93-114]μm and 116[106-127]μm; Group B: 68[65-70]μm, 101[94-108]μm and 114[109-120]μm; Group C: 59[55-64]μm, 93[89-98]μm and 106[103-110]μm; Group D: 56[52-61]μm, 102[98-105]μm and 109[100-118]μm and Group E: 50[45-55]μm, 99[96-102]μm and 109[105-112]μm. Descriptive statistics are displayed in Tables 2,3,4 along with geometric means and confidence limits, see also Figure 7.
Before cementation, the mean (geometrical) marginal gap width consistently decreased, as the dimensions of the restorations increased from Group A to Group E (Table 2). Group A had significantly higher marginal gap values than group B (p = 0.017) and the other groups (p<0.0001). Group E (PCR-4 cusps) showed significant lower marginal gap values than Group B (PCR-1 cusp) (p = 0.0002).
After the cementation of the ceramic restorations, the groups A, B, C, D and E did not significantly differ from each other (p>0.05) (Table 3). Cementation increased the marginal gap in groups B-E significantly (p<0.00001), not significantly in group A (p = 0.059).
After masticatory simulation the marginal gap values of all groups did not demonstrate any significant differences (p>0.05) (Table 4). Compared to marginal gap values after cementation masticatory loading led to further decrease of marginal accuracy in Group B (p = 0.029) and C (p = 0.026) significantly, not statistically significant in the remaining groups (p>0.05).
Discussion
In vitro and in vivo studies that have examined the width of the marginal gap of all-ceramic partial coverage restorations are in short supply.12,13,14 Direct comparisons between published studies are very limited due to the differences in the study set-ups and statistical analyses.
The dental laboratory procedures, the manual skills and the experience of the dental technician have a decisive influence on the marginal gap width. Consequently, all restorations employed in the present study were fabricated by the same master technician to ensure that these factors did not change for the individual test groups. The fine-particle hybrid luting composite Variolink®II (Ivoclar Vivadent, AG, Schaan, Liechtenstein) was used to cement the restorations because this composite has been reported to have produced the best marginal quality in relevant studies.15,16,17 Replica technology was used to monitor the changes in marginal gap width in the course of the investigation. The replica technique is less costly and time consuming for the user to create test specimens than other methods (eg cross section preparation technique). However, the replica technique cannot be used to examine the microleakage and disintegration of luting composite in the cement joint.
The marginal gaps measured for all five test groups before cementation, after cementation and after artificial aging were on average in the range of 120 μm, a value defined as clinically acceptable.7 After cementation, the cement joints of the restorations were on average thicker than the 50–100 μm described by Molin18 in 1996 as being ideal for achieving a strong bond between the ceramic and resin composite.
Before cementation, significantly larger mean cement joints were measured in the specimen that were restored with conventional inlay restorations (Group A) than in the ones that were restored with modified PCR. The mean thickness of the cement joints gradually decreased as the number of cusps included in the restorations increased. The smallest mean cement joint was measured in PCR that involved four cusps (Group E). The height of the occlusal isthmus was lower in the partial coverage preparations than in the inlay preparations due to the reduction of the cusps. The reduced height of the isthmus may have decreased the risk of jamming, or inappropriately high friction during insertion. It remains to be examined whether the marginal fit can be improved by increasing the divergence of the overall preparation angle (>6°) in the occlusal box. The literature currently available does not include any data on this issue. A study by Denissen12 also examined the marginal fit of all-ceramic PCR before cementation. This study used an experimental preparation design. The molars were prepared with deep gingival chamfers in the proximal boxes and around the functional cusps. The non-functional cusps were prepared with broad bevels. The marginal gap of 25 partial crowns, which were fabricated with different CAD/CAM systems, was measured on stone dies prior to cementation. The mean marginal gaps of the Cicero, Cerec and Procera onlays on the stone dies were 74 μm, 85 μm and 68 μm respectively. These values are slightly higher than the mean marginal gaps measured for Group B (68 μm), C (60 μm), D (57 μm) and E (51 μm) of the present study.
Denissen12 reported a mean cement width of 81 μm after the partial crowns had been cemented in place. This value is lower than the marginal gap measured after the cementation of the partial coverage restorations used in the present study. Gemalmaz19 also described an increase in the marginal gap of ceramic inlays after cementation. In the present study, a significant increase in marginal gap width was observed for all partial coverage restorations after adhesive cementation. The lowest increase in mean marginal gap width after cementation was recorded for Group A (20 μm), followed by Group B (34 μm), C (34 μm), D (45 μm) and E (49 μm). Basically, the increase in marginal gap width is caused by the volume requirement of the luting cement, depending on particle size, flow properties, and consistency.15,16 Hence, the large initial gap, which facilitates the flowing off of luting material during the cementation process, may explain why the cement width increased to a lesser degree in Group A than it did in the other groups. Conversely, Group E, which showed the best initial fit, produced the largest increase in marginal gap after cementation. The good initial fit and the size of the restoration surface may have diminished the capability of the luting composite to flow off and consequently may have been conducive to increasing the cement width of this group. After masticatory simulation and thermal cycling, a significant increase of the marginal gap was observed for Group B (p = 0.029) and C (p = 0.026) only. Nevertheless, a trend towards decrease of marginal accuracy after fatigue was demonstrated in all groups. Numerous in vivo studies have provided evidence that the marginal quality of ceramic restorations tends to deteriorate over the years after adhesive cementation.20,21,22,23,24 The increase in marginal gap width after thermal cycling and artificial aging may be attributed to hydrolytic and mechanical stresses. The luting composite may absorb water and the resultant expansion in volume may lead to an increase in marginal gap width. However, the median marginal gaps of the test groups were slightly below the clinically acceptable marginal gap of 120 μm7 even after thermal cycling and masticatory simulation.
Conclusions
The results of this in vitro study showed that the press ceramic IPS e.max® Press (VP 1989) can be used to fabricate inlays and partial crowns which meet the requirements in terms of a clinically acceptable marginal gap, irrespective of the preparation design used. However, the preparation design and dimensions of the restorations appeared to affect the initial marginal fit and flowing off of luting material during the cementation process. The factors responsible for these findings require further substantiation. A clinical trial on the new preparation designs and materials is desirable.
References
Anusavice KJ . Degradability of dental ceramics. Adv Dent Res 1992; 6: 82–89.
Rehberg HJ . Exact marginal accuracy — what does that mean? Dtsch Zahnärztl Z 1971; 26: 696–699.
Noack MJ . Adaptation of composite-, glass-ceramic- and ceramic-inlays. Dtsch Zahnärztl Z 1994; 49: 873–878.
Kerschbaum T . Standardized margin of the restoration? — Results from the clinical point of view. In Walther W (ed) Qualitätssicherung in der Zahnheilkunde. pp 19–45. Heidelberg: Hüthig GmbH, 1995.
Holmes JR, Bayne SC, Holland GA et al. Considerations in measurement of marginal fit. J Prosthet Dent 1989; 62: 405–408.
Dreyer Jorgensen K. Testing results of dental casting techniques. Dtsch Zahnäztl Z 1958; 13: 461–649.
McLean JW, Von Fraunhofer JA . The estimation of cement film thickness by an in vivo technique. Br Dent J 1971; 131: 107–111.
Marxkors R . Marginal accuracy of gold crowns. Dtsch Zahnärztl Z 1980; 35: 913–915.
Spiekermann H . Crown restorations and periodontal tissue response. In Lange D E (ed) Parodontologie, Implantologie und Prothetik im Brennpunkt von Praxis und Wissenschaft. pp 209–233. Berlin: Quintessenz, 1985.
Delong R, Douglas WH . Devlopment of an artificial oral environment for the testing of dental restoratives: bi-axial force and movement control. J Dent Res 1983; 62: 32–36.
Sakaguchi RL, Douglas WH, De Long R et al. The wear of a posterior composite in an artificial mouth: a clinical correlation. Dent Mater 1986; 2: 235–240.
Denissen H, Dozic A, Van DerZelJ, M VW . Marginal fit and short-term clinical performance of porcelain-veneered CICERO, CEREC and PROCERA onlays. J Prosthet Dent 2000; 84: 506–513.
Hürzeler M, Zimmermann E, Mörmann WH . The marginal adaptation of mechanically produced onlays in vitro. Schweiz Monatsschr Zahnmed 1990; 100: 715–720.
Schäfers F, Järschke J, Meyer G . Accuracy of fit of different all-ceramic procedures. ZWR 1994; 103: 686–689.
Lang R, Rosentritt M, Behr M, et al. The influence of modified glass ionomer cement, polyacid modified composite- and composite resin on the marginal accuracy of ceramic inlays. Dtsch Zahnärztl Z 2000; 55: 540–543.
Gemalmaz D, Ozcan M, Alkumru HN . A clinical evaluation of ceramic inlays bonded with different luting agents. J Adhes Dent 2001; 3: 273–283.
Lafuente JD, Chaves A, Carmiol R . Bond strength of dual-cured resin cements to human teeth. J Esthet Dent 2000; 12: 105–110.
Molin MK, Karlsson SL, Kristiansen MS . Influence of film thickness on joint bend strength of a ceramic/resin composite joint. Dent Mater 1996; 12: 245–249.
Gemalmaz D, Özcan M, Yoruc AB et al. Marginal adaptation of a sintered ceramic inlay system before and after cementation. J Oral Rehabil 1997; 24: 646–651.
Felden A, Schmalz G, Federlin M, et al. Retrospective clinical study and survival analysis on partial ceramic crowns: results up to 7 years. Clin Oral Invest 2000; 4: 199–205.
Isenberg BP, Essig ME, Leinfelder KF . Three-year clinical evaluation of CAD/CAM restorations. J Esthet Dent 1992; 4: 173–176.
Krämer N, Frankenberger R, Pelka M, et al. IPS EMPRESS inlays and onlays after four years — a clinical study. J Dent 1999; 27: 325–331.
Otto T, De Nisco S . Computer-aided direct ceramic restorations: a 10-year prospective clinical study of Cerec CAD/CAM inlays and onlays. Int J Prosthodont 2002; 15: 122–128.
Felden A, Schmalz G, Hiller K-A . Retrospective clinical investigation and survival analysis on ceramic inlays and partial ceramic crowns: results up to 7 years. Clin Oral Invest 1998; 2: 161–167.
Hahn R . Experimental investigations of reproducible fitting accuracy of ceramic inserts. Dtsch ZahnärztlZ 1990; 45: 653–656.
Siervo S, Bandettini B, Siervo P et al. The CELAY system: a comparison of the fit of direct and indirect fabrication technique. Int J Prosthodont 1994; 7: 434–439.
Siervo S, Pampalone A, Siervo P, et al. Where is the gap? Machinable ceramic systems and conventional laboratory restorations at a glance. Quintessence Int 1994; 25: 773–779.
Mörmann WH, Schug J . Grinding precision and accuracy of fit aof CEREC 2 CAD/CIM inlays. J Amer Dent Assoc 1997; 128: 47–53.
Sturdevant JR, Bayne SC, Heymann HO . Margin gap size of ceramic inlays using second-generation CAD/CAM equipment. J Esthet Dent 1999; 11: 206–214.
Acknowledgements
The authors would like to acknowledge M. Hans-Peter Foser, Master Dental Technician, Ivoclar-Vivadent AG, Schaan, FL, for his effort in the fabrication of the ceramic restorations for this study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Stappert, C., Denner, N., Gerds, T. et al. Marginal adaptation of different types of all-ceramic partial coverage restorations after exposure to an artificial mouth. Br Dent J 199, 779–783 (2005). https://doi.org/10.1038/sj.bdj.4813036
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4813036
This article is cited by
-
Comparative evaluation of internal fit and marginal gap of endocrowns using lithium disilicate and polyether ether ketone materials - an in vitro study
BMC Oral Health (2023)
-
Digital dentistry: an overview of recent developments for CAD/CAM generated restorations
British Dental Journal (2008)
-
Full ceramic restorations in posterior teeth
British Dental Journal (2005)