Key Points
-
This paper illustrates an effective means of providing a provisional restoration for a missing single tooth.
-
The Rochette design remains useful as it permits simple removal and replacement during implant treatment.
-
The provisional Rochette bridge can use an adjacent tooth or a distant tooth as an abutment.
-
The Rochette bridge has a probability of survival of 80% after 200 days.
Abstract
A retrospective clinical audit of the role and survival of 69 Rochette bridges used as immediate provisional restorations for single tooth, implant-retained crowns was carried out over the period between February 1991 and May 2001. In each case the extracted tooth was immediately temporised using a Rochette bridge with a single wing and pontic and cemented to the abutment tooth without any tooth preparation (Phase I). This bridge was removed at the time of implant placement and recemented (Phase II). At the implant exposure stage the bridge was removed and discarded. In Phase I, 15.9% of the bridges required recementation and 27.5% of the bridges required recementations in phase 2; 7.2% of the bridges required recementations in both phases. An 80% probability of survival was noted after an interval of 200 days for phase I and a 78% probability of survival over the same time interval was observed for Phase II. A significant debond rate was observed when the retainer was a canine in comparison to the other bridges in Phase I. In Phase I the spring cantilever debond rate was significantly higher than that observed on the other bridges. More debondings were observed in males (25.8%) compared with females (7.9%) in Phase I. More debondings were noted in the maxilla than in the mandible in Phase II. The performance characteristics of the metal acrylic Rochette bridge observed in this report supports the conclusion that this type of restoration is an effective means of immediate temporisation for patients undergoing single tooth implant retained restorations.
Similar content being viewed by others
Introduction
The evolution of implant-supported rehabilitation of the edentulous patient is well documented in the dental literature. The replacement of missing teeth with implant-retained restorations is becoming a popular treatment option for both the clinician and the patient. The predictability of implants and associated soft tissue surgical techniques provide the patient with desirable, functional and aesthetic results. Although immediate implant placement and loading is possible, there are certain clinical situations where a staged technique is indicated and therefore a provisional restoration is required to maintain aesthetics and function.1,2
Rochette3 was the first to describe the use of a resin-bonded prosthesis for the splinting of periodontally mobile teeth using a perforated, cast metal framework that was cemented with acrylic resin to acid etched enamel. Later Howe and Denehy4 described a technique that used a cast metal perforated bridge framework with clinical success5 and such restorations have subsequently come to be known as Rochette bridges. Wise6 illustrates an acid etch retained provisional bridge which removes the need to prepare non-restored teeth or compromise the anterior occlusion. He suggests that if the occlusion permits, to confine the retainer to the lingual surface of the abutments and the use of a Rochette bridge so that removal can be readily accomplished by cutting through the resin tags.
Many workers7,8,9,10,11,12 have commented upon the advantages and features of fixed provisional restorations during implant treatment. These include: patient acceptability, diagnostic value, loading and oral hygiene, tooth tissue conservation, retrievability and predictability.
The aim of this audit was to investigate the survival of Rochette bridges when used as provisional restorations during implant treatment.
Materials and methods
A total of 69 patients' records were selected from the records of all 150 patients who had received implant treatment for a single tooth, implant-retained crown over the period between February 1991 and May 2001. The criteria for selection were that a single tooth had to be replaced with an implant retained restoration and an immediate Rochette bridge had been constructed prior to the extraction of the tooth and cemented immediately after the tooth had been extracted. All patients fulfilling the selection criteria were included in the study. The bridge was held in place by one retainer tooth only, which was selected prior to the tooth being extracted from the study models, usually an adjacent tooth (n = 62). For the remainder (n = 7), a spring cantilever design was selected where the adjacent tooth was deemed unsuitable for occlusal reasons or due to inadequate potential bonding surface area. The age of the patient was recorded as the number of years nearest the date when treatment started.
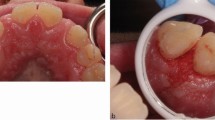
Figure 1 shows an example where tooth 22 has a root fracture and is to be extracted. An immediate provisional Rochette restoration has been placed (Fig. 2). This has been cantilevered from tooth 21 (Fig. 3) due to the occlusion at 23. In another example (Fig. 4) tooth 11 has external cervical resorption which has become visible labially. Following extraction using luxators a spring cantilever Rochette was fitted (Fig. 5). After a period of healing the Rochette provisional bridge was removed and the implant site prepared (Fig. 6). The Rochette provisional bridge was refitted and after a further period of healing it was again removed to allow exposure of the fixture (Fig. 7). The final restoration, an implant retained crown, is shown in Figure 8.
Patients had the single tooth extracted and replaced immediately with an adhesive Rochette bridge and subsequently by an implant retained crown. The same bridge was used throughout the duration of the treatment. At the time of extraction the bridge was cemented in place using Super C cement (AMCO International, 2 Union Hill Road, West Conshohocken, PA 19428, USA). The same cement was used to replace the bridge after implant fixture placement and during any recementation procedure. This treatment was all carried out by a single clinician. A second surgeon who placed all the implant fixtures carried out the recementation of the bridge at the time of surgery. The occlusal records were provided to the technician by indicating some strategic teeth, which held shimstock foil on closure. The tooth to be extracted was removed from the cast and the bridge constructed. The same technician was involved in the making of the all the bridges, which were constructed from non-precious alloy and K&B acrylic (Dentsply).
Rubber dam was not used during the cementation procedure. If bone grafting techniques or soft tissue manipulation was required at the fixture placement appointment then the acrylic pontic was suitably adjusted as required. After the tooth was extracted and the haemorrhage controlled the retainer tooth was etched with 37% phosphoric acid for one minute. A small amount of the liquid component of the cement was applied to the fitting surface of the bridge before cementation. The bridge was positioned and held in place until the cement had set and the excess cement removed with polishing burs in a high-speed handpiece. Occlusal contacts were checked with shim stock, comparing centric holding stops before and after cementation, to exclude changes to the occlusion.
Patients were reviewed after two weeks. At the implant placement appointment the bridge was removed from the retainer tooth by removal of the cement from the hole areas of the wing with use of a round diamond bur in a high-speed handpiece and displacing the bridge with a spring loaded crown and bridge remover. The cement present on the surface of the tooth was not removed to avoid enamel loss. However cement remaining on the wing was removed with a diamond bur at high speed. The cement area on the tooth was cleaned by etching using 37% phosphoric acid and the bridge recemented as before. The bridge was finally removed and discarded at the implant exposure appointment and the retainer tooth smoothed. The recementation technique, if the bridge prematurely dislodged, was the same as described above.
Phase I refers to the period between the bridge being placed immediately after tooth extraction and the appointment when the bridge was removed for the implant to be placed and the same bridge recemented. Phase II was the period between the implant being placed (and the bridge being recemented) and the appointment when the implant was exposed and the bridge removed and no longer required.
All patients completed the treatment. The date when the bridge dislodged prematurely was recorded, ie before the date when the implant was placed or exposed. None of the bridges involved required cementation more than once during either phase.
Calculations were undertaken using the SPSS computer programme (www.spss.com). Kaplan-Meier probabilities of survival13,14 were calculated and plotted. An analysis of variance table14,15 was constructed to calculate the F-ratio value, which was compared with critical values given in a table of the F distribution.14
The variants that were considered were:
-
1
Bridges requiring recementations during Phase I, Phase II or both phases. Survival of the bridges where the duration of Phase 1 and Phase 2 was greater than 180 days.
-
2
Recementations required for bridges which had a canine tooth as a pontic both during Phase I and Phase II.
-
3
Recementations required for bridges which had a canine tooth as a retainer both during Phase I and Phase II.
-
4
Recementations required during both phases for bridges which had a posterior tooth as a pontic.
-
5
Comparisons between the bridges placed in the mandible and the maxilla.
Recementations for spring cantilever bridges during both phases.
-
1
The age groupings of the patients: below 40 years, 40-55 years and above 55 years.
-
2
Recementations required during both phases according to gender.
The implant surgeon determined the time for the implant placement and exposure as six months therefore the mean survival times of the bridges were not calculated.
Results
-
1
Bridges requiring recementations during Phase I, Phase II and both phases. Of the 69 bridges in the study 11 (15.9%) bridges required recementations during Phase I. Nineteen bridges required recementing (27.5%) during Phase II and 5 (7.2%) of the bridges required recementation during both phases.
The Kaplan-Meier probabilities of survival (Fig. 9) showed that a cumulative probability of 0.84 was observed at 550 days for Phase I and that for Phase II was 0.70 in 300 days. The observed difference between the number of recementations between phase I and phase II was significant (P < 0.05) as seen in Table 1.
Figure 9: Kaplan-Meier probabilities of survival (all cases). -
2
Survival of the bridges where the duration of Phase I and Phase II was greater than 180 days. In Phase I the cumulative probability of survival of 0.70 was observed at 550 days and that in Phase II was observed at 0.76 at 300 days.
Figure 10 illustrates the Kaplan-Meier probabilities of survival comparison between Phase I and Phase II where the duration was greater than 180 days. Lt1 (cumulative probability of survival during phase I of treatment determined from the Kaplan-Meier table for duration over 180 days only) and Lt2 (as Lt1 but for phase II of treatment) plotted against time in days (T).
Figure 10: Kaplan-Meier probabilities of survival comparison of Phase I and Phase II. Kaplan-Meier probabilities of survival comparison between Phase I and Phase II where the duration was greater than 180 days. Lt1 (cumulative probability of survival during Phase I of treatment determined from the Kaplan-Meier table for duration over 180 days only) and Lt2 (as Lt1 but for Phase II of treatment) plotted against T.
-
3
Recementations required for bridges which had a canine tooth as a pontic during Phase I and Phase II A total of seven bridges out of the 69 had the pontic as a canine tooth. None of these required recementations in Phase I and II required recementation in Phase II.
-
4
Recementations required for bridges which had a canine tooth as a retainer both during Phase I and Phase II The canine tooth was used as a retainer for eight bridges. Four required recementations in Phase I compared to three in Phase II.
The difference observed between the proportion of bridges requiring recementations where the retainer was a canine and the other bridges was significant at a probability of 5% (Table 2).
-
5
Recementations required during both phases for bridges which had a posterior tooth as a pontic. Fifteen bridges out of the total 69 had the pontic as a posterior tooth and in both phases three required recementation (not significantly different from anterior bridges, P>0.05).
-
6
Comparisons between the mandible and the maxilla
A majority (61) of the bridges were placed in the maxilla out of which 10 required recementation during Phase I and 16 during Phase II. Out of the eight in the mandible one required recementation in Phase I and 3 in Phase II. The difference observed in Phase II was significant at a probability of 5%.
-
7
Recementations for spring cantilever bridges during both phases
Seven bridges were of the spring cantilever design and in Phase I, three required recementations compared with two in Phase II.
The difference observed between these bridges and the others requiring recementations during phase I was significant at the probability of 5% (Table 3).
-
8
Recementation and patient's age group. Twenty patients were below 40 years of age, 37 were between 40-55 and 12 were above 55. In Phase I recementation was required for two, four and five bridges respectively whereas in Phase II the numbers were seven, seven and five.
The difference observed between the age groups in Phase I was significant at a probability of 5% (Table 4).
-
9
Recementations required during both phases according to gender. There were 38 females and 31 males included in this study. During Phase I, three females and eight males required recementations and this was significant at a probability of 5%. In Phase II, seven females and 12 males required recementations. The difference observed between the genders for bridges that required recementations during Phase I is significant at a probability of 5%.
Discussion
This study investigated the clinical performance of the bridges used for the temporisation of single tooth replacements with implant retained prostheses. It has been reported that single abutment, single pontic, cantilever, resin bonded bridges have several advantages over multi-abutment resin bonded bridge designs16 and that cantilevers had a greater median survival than all other designs.17 De-bond rates of 20%,16 21%,18 17%19 and 32%15 have been reported. It has been proposed that the Rochette retainer design is more prone to debonding because of the relatively small retentive area per retainer, but the facility for easier removal, cleaning and rebonding is recognised.18
In this report 15.9% required recementations during Phase I, 27.5% required recementations during Phase II and 7.2% required recementations in both phases. The difference observed between the two phases was significant at 5%. Certain factors could contribute to the increased debond rate observed in Phase II:
-
1
Difficulty of moisture control post surgery. Moisture control is crucial for successful adhesive dentistry. However, it can be time consuming and often difficult to achieve.16 Placement of rubber dam adjacent to the surgical site, both at the extraction and the implant placement stage was difficult and rubber dam was not used.
-
2
Insufficient cleaning of the cement from the abutment tooth and wing. Cementation at the implant placement stage did not involve the removal of cement from the abutment tooth. The cement adherent to the fitting surface of the wing was removed using a diamond bur in an air turbine handpiece. Some authors20 have described thermal removal of composite resin from the wing.
-
3
Different surgery used and different operator. Creugers et al.21 compared bridges placed by five dentists and found no difference in retention rates while Marinello et al.22 have shown variable results:
-
a
Modifications made to the pontic to accommodate for hard/soft tissue surgical procedures.
-
b
Post operative swelling after implant surgery.
-
a
Creugers et al.23 have stated that the rebonded bridges (after first dislodgement) showed a significantly higher failure rate than the original bonded bridges. One of the probable reasons mentioned was that dislodgements (27%) were caused by biting or chewing hard food and instructions to the patient to avoid biting on hard objects would lower the failure rate. No such instructions were given to the patients in this study. They also concluded that a comparison of the failure characteristics of the 'first dislodgements' and 'second dislodgements' showed no correlation.
It has been suggested that excursive occlusal contacts should be avoided, if possible, on the pontic of cantilever resin bonded bridges16. However it has also been suggested24 that occlusal contacts had no significant adverse effect on survival, as the occlusal relationships originally prescribed were no longer present after a period of service. For all the bridges in the present study, no excursive contacts were prescribed on the pontics or the retaining wings. No statistically significant differences were observed in the debond rates according to pontic/retainer positions apart from when the abutment tooth was a canine, and in the cases of spring cantilever designs. In the cases where the abutment tooth was a canine, the surface area of retainer coverage was reduced so as to prevent any occlusal excursive contacts on the retainer and also to protect the adjacent tooth from wear. This would affect the survival of these bridges as the surface area is an important factor.6,24 The rigidity of the connector has also been described as an important feature for survival by the same authors therefore the spring cantilever design, with its reduced rigidity and increased leverage, would be expected to have its survival compromised.
Hussey et al.9 showed no difference in debond rates between patients under 30 years with those over 30. However Dunne and Millar18 had a significantly higher debond rate (46%) in the age band 11-20 years. They attributed this to the shorter clinical crowns, higher incidence of trauma and possibly a higher fluoride content in the enamel of children and young adults. In this report the youngest patient was 23 years of age. However in the age groups observed there was a significant difference in Phase I with the above 55 year group having a 41.67% debond rate. However the numbers involved were small (12, 20.9%).
Olin et al.5 noted that debondings were more frequent in men than in women. He suggests possible reasons to be physical factors such as the lower bite force experienced by women26 or perhaps to sociological factors. A significant difference was observed in this report for the debonding of the bridges according to gender in Phase 1 (males 25.8%, females 7.9%). In contrast other studies18,19 have found that gender was not a significant factor.
The position of the restoration in the dental arch was not found to be a significant factor in certain studies.18,24 In this report the debonding of the maxillary bridges was more than that observed in the mandibular arch in Phase II and this was statistically significant at the 5% confidence interval. One possible explanation for this could be the fact that maxillary implant placement surgery also involved grafting and other soft and hard tissue augmentations and manipulation in the majority of cases whereas none of the mandibular implants involved any supplemental surgical techniques. As a consequence of this the bridge pontic had to be adjusted to accommodate the new shape of the edentulous area. Studies have shown27 a higher failure rate in the lower arch.
Conclusions
From the results obtained the following conclusions can be made:
-
1
15.9% of the bridges required recementations in Phase I, 27.5% of the bridges required recementations in Phase II and 7.2% of the bridges required recementations in both phases.
-
2
An 80% probability of survival was observed after an interval of 200 days for Phase I and a 78% probability of survival over the same time interval was observed for Phase II.
-
3
A significant debond rate was observed when the retainer was a canine in comparison to the other bridges in Phase I.
-
4
Fewer debondings were noted in the maxilla than in the mandible in Phase II.
-
5
In Phase I the spring cantilever debond rate was significantly higher than that observed on the other bridges.
-
6
More debondings were observed in males (25.8%) compared with females (7.9%) in Phase I.
The performance characteristics of the metal acrylic Rochette bridge observed in this report supports the conclusion that this type of restoration is an effective means of immediate temporisation for patients undergoing single tooth implant retained restorations.
References
Szmukler-Moncler S, Piattelli A, Favero GA et al. Considerations preliminary to the application of early and immediate loading protocols in dental implantology. Clin Oral Implants Res 2000; 11:12–25.
Szmukler-Moncler S, Salama H, Reingewirtz Y et al. Timing of loading and effect of micromotion on bone-dental implant interface: review of experimental literature. J Biomed Mater Res 1998; 43: 192–203.
Rochette AL . Attachment of a splint to enamel of lower anterior teeth. J Prosthet Dent 1973; 30: 418–423.
Howe DF, Denehy GE . Anterior fixed partial dentures utilizing the acid-etch technique and cast metal framework. J Prosthet Dent 1977; 37: 28–31.
Denehy GE . Cast anterior bridges utilizing composite resin. Pediatr Dent 1982; 4: 44–47.
Wise MD . Failure in the restored dentition: Management and treatment. London: Quintessence Publishing, 1995.
Federick DR . Methods and materials for provisionalization in implant prosthodontics – Part 1. Dent Impl Update 1995; 6: 49–53.
Emtiaz S, Tarnow DP . Processed acrylic resin provisional restoration with lingual cast metal framework. J Prosthet Dent 1998; 79: 484–488.
Amet EM, Phinney TL . Fixed provisional restorations for extended prosthodontic treatment. J Oral Implantol 1995; 21: 201–206.
Breeding LC, Dixon DL . A bonded provisional fixed prosthesis to be worn after implant surgery. J Prosthet Dent 1995; 74: 114–116.
Zinner ID, Panno FV, Pines MS, Small SA . First-stage fixed provisional restorations for implant prosthodontics. J Prosthod 1993; 2: 228–232.
Chee WWL . Provisional restorations in soft tissue management around dental implants. Periodontol 2000; 27: 139–147.
De Kanter RJAM, Creugers NHJ, Verzijden CWGJM, Van'T Hof MA,. A five-year multi-practice clinical study on posterior resin-bonded bridges. J Dent Res 1998; 77: 609–614.
Bulman JS, Osborn JF . Statistics in dentistry. London: BDJ Books, 2000.
Gilmour ASM . Resin bonded bridges: a note of caution. Br Dent J 1989; 167: 140–142.
Shaw MJ, Tay WM . Clinical performance of resin-bonded cast metal bridges (Rochette bridges). Br Dent J 1982; 152:378–380.
Briggs P, Dunne S, Bishop K . The single unit, single retainer, cantilever resin-bonded bridge. Br Dent J 1996; 181:373–379.
Dunne SM, Millar BJ . A longitudinal study of the clinical performance of resin bonded bridges and splints. Br Dent J 1993; 174:405–411.
Hussey DL, Pagni C, Linden GJ . Performance of 400 adhesive bridges fitted in a restorative dentistry department. J Dent 1991; 19:221–225.
Haywood VB, Kanoy BE, Bruggers KJ, Andreaus SB . Thermal removal of composite resin: Effect on rebonding etched metal. J Prosthet Dent 1990; 63:289–291.
Creugers NHJ, Snoek PA, Van 'T Hof MA, Kayser AF . Clinical performance of resin-bonded bridges: a 5-year prospective study. 1. Design of the study and influence of experimental variables. J Oral Rehab 1989; 16:427–436.
Marinello CP, Kerschbaum TH, Heinenberg B et al. First experiences with resin-bonded bridges and splints – a cross-sectional retrospective study, part II. J Oral Rehab 1988; 15: 223–235.
Creugers NHJ, Snoek PA, Van 'T Hof MA, Kayser AF . Clinical performance of resin-bonded bridges: a 5-year prospective study. Part III. Failure characteristics and survival after rebonding. J Oral Rehab 1990; 17: 179–186.
Djemal S, Setchell D, King P, Wickens J . Long-term survival characteristics of 832 resin-retained bridges and splints provided in a post-graduate teaching hospital between 1978 and 1993. J Oral Rehab 1999; 26:302–320.
Olin PS, Hill EME, Donahue JL . Clinical evaluation of resin-bonded bridges: a retrospective study. Quint Int 1991; 22:873–877.
Okeson J . Management of temporomandibular disorders and occlusion. 2nd Ed. p 52. St Louis: CV Mosby Co, 1989.
Olin PS, Hill EM, Donahue JL . Resin bonded bridges: University of Minnesota recall data. J Dent Res 1990; 69: 362 abstr 2031.
Acknowledgements
This project forms the final part of the Masters of Clinical Dentistry (Prosthodontics) degree course run by the Guy's, King's and St. Thomas' Dental Institute at King's College London. Romesh Paul is thanked for his assistance with the statistics.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Banerji, S., Sethi, A., Dunne, S. et al. Clinical performance of Rochette bridges used as immediate provisional restorations for single unit implants in general practice. Br Dent J 199, 771–775 (2005). https://doi.org/10.1038/sj.bdj.4813027
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4813027
This article is cited by
-
Peri-implantitis. Part 3: Current modes of management
British Dental Journal (2014)
-
A review of the success and failure characteristics of resin-bonded bridges
British Dental Journal (2013)