Key Points
-
Diabetic patients should be treated first on a treatment session so that the start time is predictable. Hypoglycaemia must be avoided and presents more quickly than hyperglycaemia. A physician should be consulted if a general anaesthetic is being considered.
-
Thyroid disease may present as a goitre. Thyroid function should be stabilised before a general anaesthetic is used.
-
Oral contraceptives may predispose to thromboembolism and their action may be impaired by some antibiotics and anticonvulsants.
-
In pregnancy essential treatment should be carried out in the second trimester when possible.
-
Acromegaly may be associated with headaches, visual loss, diabetes and hypertension.
Key Points
General medicine and surgery for dental practitioners:
-
1
Cardiovascular system
-
2
Respiratory system
-
3
Gastrointestinal system
-
4
Neurological disorders
-
5
Liver disease
-
6
The endocrine system
-
7
Renal disorders
-
8
Musculoskeletal system
-
9
Haematology and patients with bleeding problems
-
10
The paediatric patient
Abstract
The endocrine system consists of glands that produce hormones that may exert their effects at distant sites. Widespread problems may result when there is derangement of the system. Disorders may have a bearing on the management of a dental patient either in terms of the treatment itself or the provision of a specific method of anaesthesia.
Similar content being viewed by others
Points in the history
The patient may suffer from diabetes mellitus (DM). This is a persistent state of hyperglycaemia due to either a lack of insulin or a diminished physiological effect of the hormone after production by the pancreas. DM may be diagnosed by two fasting venous blood glucose levels of greater than or equal to 7.8 millimoles per litre. The disease may be Type I (Insulin Dependent Diabetes Mellitus IDDM) or Type II (Non-insulin Dependent Diabetes Mellitus NIDDM). Type I occurs most frequently in young people, whilst Type II is usually a maturity onset diabetes. Type II diabetes is treated by careful diet or oral hypoglycaemics. Factors predisposing to DM include pancreatic disease and drugs eg thiazide diuretics, steroids. Other endocrine disorders such as Cushing's Disease, phaeochromocytoma and acromegaly (all of which are discussed later) may also be relevant as the likelihood of DM is increased in these disorders. The diabetic tendency tends to resolve if the underlying disorder is corrected.
Good control of DM helps to prevent or manage some of the associated complications of the disease which particularly relate to the cardiovascular system and retina. DM may be asymptomatic, but the patient may have noticed drinking excessive fluids, passing lots of urine, lethargy, weight loss and possibly recurrent skin infections.
It is important to ascertain some idea of the degree of diabetic control — patients will often know their typical blood sugar level and have experienced episodes of hypoglycaemia or 'hypo's'. The latter is discussed further later.
Abnormalities of the circulating level of thyroxine are usually due to disorders of the thyroid gland and may be due to over production (hyper-thyroidism) or under production (hypothyroidism). Two main hormones are produced by the thyroid gland — T3 (tri-iodothyronine) and T4 (thyroxine) — the former is five times as active as the latter, and both are bound to protein in the blood. The hypothalamus produces Thyroid Releasing Hormone (TRH) stimulating the release of Thyroid Stimulating Hormone (TSH) from the anterior pituitary, which in turn causes release of T3 and T4 from the thyroid. Details of hyper and hypothyroidism are given in Table 1, and the pathway of T3 and T4 production in Figure 1. Hypothyroidism may decrease the immune response leading to an increased incidence of opportunistic infections such as oral candidosis.
Many patients will be taking the oral contraceptive pill (OCP) which comprises varying proportions of synthetic oestrogens and progestogens. It is the oestrogen component that tends to cause complications. The major risk is the increased chance of thromboembolic disease, especially deep vein thrombosis (DVT). Hypertension and a diabetic tendency are other potential risks. The 'pill' is usually maintained for minor procedures but if a prolonged GA is being given, prophylaxis against DVT eg subcutaneous heparin, should be given due to the increased risk from venous stasis. Some surgeons would recommend discontinuing the OCP for two months prior to a surgical procedure to eliminate the potential for the complications mentioned above.
Many patients are receiving Hormone Replacement Therapy (HRT) which may be given orally or as an implant and aims to replace oestrogen which is deficient due to reduced secretion eg after the menopause or ovary removal. Osteoporosis is inhibited in the patient on HRT and it also appears to reduce the rate of alveolar bone resorption.
A patient may be unaware of pregnancy, especially in the first two months, a time when the foetus is particularly vulnerable. In diabetic patients good control of blood sugar levels may become more difficult during pregnancy. Diabetes may occur for the first time in pregnancy (gestational diabetes) and this usually resolves after birth. In the later stages the patient should not be laid fully supine since the gravid uterus compresses the inferior vena cava and impedes venous return. Likewise, in the unlikely event of having to carry out CPR on a pregnant patient, it is important that the patient is put in a left lateral position otherwise venous return would be similarly impeded.
Cardiac output is increased in pregnancy which leads to a tachycardia. Hypertension in pregnancy will often be asymptomatic but should always be taken seriously. If the hypertension is associated with protein in the urine and oedema the condition is known as pre-eclampsia. This may culminate in eclampsia (hypertension, protein in urine and convulsions) and can have fatal consequences.
Cushing's Disease occurs as a result of excess glucocorticoid production secondary to adrenal hyperplasia. The adrenal hyperplasia, in turn may be secondary to excess adrenocorticotrophic hormone (ACTH) production eg by a pituitary adenoma. Ectopic ACTH may be produced by a small cell lung cancer, producing similar effects. The hypothalamo-pituitary-adrenal axis is shown in Figure 2.
Cushing's Syndrome is similar clinically, but caused by primary adrenal disease eg cancer or adenoma. The terms Cushing's Syndrome and Cushing's Disease are often used synonymously — but incorrectly. The clinical features are discussed later.
Patients with Conn's Syndrome have a tumour or hyperplasia of the adrenal cortex. The resulting high levels of aldosterone secretion lead to potassium loss and sodium retention. The decreased potassium leads to muscle weakness and polyuria, whereas sodium retention leads to hypertension.
Addison's Disease is a disease of the adrenal glands leading to decreased secretion of cortisol and aldosterone. The cause may be tuberculous destruction of the adrenals but is not known in up to 80% of cases. There may be an association with Grave's Disease (see later) or IDDM. If known, the cause is treated but replacement steroids are needed and a steroid boost is therefore required for surgical dental treatment.
Disorders of the parathyroid glands may occur. The function of parathyroid hormone (PTH), secreted by the glands, is to regulate the level of calcium in the plasma by acting on the kidney, gut and bone. Secretion of PTH is stimulated if the plasma calcium level falls. The hormone causes increased reabsorption of calcium by the kidney and gut and induces resorption of bone, to restore a drop in blood calcium level. Hypoparathyroidism occurs most commonly after thyroid surgery since the thyroid and parathyroid glands are anatomically very close (the four parathyroid glands normally lying posterior to the thyroid gland).
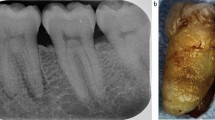
Hyperparathyroidism may be classified as primary, secondary or tertiary. The most common cause of primary hyperparathyroidism is a parathyroid gland adenoma. Secondary hyperparathyroidism occurs when there is a chronically low plasma calcium level eg in chronic renal failure or malabsorption. Tertiary hyperparathyroidism is said to occur when the parathyroid glands have started to produce PTH autonomously, usually after a prolonged period of secondary hyperparathyroidism. Hyperparathyroidism may lead to a loss of lamina dura around the teeth and central giant cell granulomas may occur.1 These are known as brown tumours and are histologically indistinct from other giant cell lesions. If such granulomas are found it therefore prudent to arrange for a test of calcium and PTH levels.
A phaeochromocytoma is a rare cause of hypertension. It is a usually benign tumour of the adrenal medulla (usually unilateral) producing excess catecholamines eg adrenaline. Symptoms are episodic and consist of headaches, palpitations and sweating together with pallor and hypertension. Elective treatment should be delayed until the tumour has been dealt with (local anaesthetic injections with epinephrine [adrenaline] should be avoided). Treatment of phaeochromocytoma is surgical and both alpha and beta blockers are used to prevent hypertensive crises during such surgery.
The patient may report having been diagnosed with Diabetes insipidus — a condition in which impaired water reabsorption occurs in the kidney either as a result of too little anti-diuretic hormone (ADH) being produced by the posterior pituitary or an impaired response to ADH by the kidney. The patient will complain of drinking excessive fluid and passing lots of urine. Causes include head injury, pituitary tumour or sarcoid. Patients may complain of a dry mouth. The Syndrome of Inappropriate ADH secretion (SIADH) may occur secondary to some malignancies and certain benign chest disorders eg pneumonia. It may occur secondary to trauma and is characterised by a low blood sodium level with a high urinary sodium concentration.
Acromegaly (Fig. 3) is caused by increased secretion of growth hormone from a pituitary tumour. It has an insidious onset and the clinical features are discussed in the Examination section. Relevant complications include hypertension, DM and cardiomyopathy (disease of the cardiac muscle).
The main pancreatic problem of relevance in an endocrine context is DM and is discussed above. Hormone secreting pancreatic tumours are rare and include the Zollinger-Ellison Syndrome in which a gastrin secreting tumour leads to duodenal ulceration and diarrhoea. Insulinomas may also occur leading to hypoglycaemia. Glucagonoma leads to hyperglycaemia, oral bullae and erosions.
Nelson's Syndrome affects people who have had bilateral adrenalectomy eg to treat Cushing's Syndrome, which leads to increased pituitary activity and adenoma formation. ACTH is released in great quantities and cutaneous or oral pigmentation may result.
A summary of the main points in the endocrine history is given in Table 2
Examination of patients with endocrine disorders
The diabetic patient may have little or nothing of note to see on clinical examination that gives a clue to their condition. There may be sialosis (swelling of the salivary glands). If diabetic control is poor, oral candidosis may develop. These patients are generally more prone to infections and may have more severe gingivitis than might be expected from the level of oral hygiene. Certainly, diabetic patients are more prone to periodontal breakdown compared with healthy patients.2 The skin is more prone to infections. Peripheral neuropathy may lead to severe foot infections since foreign bodies can be trodden on and not noticed.
A goitre may be noted. This is a lump in the neck comprising an enlarged thyroid gland, usually due to hyperplasia caused by stimulation by TSH, secondary to a decreased level of circulating thyroid hormone. The thyroid gland begins its development at the foramen caecum at the junction of the posterior one third with the anterior two thirds of the tongue and descends to its normal position in the neck during development. On rare occasions remnants of thyroid tissue remain along the developmental path and may be seen as a lump in the midline lying at any point between foramen caecum and epiglottis, the so-called thyroglossal cyst. A goitre may lead to difficulty in swallowing or even compromise the airway. Thyroid tissue may occasionally be present within the tongue – the so-called 'lingual thyroid'. All goitres should be fully investigated, particularly to exclude cancers.
The poorly controlled hyperthyroid patient is tachycardic and may well be in atrial fibrillation with an irregularly irregular pulse. A fine tremor is sometimes noted and the patient may have exophthalmos with resultant diplopia. The thyroid gland itself can be enlarged. The hypothyroid patient will often have a bradycardia, dry skin and hair and a goitre.
A patient with hypoparathyroidism, the commonest cause of which is as a complication of thyroid surgery, may exhibit facial paraesthesia and facial twitching when the preauricular skin over the facial nerve is tapped — known as Chvostek's Sign, due to decreased plasma calcium levels.
In a Cushingoid patient the tissues are wasted, leading to peripheral myopathy and thin skin which bruises easily. Purple striae on the skin (usually abdominal) also occurs. Water retention leads to the characteristic moon face with hypertension and oedema (Fig. 4). There is obesity of the trunk, head and neck (buffalo hump). A summary of the clinical features of Cushing's Syndrome is given in Table 3. In hypofunction (Addison's Disease) hyperpigmentation may be seen eg of palmar creases and buccal mucosa. This pigmentation is related to high circulating levels of Melanocyte Stimulating Hormone (MSH).
Hirsutism is sometimes seen in Cushing's Syndrome and hyperthyroidism as well as acromegaly. It is also seen in ovarian and adrenal tumours.
Facial flushing can be seen in phaeochromocytoma due to the release of sympathomimetic substances or be a sign of the Carcinoid Syndrome due to the over production of 5-hydroxytryptamine. Diarrhoea is associated with the carcinoid syndrome and flushing is precipitated by alcohol or coffee ingestion.
The acromegalic patient (Fig. 3) is easily recognised due to the gigantism, prominent mandible, thickened soft tissues, 'spade-like hands' and prominent supraorbital ridges. There are sometimes visual field defects due to pressure from the pituitary tumour compressing the optic chiasma. A diabetic tendency should be borne in mind.
Factors relating to dental treatment and GA, LA and IV sedation in endocrine disorders
The most common condition to consider is the management of the diabetic patient. When providing treatment under LA alone it is important to check the patient has eaten that day, and taken their usual medication. The signs and symptoms of hypoglycaemia and hyperglycaemia are given in Tables 4 and 5 respectively. When the diabetic regimen needs to be altered eg for GA, this is best done in conjunction with the patient's physician. The management should be matched to the severity of the diabetes, as well as to the planned surgical procedure.
Diabetes When treating a patient with diabetes mellitus as an out-patient a balance must be struck between diet and normal medication. The use of GA necessitates an intravenous infusion in most cases
For diabetes controlled by diet or oral hypoglycaemics undergoing relatively minor oral surgery under LA, the morning dose of oral hypoglycaemic should be omitted with monitoring of blood sugar levels and recommencement of oral hypoglycaemic therapy post operatively. For an IDDM patient undergoing major surgery, an IV infusion of insulin and dextrose and potassium may be used, with the infusion rate titrated against hourly blood sugar measurements. Potassium is required since insulin causes potassium to enter cells and thus the blood level must be replenished.
The use of supplemental steroids prior to dental surgery in patients at risk of an 'adrenal crisis' is a contentious issue3,4 and is discussed in the Respiratory paper in this series. After unilateral adrenalectomy for a Cushing's adenoma, steroid support may be required for a period of weeks or months and the patient's physician should be consulted. After adrenal surgery for phaeochromocytoma, steroid supplementation may rarely be required if the adrenal cortex has been damaged at operation. A GA should not be given to the uncontrolled patient with phaeochromocytoma. Local anaesthetics containing epinephrine should be avoided. Treatment may also be complicated by dysrhythmias and hypertension. Elective treatment should be carried out when the phaeochromocytoma has been treated. If emergency treatment is necessary, the blood pressure should first be controlled by the patient's physician.
A GA may precipitate a thyroid crisis in the untreated patient with hyperthyroidism due to the risk of dysrhythmias. Such a crisis is characterised by dyspnoea, marked anxiety and tremor. Hyperthyroidism must therefore be controlled before GA is contemplated. With appropriate management, this complication should not arise in modern day practice. A treated hypothyroid patient may lapse into hyperthyroidism and this must obviously be considered if a GA is planned. Indeed the use of general anaesthesia and sedation in patients who are hypothyroid must be performed with great care and should only be carried out in specialist units. The use of local anaesthetics containing epinephrine is not contraindicated in patients receiving thyroid replacement therapy. The only time epinephrine should be avoided is during thyroid storm5 ie extreme hyperthyroidism due to thyroid surgery, infection or trauma.
GA or IV sedation should avoided in the first trimester and last month of pregnancy. There is an increased tendency to vomiting, particularly in the last trimester due to the impaired competence of the lower oesophageal sphincter secondary mainly to pressure from the gravid uterus.
The prescription of some drugs by dentists is affected by concurrent endocrine therapy. Erythromycin may interact with diabetic medications, for example combined therapy with chlorpropamide may produce liver damage and concurrent use with glibenclamide may precipitate hypoglycaemia. There may be a reduced efficacy of oral contraceptives during therapy with antibiotics. Although the evidence for this is scarce it is wise to recommend other methods of contraception during antibiotic therapy.6 Similarly, carbamazepine, which may be prescribed for the treatment of trigeminal neuralgia, may decrease the efficacy of the OCP and patients must be warned of this hazard.
Effects of drugs used in endocrine disorders on oro-dental structures
Diabetes When treating a patient with diabetes mellitus as an out-patient a balance must be struck between diet and normal medication. The use of GA necessitates an intravenous infusion in most cases
The impact of corticosteroids on dental treatment was mentioned above. Other drugs used in the management of endocrine disorders may affect the mouth and surrounding structures.
Insulin given by injection may cause pain and swelling of the salivary glands. The oral hypoglycaemic metformin may produce a metallic taste.7 Sulphonylurea hypoglycaemics such as gliclazide and glibenclamide have been implicated in causing oral lichenoid eruptions, erythema multiforme and orofacial neuropathy such as burning tongue.
Hormone replacement therapy with oestrogens may increase gingivitis and cause gingival pigmentation. The OCP may increase gingival and periodontal disease. The amount of gingival exudate is increased in women taking the OCP8 and there is a correlation between the level of progesterone in plasma and gingival inflammation.9
Calcitonin may cause taste disturbance.
Summary
A good basic knowledge of endocrine disorders is essential for safe dental practice. The multisystem effects of various endocrine disorders should be remembered.
References
Shafer WG, Hine MK, Levy BW . A Textbook of Oral Pathology. 4th ed. pp 658–661. Philadelphia: Saunders, 1983.
Shlossman M, Knowler WC, Pettit DJ, Genco RJ . Type 2 diabetes mellitus and periodontal disease. J Am Dent Assoc 1990; 121: 532–536.
Luyk NH, Anderson J, Ward-Booth RP . Corticosteroid therapy and the dental patient. Br Dent J 1985; 159: 12–17.
Thomason JM, Girdler NM, Kendall-Taylor P, Wastell H, Weddell A, Seymour RA . An investigation into the need for supplementary steroids in organ transplant patients undergoing gingival surgery. J Clin Periodontol 1999; 26: 577–582.
Meechan JG, Jastak JT, Donaldson D . The use of epinephrine in dentistry. J Can Dent Assoc 1994; 60: 825–834.
Hersh EV . Adverse drug interactions in dental practice: interactions involving antibiotics. J Am Dent Assoc 1999; 130: 236–251.
Seymour RA, Meechan JG, Walton JG . Adverse Drug Reactions in Dentistry. 2nd ed. p 137. Oxford: Oxford University Press, 1996.
Lindhe J, Bjorn AL . Influence of hormonal contraceptives on the gingiva of women. J Periodont Res 1967; 2: 1–6.
Vittek J, Rappaport SC, Gordon GG, Munnangi PR, Southern AL . Concentration of circulating hormones and metabolism of androgens by human gingiva. J Periodont 1979; 50: 254–264.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Greenwood, M., Meechan, J. General medicine and surgery for dental practitioners Part 6: The endocrine system. Br Dent J 195, 129–133 (2003). https://doi.org/10.1038/sj.bdj.4810395
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4810395
This article is cited by
-
General medicine and surgery for dental practitioners. Part 1 – the older patient
British Dental Journal (2010)