Key Points
-
Orthodontic treatment can effect the appearance of the face in all three dimensions of space. The extent of these effects can be accurately assessed using an imaging technique such as three-dimensional optical surface scanning.
-
It is evident from this study that three-dimensional optical surface scanning allows a greater degree of assessment of facial changes occurring with orthodontic treatment than two-dimensional analyses. This non-invasive three-dimensional technique has great potential for further similar studies.
-
It is important (in particular in this aspect of orthodontics) that the profession make use of the best available resources to allow informed decisions on treatment to be reached.
Abstract
Objective To examine the three-dimensional effects of extraction and non-extraction orthodontic treatment on the facial soft tissues.
Setting Department of Orthodontics, Royal London Hospital.
Design Longitudinal study of two prospective cohorts of patients who were attending for orthodontic treatment.
Method 12 patients were included in each group, in accordance with the selection criteria. Three-dimensional optical surface scans of these patients were obtained in the one month prior to having fixed appliances placed and this was repeated at the end of treatment.
Results The average face of the non-extraction patients was of greater general dimensions than the extraction average, both at the start and the end of treatment. During the fixed appliance treatment, the vermilion of the upper lip became more protrusive to a similar extent in both groups in relation to the reference plane. The lower lip vermilion and the philtrum showed no change for either group over the treatment time. The labiomental fold area showed a slightly greater forward movement in the extraction group with treatment.
Conclusion Three-dimensional optical surface scanning allows data from the whole of the face to be assessed, as opposed to the lateral profile view used in the majority of the studies to date. The effects of the two types of treatment on the facial soft tissues were very similar, indicating that orthodontic treatment involving the extraction of teeth does not have a detrimental effect on the face.
Similar content being viewed by others
Main
The controversy as to whether teeth should be extracted or not as part of orthodontic treatment has been debated since the turn of the last century. Angle1 argued that the 'best balance and proportions of the mouth and its relation to other features require that there shall be a full complement of teeth in all cases'. This non-extraction philosophy as taught by Angle had a significant following with the North American orthodontic profession in the early twentieth century. However, in the United Kingdom, the respective roles of genetics and the environment in the aetiology of malocclusion were given greater significance.2 This resulted in a less marked tendency for non-extraction treatment.
Charles Tweed,3 who was trained under the Angle school, found that cases he had treated in accordance with the Angle philosophy showed poor stability after treatment. To overcome this problem, he re-treated certain cases with the extraction of premolar teeth and this resulted in good aesthetics and stability. The publication of his findings led to a sway of opinion away from the non-extraction ethos.
Begg,4 who was also a student of Angle, agreed with the findings of Tweed. He argued that increases in arch length due to dietary and evolutionary changes, resulted in the need to extract teeth as part of orthodontic treatment.
The modern-day scenario of greater patient awareness on the effects of treatment, and the advancements in orthodontic appliances have led to a more critical approach to the outcome of treatment. For example, we have progressed from merely examining the occlusion after treatment on models, to appreciating the changes that orthodontic treatment may have produced in the facial profile. Investigations into the frequency of extractions as part of orthodontic treatment have shown a surprising variation of between 15% and 95% in orthodontists questioned. This figure reported by Peck and Peck,5 has been confirmed by more recent work6 which showed good intra-operator correlation in the frequency of orthodontic extractions, but poor inter-operator agreement.
Changes in profile with extraction and non-extraction treatment.
The majority of work investigating the effects of orthodontic treatment on the face has been based on lateral cephalometric assessments or two dimensional profile photographs.
The prospective studies of Bishara et al.7,8 comparing extraction and non-extraction treatments, have shown that after treatment, the extraction group had straighter faces and slightly more upright incisors in both arches. The authors concluded that if the decision to extract was based on sound diagnostic criteria, it seemed to have no deleterious effects on the facial profile. Other studies have indicated that at the end of both types of treatment, the mean values for facial contours fell within normal ranges.9
Paquette et al10 looked at 'borderline' extraction/non-extraction cases 14.5 years out of retention and found that in the long term, the non-extraction patients had profiles that were 2 mm fuller. A similar study11 looked at carefully selected and defined first premolar-extraction cases and non-extraction cases over the same post-retention time frame. The results indicated that the extraction of first premolars tended to flatten the profile by 2–3 mm when compared with non-extraction treatment. Interestingly, the non-extraction patients had the more concave faces post-treatment and this challenges the concept of extractions as part of orthodontic treatment 'dishing the face'.
The ability to predict from post-treatment lateral photographs, whether individuals had been treated with or without extractions has been investigated.12 The findings indicated a correct response in only 54% of cases – just greater than pure chance.
Profile changes with growth.
The soft tissues of the face will change with growth and it is important to be aware of the likely growth changes when assessing the effects of orthodontic treatment.
Studies investigating the facial changes that occur with growth have used indirect measurements from lateral cephalograms.13,14,15 Bhatia and Leighton16 have produced the most comprehensive longitudinal cephalometric data from British patients. Following patients from 4 to 20 years old, they found that on average, the upper lip retracted by 3 mm and the lower by 1.5 mm to the Rickett's 'E' plane. The upper lip lengthened by 2 mm in both sexes and the lower increased by 4 mm in females but by 8 mm in males.
Patients usually tend to look at themselves from a 'front-on' or three-quarter profile perspective and infrequently from the side-on view as depicted in lateral cephalograms.
To ascertain changes over the soft tissues of the face, an accurate, reproducible, non-invasive and straight forward technique is ideally required.
Optical surface scanning17,18,19 allows a three-dimensional image of the whole of the face to be recorded with no hazard to the patient and enables the face to be viewed from any direction. The accuracy of this system has been investigated20 and has been shown to vary between 0.5 mm and 2 mm from the direct measurement.
The aims of this study were to obtain three-dimensional optical surface scans of patients at the start of fixed appliance treatment and compare these with scans taken at the end of treatment. Using these it was possible to assess the changes that occurred during treatment.
Materials and method
A prospective study was undertaken using consecutive patients attending for treatment in the orthodontic department of a single institution, fulfilling the following criteria for selection
-
Caucasian race.
-
Aged between 10 and 18 years and requiring fixed appliance treatment.
-
No previous orthodontic treatment.
-
No history of congenital abnormalities or associated syndromes.
-
Cephalometrically skeletal I patterns with a mean ANB value of 3.5 degrees (range 0.74 to 5.31).
-
Maxillary – mandibular planes angle with a mean value of 30 degrees (range 19.88 to 38.31).
Twelve extraction cases (7 females and 5 males) and twelve non-extraction cases (6 females and 6 males) were included in the study. The sexes were pooled in both groups due to the small sample sizes.
All patients were treated with the pre-adjusted edgewise appliance in order to establish a class I occlusion.
Data acquisition
Those patients included in the study underwent an optical surface scan at the start of fixed appliance treatment which was recorded using the three-dimensional optical scanning apparatus previously described.16,17 Each optical surface scan consisted of sixty thousand three-dimensional data points recorded from the surface of the face. This process of scanning was repeated at the end of treatment. The two scans allowed an assessment to be made of the changes that occurred in the facial soft tissues during the course of treatment.
Clarity of the image depended on correct calibration of the apparatus and the co-operation of the patient in not moving while the scan was being produced. Poor quality scans were discarded and the process was repeated as necessary until an acceptable image resulted.
Averaging
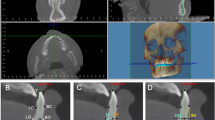
This allowed one representative image of the collection of scans in each subset to be created. The software package enabled the user to automatically configure an average scan based on 5 references points over the forehead region. These were calculated using the computer software programme and were located in a horizontal plane 30 mm superior to soft tissue nasion using the landmark points. A total of 4 average scans were produced, one pre-treatment and one at the end of treatment for each group.
Registration and superimposition
The superimposition of the scans allowed detection of any differences between the pre-treatment and end of treatment images. These differences were displayed in colour, using a registration programme that incorporates the 'least squares patch technique' that has been previously described.16,17
Warm colours (yellow, orange and red) indicate positive changes and the colder colours negative ones, (green, blue and purple). Each colour change represented a 2 mm difference in the respective direction, with brown indicating no change.
Results
Study of method error
To critically assess the accuracy of the scanning procedure, an error study was undertaken. Ten adult subjects were requested to have two scans taken, seven days apart. The completion of normal growth in these cases should mean that there is no difference between the two average scans, presuming the method was employed correctly (Figure 1).
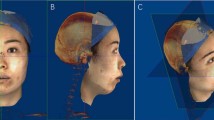
Pre-treatment (Figures 2 and 3)
The non-extraction average face was seen to have slightly larger dimensions, both vertically and laterally, when compared with the extraction face. In the non-extraction face, the soft tissues over the chin region were 7–9 mm in advance of the same area in the extraction group. In the vertical dimension this difference was in excess of 9 mm.
The philtrum This area was similar in both groups at the start of treatment.
The lips The vermilion of the upper lip was 1-3mm further forwards in the non-extraction group. Part of the lower lip vermilion was 1–3 mm further forward in the extraction group.
The labiomental fold This region was in a similar position in the two groups at the start of treatment.
The chin The majority of this area was 1–3 mm further forwards in the non-extraction group at the start of treatment.
Post-treatment (Figures 4 and 5)
Overall, the non-extraction face maintained the greater vertical and lateral dimensions seen before treatment.
The philtrum Part of the philtrum was 1–3 mm further forwards in the non-extraction group, however most of this area showed no difference between the two groups.
The lips The upper lip vermilion was 3–5 mm further forwards in the non-extraction group at the end of treatment. The lower lip vermilion showed no difference between the two groups.
The labiomental fold The non-extraction group was 1–3 mm in advance of the extraction group at the end of treatment.
The chin This area showed no difference between the two groups at the end of the treatment period.
Extraction group (Figure 6)
The time period has resulted in a general increase in the overall dimensions of the face.
The philtrum There was no change in this area over time.
The lips The vermilion of the upper lip was 3–5 mm further forwards at the end of treatment. The majority of the lower lip vermilion showed no difference over the time period.
The labiomental fold At the end of treatment this region was 3–5 mm further forwards when compared with the start of treatment.
The chin There was no change in this area during the course of treatment.
Non-extraction group (Figure 7)
There was an increase in the facial dimensions on the right side with time. There was little change over the left side.
The philtrum – The majority of the philtrum showed no difference over the treatment period, although there were minimal areas showing a 1–3 mm difference.
The lips – The majority of the upper lip vermilion came forwards by 3–5 mm with a small area advancing by 5–7 mm. The majority of the lower lip vermilion showed no difference over the time period.
The labiomental fold – There was a central area that was 3–5 mm further forwards at the end of treatment.
The chin – This area did not exhibit any change over the treatment period.
Discussion
The studies undertaken investigating the effects of extraction and non-extraction orthodontic treatment using lateral cephalograms, indicate that there is great variability in the effects on the facial soft tissues.11,21 However, the indication is that the face flattens slightly7 with extraction treatment.
Long term cephalometric studies of class II division 1 malocclusions have indicated that on average, in borderline extraction cases, the facial profiles of the non-extraction patients were on average 2 mm more protrusive when compared with the extraction patients after treatment.10,11 This study indicates that over the course of treatment, the upper lip has become 3–5 mm more protrusive in both groups, and the lower lip in both cases has shown no change. If these lip changes are related to the reference points of the Rickett's 'E'-plane22 (a tangential plane to the tip of the nose and the tip of the chin), which has been used in the majority of the lateral cephalometric studies on this topic, it appears that during treatment, the lips in the non-extraction group have advanced 1–3 mm further than the lips in the extraction group.
One of the drawbacks with many of the studies undertaken to date is that the reference points used in the methods of analysis, are known to be undergoing growth changes during the period of assessment, for example the Rickett's aesthetic plane21 and Merrifield's 'Z' angle.23
This study included two fairly small sample groups of growing patients. This entails a potential source of inaccuracy in the study as individual growth rates may affect the results. Due to the difficulty with establishing numbers of patients, the groups were not matched for age or sex.
Pre-treatment
The non-extraction average face appears to be larger and therefore the majority of features appear further forward than those same areas in the extraction group. This may have been due to the non-extraction patients being on average, almost 1 year older than the extraction patients.
Post-treatment
The average non-extraction scan still appeared to be further forwards when compared with the average extraction scan. The slightly greater area of 1–3 mm difference between the two groups over the central regions of the face implies a wider 'fullness' of the facial tissues around the lips and labiomental fold in the non-extraction group. However, more peripherally (over the cheeks), the difference between the two groups became less evident over the treatment period. This indicates that somewhat surprisingly, in the peripheral regions, the extraction group appears to show relatively more advancement of the facial structures than the non-extraction group over the treatment period. However, it must be remembered that the effects of growth on each group have not been accounted for in these scans.
Extraction group changes
The upper lip is 3–5 mm further forwards as a result of both growth and treatment changes, and the labiomental fold region advances by 3–5 mm over this time period. The lower lip vermilion and the philtrum area show little change.
Non-extraction group changes
The majority of the changes were very similar to those in the extraction group over the treatment period.
The evidence from this study indicates that when considering the effects of extraction and non-extraction orthodontic treatment on the facial soft tissues, there is very little difference between the two treatment modalities. At most, the lips and the labiomental fold advanced 1–3 mm more in the non-extraction group, with the chin showing negligible change during the treatment period.
This study has illustrated the merits of being able to assess facial changes three-dimensionally when comparing extraction and non-extraction treatment. As the technique is non-invasive; it is possible to record scans at the start of space closure, and repeat these when space closure is complete. This will allow the effects of space closure on the soft tissues of the face to be analysed.
The ability to record data from the whole of the face with this degree of detail, and to observe the face from any desired perspective, allows the profession a more in-depth analysis on the effects of orthodontic treatment on the face.
Conclusions
Firstly, optical surface scanning allows three-dimensional data to be recorded from the whole of the face. Secondly, there is no evidence that in these groups of patients, the extraction of teeth as part of orthodontic treatment, results in a flattening of the facial soft tissues when assessed three-dimensionally. However these findings should be looked upon as a preliminary study and not be extrapolated to the population as a whole. A more in depth study with larger sample sizes and better matched groups needs to be undertaken to verify these findings.
References
Angle EH Treatment of malocclusion of the teeth and fractures of the maxillae. 6th Ed. pp15–23 Philadelphia: SS White Dental manufacturing 1900.
Townend BR The philosophy of orthodontics. Trans Br Orthod Soc 1947; 66–80.
Tweed CH Indications for the extraction of teeth in orthodontic procedures. Am J Orthod 1944; 30: 405–427.
Begg PR Stone Age Man's dentition. Am J Orthod 1954; 40: 298–312.
Peck S, Peck H Frequency of tooth extraction in orthodontic treatment. Am J Orthod 1979; 76: 491–496.
Ribarevski R, Vig P, Dryland Vig K et al. Consistency of orthodontic extraction decisions. Eur J Orthod 1996; 18: 77–80.
Bishara SE, Cummins DM, Jakobsen JR et al. Dentofacial and soft tissue changes in Class II Division I cases treated with and without extractions. Am J Orthod Dentofac Orthop 1995; 107: 28–37.
Bishara SE, Cummins DM, Zaher AR Treatment and post-treatment changes in patients with class II division I malocclusion after extraction and non-extraction treatment. Am J Orthod Dentofac Orthop 1997; 111: 18–27.
James RD A comparative study of facial profiles in extraction and non-extraction treatment. Am J Orthod Dentofac Orthop 1998; 114: 265–276.
Paquette DE, Beattie JR, Johnston LE A long term comparison of non - extraction and premolar extraction edgewise therapy in 'borderline' in Class II patients. Am J Orthod Dentofac Orthop 1992; 102: 1–14.
Luppanapornlarp S, Johnston LE The effects of premolar extraction : A long term comparison of outcomes in 'clear-cut' extraction and non-extraction class II patients. Angle Orthod 1993; 63: 257–272.
Boley JC, Pontier JP, Smith S et al. Facial changes in extraction and non-extraction patients. Angle Orthod 1998; 68: 539–546.
Nanda RS, Meng H, Kapila S et al. Growth changes in the soft tissue facial profile. Angle Orthod 1990; 60: 177–190.
Subtelny JD A longitudinal study of soft tissue facial structures and their implications in oral surgical practice. Am J Orthod 1959; 45: 481–507.
Vig PS, Cohen AM Vertical growth of the lips: A serial cephalometric study. Am J Orthod 1979; 75: 405–415.
Bhatia SN, Leighton BC A manual of facial growth. A computer analysis of longitudinal cephalometric growth data Oxford: Oxford University Press 1993.
Arridge S, Moss JP, Linney AD et al. Three dimensional digitization of the face and skull. J Maxillofac Surg 1985; 13: 136–143.
Moss JP, Linney AD, Grindrod SR et al. 3-dimensional visualization of the face and skull using computerized tomography and laser scanning techniques. Eur J Orthod 1987; 9: 247–253.
Coombes AM, Moss JP, Linney AD et al. A mathematical method for the comparison of three dimensional changes in the facial surface. Eur J Orthod 1991; 13: 95–110.
Aung SC, Ngim RC K, Lee ST Evaluation of the laser scanner as a surface measuring tool and its accuracy compared with direct facial anthropometric measurements. Br J Plastic Surg 1995; 48: 551–558.
Young TM, Smith RJ Effects of orthodontics on the facial profile : A comparison of changes during non-extraction and four premolar extraction treatment. Am J Orthod Dentofac Orthop 1993; 103: 452–458.
Ricketts RM Cephalometric synthesis. Am J Orthod 1960; 46: 647–673.
Merrifield LL The profile line in critically evaluating facial esthetics. Am J Orthod 1966; 52: 804–822.
Author information
Authors and Affiliations
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Ismail, S., Moss, J. The three-dimensional effects of orthodontic treatment on the facial soft tissues – a preliminary study.. Br Dent J 192, 104–108 (2002). https://doi.org/10.1038/sj.bdj.4801305
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4801305
This article is cited by
-
3D Soft Tissue Changes in Facial Morphology in Patients with Cleft Lip and Palate and Class III Mal occlusion under Therapy with Rapid Maxillary Expansion and Delaire Facemask
Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie (2010)
-
Implementing a Superimposition and Measurement Model for 3D Sagittal Analysis of Therapy-induced Changes in Facial Soft Tissue: a Pilot Study
Journal of Orofacial Orthopedics / Fortschritte der Kieferorthopädie (2010)