Abstract
This report is concerned with the manifestations associated with focal dermal hypoplasia (Goltz syndrome) in two patients. Goltz syndrome is a rare polydysplastic syndrome. Systemic findings were similar to those previously reported in the literature and are illustrated. More detailed descriptions of the dental abnormalities are presented. The possibility of root resorption being a previously unreported part of the syndrome is hypothesised.
Similar content being viewed by others
Main
Goltz syndrome is a rare syndrome described by Goltz and co-authors in 1962.1 The accepted term for the syndrome is focal dermal hypoplasia (DHOF) MIM305600, as listed on the Online Mendelian Inheritance in Man website at www.ncbi.nlm.gov/omim/.
This syndrome is seen mainly in females and appears to be sporadic with no relevant family history. It is suggested that the disorder is X-linked dominant or autosomal dominant with sex-limited inheritance caused by a single mutant gene, with a variable expression.2 The syndrome, in its full expression, usually proves fatal to the hemizygous male foetus.3 Goltz et al. (1970) also suggested that the onset of the syndrome is around the eighth week of gestation but the presence of uveal colobomata suggests an earlier onset of 4 or 5 weeks.4
This proposed earlier onset would account for the dental anomalies seen in the dentition. Dental development begins around 6–7 weeks in utero.5
This syndrome affects both mesodermal and ectodermal structures and may result in multiple congenital defects affecting the main body systems (Table 1).6
Abnormalities are also seen in the oral and dental systems. Bucci et al. reviewed the oral and dental anomalies.7 These are listed in Table 2.
This paper reports on two cases of focal dermal hypoplasia and their subsequent management.
Both cases also presented with external root resorption, which may be related to defects in the formation of cementum, previously unreported as part of this syndrome.
Case reports
Case 1
Miss C., a 16-year-old patient was referred to the Department of Restorative Dentistry by her general dental practitioner who was concerned about the appearance of her dentition. At the initial consultation the patient was also aware of pain from the UR1(11) tooth.
She presented with several of the classic systemic signs of the syndrome including disorder of skin pigmentation (Fig. 1) and hand and finger defects (Fig. 2). The syndrome had been diagnosed at birth and there was no family history of the disorder. The dentition was also affected showing enamel hypoplasia resulting in unaesthetic peg-shaped teeth (Fig. 3). The previously reported arborescent hyperplastic lesions affected several areas of the gingiva but were most severe on the labial gingiva related to the upper right central incisor tooth (Fig. 4). Radiographic examination revealed a generalised short root formation and all four second premolar teeth were absent (Fig. 5). The UR1(11) tooth had an area of external root resorption (Fig. 6).
Initial management was aimed at improving the oral hygiene, reducing the cariogenic potential of the diet and improving the dental appearance.
The maxillary central incisor tooth exhibited grade II mobility and required extraction. The tooth was carefully extracted and sent for a pathology report. This revealed external root resorption. The dentine was essentially normal and only acellular cementum was present. This would be expected in a patient of this age.
Replacement of this tooth was initially with an immediate removable acrylic prosthesis. The remaining upper anterior teeth were modified with light cured composite resin to improve their appearance to the patient's satisfaction (Fig. 7).
The provision of an osseointegrated dental implant is being planned as the definitive restoration to replace the UR1(11) tooth.
Case 2
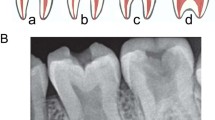
Miss L. was referred to the Department of Restorative Dentistry by a local Oral and Maxillo-facial Unit. She was 19-years-old and presented with hypodontia. She was seeking an opinion concerning the feasibility of dental implants. Miss L. was of short stature and had required surgery to correct skeletal abnormalities of the spine and right leg. She exhibited micropthalmia, the right eye was a prosthetic replacement. The teeth exhibited microdontia and the UR8, UR2, UR1, UL1, UL5, UL8, LL8, LL5, LL1, LR1, LR7, LR8 (18, 12, 11, 21, 25, 28, 38, 35, 31, 41, 47 and 48) were congenitally absent. The enamel hypoplasia, characteristic of the syndrome, was evident. The UR6 (16) tooth was partly submerged but firm to probing. Radiographic examination revealed short root formation (Fig. 8) and a large area of external resorption affecting the crown and cervical one third of the root of the UR6 (16) tooth (Fig. 9).
Unfortunately, before further treatment could be undertaken the patient left the area and was lost to follow-up.
Discussion
Goltz et al. in 1962, first used the phrase 'focal dermal hypoplasia' to amalgamate the features of this disease. Focal dermal hypoplasia is also referred to as Goltz syndrome but should not be confused with Gorlin-Goltz syndrome, an entirely different entity.
The characteristics of Goltz syndrome include disturbance of skin and skin appendages, ocular lesions, musculo-skeletal abnormalities and dental anomalies. The main features of Gorlin-Goltz syndrome8 are naevoid basal cell carcinomas, odontogenic keratocysts, skeletal anomalies and intracranial calcifications. Focal dermal hypoplasia is a rare syndrome. Gorlin et al. in 1990 stated that 'only two hundred cases of Goltz syndrome have been described in the literature'. Cases are mainly sporadic in occurrence with only 10% of reported cases occurring in males.6 Rare male cases have been reported and this is thought to be caused by half-chromatid mutations.9
Each of the cases described here presented with typical systemic oral and dental defects; in addition each case had a tooth affected by an area of external root resorption. This may have been an incidental finding or part of the dysplasia seen in this syndrome. Similarly, McNamara et al.10 reported a case of focal dermal hypoplasia in which a range of the usual dental abnormalities were present and additionally both permanent first mandibular molars exhibited taurodontism.
External root resorption has not previously been described as part of the syndrome. In one case the resorption was a presenting symptom and in the other an incidental finding. In each instance as the result of the extent or the site of the resorption tooth extraction was the outcome.
It is possible that either the cementoblasts, which are ectomesenchymal in origin, or the cementum these cells produce are defective as part of the syndrome. This could result in exposure of dentine with the sequel of root resorption.11
Tronstad11 divided external root resorption into three categories:
-
Progressive inflammatory resorption.
-
Cervical resorption.
-
Replacement resorption.
In this case report the clinical and radiographic appearance of the teeth involved is consistent with the cervical type of resorption. The exact pathogenesis of cervical root resorption is not yet fully understood and requires further study but affected teeth have often been the subjects of previous trauma or orthodontic therapy. Neither of the cases presented here had a history of trauma or previous orthodontic treatment. It is thought that the cervical type of resorption is related to defects in the precementum layer below the epithelial attachment and the resorption is often self-limiting.11 Resorbing activity may be perpetuated when bacteria or their products invading from the gingival sulcus affect the area of destruction. The absence of this continuing stimulus may be the reason why more teeth with cemental defects are not affected by cervical root resorption. The pulp tissue is initially unaffected but as the lesion extends, pulp involvement occurs and pain of pulpal origin supervenes.12
Thus, pain often presents as a late symptom when the extent of tooth destruction may render the affected tooth unrestorable. Case 1 is an example of this sequence of events.
Conclusions
Focal dermal hypoplasia is a rare syndrome affecting ectodermal and mesodermal tissues. It is a multi-system disorder with debilitating oral and dental defects. The cases presented here also demonstrated external root resorption. This has not previously been described as part of the syndrome, and may be a result of cementum disturbance associated with the dental dysplasia.
References
Goltz R W, Peterson N C, Gorlin, R J, Ravit, H G . Focal dermal hypoplasia. Arch Derm 1962; 86: 708–717.
Goltz R W, Henderson R R, Hitch J M, Ott J E . Focal hypoplasia syndrome: A review of the literature and report of two cases. Arch Derm 1970; 101: 1–11.
Wettke-Shäfer R, Kantner G . X-linked dominant diseases with lethality in hemizygous males. Human Genet 1983; 64: 1–23.
Willetts G S . Focal dermal hypoplasia. Br J Opthal 1974; 58: 620–624.
Ten Cate A R . Oral Histology. Development, Structure and Function. 5th ed.: pp 78–103. St. Louis: Mosby, 1998.
Gorlin R J, Cohen M M, Levin S . Syndromes of the Head and Neck. 3rd ed.: pp472–475. New York: Oxford University Press, 1990.
Bucci E, Muzio L L, Mignogna M D . Oral and dental anomalies in Goltz syndrome. J Pedod 1989; 13: 161–168.
Gorlin R J . Nevoid basal cell carcinoma syndrome. Med 1987; 66: 96–113.
Temple I K, MacDowell P, Baraitser M, Atherton D J . Focal Dermal Hypoplasia (Goltz syndrome). J Med Genet 1990; 27: 180–187.
McNamara T, Trotman C A, Hahessy A M & Kavanagh P . Focal dermal hypoplasia (Goltz-Gorlin) syndrome with taurodontism. Special Care Dent 1996; 16: 26–28.
Tronstad L . Root resorption-aetiology, terminology and clinical manifestation. Endodont Dent Traumatol 1988; 4: 241–252.
Cohen S, Burns R C . Pathways of the Pulp. 7th ed.: pp576–579. St. Louis: Mosby, 1998.
Acknowledgements
The authors would like to thank Dr J Rippon for the histopathology report and also the Department of Clinical Illustration, Birmingham Dental Hospital for their help in the preparation of the illustrations in this article.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Baxter, A., Shaw, M. & Warren, K. Dental and oral lesions in two patients with focal dermal hypoplasia (Goltz syndrome). Br Dent J 189, 550–553 (2000). https://doi.org/10.1038/sj.bdj.4800826
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800826
This article is cited by
-
Dental anomalies in 14 patients with IP: clinical and radiological analysis and review
Clinical Oral Investigations (2017)