Key Points
In this part, we will discuss:
-
Overcoming alveolar deficiencies
-
Management of localised deficiencies
-
Soft tissue deficiencies
Abstract
Autogenous grafts are considered to be the most predictable for replacement of deficient bones to facilitate implant treatment. Augmentation of soft tissue may also be required to improve aesthetics and function.
Similar content being viewed by others
Main
The indications for employing corrective or reconstructive surgical techniques may be functional and/or aesthetic and may involve both hard and soft tissues. Sufficient bone must be present to allow placement of an implant of appropriate dimensions in a stable and correct orientation to allow construction of a successful prosthesis. Subsequently the soft tissues surrounding the implant should be able to maintain normal functional integrity and withstand oral hygiene procedures. Aesthetic considerations may be relatively small involving subtle loss of alveolar ridge form or interdental papillae, but at the other extreme may involve significant skeletal jaw base discrepancies which need correction before implant treatment can commence. However, before any corrective surgical procedure is attempted it is important to consider any alternative solutions. For example, potential aesthetic problems may also be overcome by using prosthetic solutions (see Part 9). It is important to discuss the problems and various solutions with the patient, and to explain the relative advantages and disadvantages of these approaches.
Overcoming alveolar bone deficiencies
Overcoming alveolar bone deficiencies
-
Implant solutions
-
Bone augmentation:
Autogenous bone grafts
Guided bone
regeneration
Alloplastic graft materials
Allografts
Xenografts
Bone promoting
molecules
Implant solutions
As described in Parts 4 and 5, a full assessment of bone height and width (and quality) as well as its relationship to the proposed prosthesis is necessary to allow proper planning for implant surgery. Conventionally the aim is to have a border of 1 mm of bone surrounding the implant at the time of placement. This dictates a minimum bone dimension of 6 mm in both the mesial-distal and bucco-palatal direction to allow an implant of 4 mm diameter to be placed. With narrower ridges the obvious alternative is to use a narrower diameter implant. While there may be merit in considering this option it is important to remember that a reduction in implant size, particularly to a diameter less than 3.5 mm, can greatly reduce implant strength as well as surface area for integration/load distribution. Use of small diameter implants should therefore be restricted to low load situations such as replacement of missing lower incisors or upper lateral incisors. In situations where the ridge is broad but has limited height (less than 10 mm), wider diameter implants up to 6 mm can be used. These have a greater surface area for integration and load distribution as well as having an increased resistance to fracture. There are now a great many implant configurations to enable placement in regions with little bone volume but long-term data on their success are lacking. Implant placement at an alternative site to facilitate treatment may also be considered, for example using the pterygoid plates or zygomatic buttresses for implant fixation. However, implants placed in these regions may present both surgical and prosthetic difficulties and their use should be limited to experienced clinicians.
Bone augmentation
Deficiencies in bone may be restricted to small, well defined defects involving one or more sites or may be much more generalised in their presentation affecting the entire jaw. Different techniques and materials are therefore employed to augment bone into these areas although a combination may be used to achieve the desired result.
Autogenous bone grafts
Autogenous bone remains the gold standard by which all other materials are judged. It has many advantages over the alternatives in that it is:
-
Readily available from adjacent or remote sites
-
Sterile
-
Biocompatible/non-immunogenic
-
Osseoinductive/conductive
-
Easy to manipulate.
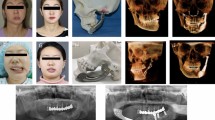
It may be harvested from intra- and extra-oral sites using trephines or by taking bone blocks or chips. Favoured intra-oral sites include the chin (fig. 1), retromolar areas (fig. 2), and other edentulous areas local or remote to the surgical site. Further bone collection is possible by using surgical bone traps attached to the suction apparatus when taking grafts or preparing implant osteotomy sites. This yields a highly osteoconductive osseous coagulum which is also easy to manipulate. Intra-oral harvesting has many merits in that the surgeon is working in an environment which is familiar, and the graft is of the same developmental origin. However, if there is a requirement for large blocks of bone an alternative site needs to be considered. Larger defects therefore require bone from extra-oral sites, the most common of which is iliac crest. While this donor site can provide large blocks of bone, the morbidity associated with this procedure must be considered. Optimisation of grafting is achieved by ensuring that the graft is stable at the time of placement and that there is close adaptation between graft and host bed. This may be achieved by compacting the bone into the available space and by direct fixation using screws or mini-plates (fig. 3). Graft stability may also be improved by using GBR membranes (see below).
In an effort to overcome the morbidity of taking autogenous grafts other techniques and materials have been developed, and these are considered in the following sections.
Guided bone regeneration
One of the most popular techniques used for the treatment of localised ridge deficiencies is guided bone regeneration (GBR). This technique employs barrier membranes which allow creation of a confined defect into which bone progenitor cells may migrate in preference to soft tissue cells, allowing bone to form within the void (fig. 4). Of the many configurations of membranes available one of the most widely used is Gore-Tex™, an expanded polytetrafluoroethylene (PTFE) which was first used in periodontal regeneration. PTFE is non-resorbable and requires removal, therefore involving a second surgical procedure. Other types of membrane are now available which are resorbable and do not require removal.
The ideal properties of GBR membranes are:
-
Biocompatible to minimise any inflammatory response. Membranes which incorporate biochemical factors to enhance bone healing are under development
-
Occlusive to prevent passage of cells during the healing period. Some membranes are semi permeable and allow passage of fluid whereas others have been tried which are totally impermeable. Totally occlusive materials such as titanium sheets formed into the required shape have also been used
-
Physical properties which allow the space under the membrane to be maintained. This may be improved by using: titanium reinforced membranes; 'tent' screws to support the membrane (fig. 5); and fillers such as bone or substitutes to fill the void.
-
Enhance wound stability and protection of the initial clot and delicate granulation tissue. Stabilisation of the membrane may be improved by securing it with small screws/pins or the implant cover screw.
In its simplest form GBR can be used to promote bone fill of a defect before implant treatment. It can also be used to regenerate bone in dehiscences and fenestrations around implants at the time of placement (fig. 4), but it must be remembered that any bone thus created does not contribute to initial implant stability and its long-term significance is currently not known.
Wound closure and stability are very important when using GBR and great efforts to maintain the vitality of the overlying soft tissues need to be made. Flaps with wound edges remote from the surgical site are recommended and wound closure without producing any tension in the soft tissues is required. Soft tissue breakdown over sites where membranes are involved can allow bacterial infection, compromised healing and possibly failure of osseointegration.
Alloplastic graft materials
These include materials such as hydroxyapatite, tricalcium phosphate and bioactive glasses. These materials are easy to use and are commonly used as fillers on their own or in combination with autogenous bone. They provide an osteoconductive framework for bone but are not osteoinductive and are unable to contribute to osseointegration. Their use has been widely documented but their efficacy when used alone as grafting materials in implant surgery requires more evaluation with carefully controlled clinical trials, as is the case for many of the bone substitutes.
Hydroxyapatite is available in a variety of forms, from porous resorbable particles to dense non-resorbable and block forms. The commonly used non-resorbable HA becomes embedded in newly formed fibrous tissue and bone, and the resulting tissue combination is a less than ideal implant bed.
The new generation of bioactive glasses are an effective synthetic bone grafting material. They are silicate glasses whose main components are sodium, calcium and phosphate in varying combinations in particulate form. They are osteoconductive as well as having bone bonding properties through corrosion of the glass when exposed to bodily fluids to produce a silica gel and a calcium phosphate surface layer. The calcium phosphate layer then recrystallises into hydroxycarbonate apatite which is able to bond to bone. This surface layer bears more similarity to the mineral component of bone than hydroxyapatite.
Allografts
Human bone material in the form of freeze dried bone or demineralised freeze dried bone (DFDB) has been used widely both in periodontology and implant dentistry. The donor bone is harvested from cadavers, processed and sterilised. A wide range of grafts are available, which may be particulate, thin sheets of cortical plate, or much larger bone blocks. They are predominantly used as a scaffold for bone repair and are resorbable but often remain as inert fragments long after placement. Despite the measures taken to ensure sterility and non-infectivity of these grafts some doubt must remain as to their absolute safety.
Xenografts
These are graft materials derived from other animal species. Some have received wide acclaim and are used to provide an inert framework for bone regeneration either alone or in combination with autogenous bone graft. Bio-Oss™ is bovine bone in which the organic component is completely removed to leave the mineralised bone architecture. This renders it non-immunogenic and presumably safe from the possibility of trans-species infection.
Other naturally occurring mineralised substances such as Coral have been advocated as it has a pore size which allows bone ingrowth. Recent research has produced some promising results describing the induction of osteoblasts and mineralised bone following implantation of Nacra (the calcium carbonate shell of molluscs).
Bone promoting molecules
The identification and production of bone morphogenetic proteins are a recent advance in regenerative therapies both in periodontology and implant surgery and hold a lot of promise for the future. They have been used with some success in bone regeneration in the maxillary antrum when delivered in a collagen based sponge. They are also present in their natural form in demineralised freeze dried bone, which may account for the reported efficacy of this material, although the processing may inactivate the bone morphogenetic proteins.
Management of localised deficiencies
Small deficiencies in the alveolar ridge may be treated using simple techniques. It is important to consider whether grafting is necessary to achieve a stable implant at the time of placement or whether it is being used to promote bone repair over exposed areas of the implant. Therefore augmentation of small defects may be considered as preparatory or perioperative procedures.
Before implant placement
Bone augmentation before implant placement is generally the preferred option. This is particularly the case for non-submerged or single stage implants. Alveolar defects should be augmented at least 3 months before implant placement but delays greater than 6 months may result in resorption of the graft.
At implant placement
Implant placement in thin ridges may result in incomplete bone coverage of the implant surface. The resulting defects can be described as either dehiscences involving the marginal bone or more apically located fenestrations (fig. 6). The clinician has to decide whether or not these require bone augmentation using grafts or GBR. This will mainly depend upon the size, location and morphology of the defect. Fenestrations are probably of little clinical significance and usually require no treatment. However, attempts should be made to repair large dehiscences or the implant placement abandoned and the site grafted to produce a more favourable situation.
Extraction sockets
Most extraction sockets heal perfectly well without interference by the clinician. However, a large defect may be produced if the buccal plate is lost or in cases of long-standing apical or periodontal infection. These defects can be repaired using a variety of techniques including small bone grafts, GBR, or a combination of the two. It is important that any residual infection is eradicated before the implant is placed. Fortunately the removal of the offending tooth and curettage of the socket usually allows this to occur readily.
While it may be possible to improve socket infill at the time of extraction by placing graft material, an alternative is to place an implant immediately into the socket (fig. 7). In this situation the amount of grafting material is significantly reduced by the implant taking up most of the space (fig. 7b). A prerequisite for this technique is that sufficient bone is present to produce initial stability of the implant ie the graft plays no stabilising role at implant placement (fig. 7c). Stability is normally achieved in these situations by engaging sound bone apical to the socket. With the immediate placement technique soft tissue coverage at implant placement can be difficult or impossible to achieve. While this may not be so important for non-submerged implants, it is desirable for submerged systems and cases where grafts, particularly in combination with membranes, are employed. Where soft tissue coverage is considered important the technique of 'delayed immediate placement' may be employed. In such situations the extraction site is left for about 4 to 6 weeks to allow soft tissue healing before an implant is placed. This period can also be useful to allow infections to completely resolve.
The patient's left incisor was lost many years ago and a standard technique is being employed with placement of a Branemark implant. On the patient's right side the incisor has just been extracted and an implant (Astra) has been placed in the socket. This occupies some of the space within the socket which has good repair potential. Subsequently the labial wall of the socket was collapsed in towards the implant surface thus reducing the bone fill requirement
Management of larger deficiencies
Management of larger deficiencies
-
General techniques
-
Onlay grafts
-
Ridge expansion
-
Sinus lifts (sub-antral grafting)
-
Inlay grafts combined with maxillary osteotomies
-
Bone deficiencies in the posterior mandible
General techniques
Larger bone deficiencies arise because of long-standing progressive resorption following tooth loss and trauma, developmental anomalies, and pathological conditions (tumour resection, cysts, etc). Techniques to overcome these problems, which may involve the entire edentulous jaw, aim to improve the height and or width of the bone available as well as providing bone of sufficient quality to provide implant anchorage. Ridge resorption in the vertical plane may require grafting to allow placement of adequate length implants and to reduce the crown to implant ratio of the prosthesis. Longer implants supporting a lower profile prosthesis will reduce the mechanical demands on the prosthetic components. One of the most difficult problems is the development of a pseudo Class III jaw relation with severe resorption of the edentulous maxilla compared with the mandible. Grafting may therefore be required to provide adequate bone for implant installation and correction of the jaw relationship.
Most of the procedures described in this section are advanced surgical procedures requiring specialist training.
Onlay grafts
Onlay grafts are versatile in that they are able to augment the bone in either the vertical or lateral dimension or a combination of the two (fig. 8). Smaller grafts may be harvested from the chin or retromolar area, although large cortico-cancellous grafts are usually taken from the iliac crest. Grafts should be secured to the recipient bed using miniscrews and plates or wires. The host bed is perforated with a small bur to allow blood clot to form between the two bone surfaces and to allow communication with the cancellous bone which contains osteoprogenitor cells. Any remaining voids may be packed with cancellous bone chips to maximise the healing potential.
A modification of this technique has been described where implants are used to stabilise large onlay grafts. In these cases an iliac graft is taken in one piece which is the same dimension as the proposed dental arch by using a surgical template. The graft is secured to the residual ridge using six or more implants. This is a useful technique to alter jaw relations and simultaneously place implants but requires that the residual alveolus is capable of stabilising the implants and graft.
Ridge expansion
Lack of bone in the bucco-lingual direction may also be dealt with by mid-crestal expansion in which a central cleft is created with standard osteotomes and the ridge split longitudinally. It is important to limit the spread of the longitudinal split by using transverse cuts through the alveolus at both ends of the ridge. Once expanded to the desired width the void can be grafted or a combination of implants and graft material may be placed. As a one stage technique problems may arise because of poor initial stability of the implant. Case selection using this technique is critical as brittle bone may fracture in an unpredictable fashion causing further bone loss. Further accurate positioning and orientation of the implants may be difficult to achieve.
Sinus lifts (sub-antral grafting)
The sinus lift or sinus floor elevation is similar to a Caldwell-Luc procedure combined with grafting of the floor of the maxillary sinus (fig. 9). It is a procedure that can be performed under local anaesthesia and involves carefully cutting a window in the lateral antral wall using surgical burs but retaining the integrity of the sinus membrane (fig. 9b). The window may then be in-fractured to create a discrete cavity on the superior aspect of the residual alveolus. Graft material may then be inserted which serves to keep the bone 'trap-door' in its elevated position (fig. 9c). If the sinus membrane is torn it is not advisable to graft particulate material although blocks of corticocancellous bone can be secured in position. The technique is commonly used as a pre-implant procedure when the residual alveolar ridge has resorbed to a point where initial implant stability is compromised. Thus maxillary ridges with less than 5 mm of available bone height should be augmented at least 3 months before implant placement. This protocol increases the likelihood of achieving stable implants at placement and improves the overall success rates. Alternatively sinus lifts may be employed to allow installation of a longer implant without it entering the sinus proper. If performed as a one stage procedure the implant serves as a support for the bone 'trap door' and may also be used to fix the graft in place, particularly if a block of cortico-cancellous bone is used.
Inlay grafts combined with maxillary osteotomies
Gross resorption of the maxilla leading to a Class III skeletal relationship can be treated using an inlay graft combined with a Le Fort I type osteotomy. This will improve the skeletal jaw relationship and available bone height while leaving the alveolar crest form unchanged. This is therefore particularly useful in the pseudo Class III edentulous maxilla or in partially dentate individuals requiring orthognathic surgery. Once the Le Fort I down fracture is complete a bone inlay of predetermined thickness is placed in the void and sandwiched between the two sections and secured using mini-plates. The size of the inlay required necessitates the use of cortico-cancellous bone from the iliac crest for this procedure.
Bone deficiencies in the posterior mandible
Alveolar resorption in the posterior part of the mandible eventually reduces the available bone height above the inferior dental canal to a point where implants cannot be placed without risk of injury to the inferior dental bundle. It is important to emphasise that due consideration has to be given when planning not only for the implant length but for the fact that the drills used usually prepare the osteotomy site 1–2 mm deeper than the actual implant. It is therefore imperative that the surgeon is familiar with the system and drills being used when planning surgery close to important anatomical structures.
Lack of height above the ID canal can be overcome by onlay grafts or alternatively the nerve bundle itself may be surgically transposed. This is a difficult technique involving deroofing the nerve and dissecting the neurovascular bundle from the body of the mandible as far distally as is required. Implants may then be placed spanning the entire height of the mandible while avoiding the nerve. Once the implants are in place, the boney window which was removed from over the nerve may be replaced in a more mesial position with the nerve emerging from the more distal aspect. This technique carries a potentially high morbidity and should be used rarely and by experienced surgeons. In the edentulous mandible it may be preferable to place multiple fixtures anterior to the mental foramen and construct a prosthesis with a distal cantilever.
Soft tissue deficiencies
Soft tissue deficiencies can give rise to both functional and aesthetic problems.
Functional problems
The soft tissue cuff around the implant abutment has to withstand oral hygiene practices and shearing forces during mastication. It is therefore desirable (but not essential) to have the implant emerging through keratinised attached mucosa. Proposed implant sites that are deficient in this tissue may be augmented by using free gingival grafts either before implant placement, at the time of implant placement, or at abutment connection. Free gingival grafts can be taken from the palate and placed on a prepared donor site which has a good vascular supply (fig. 10). As an alternative interpositional connective tissue grafts may be placed to augment the soft tissue.
The patient had experienced considerable discomfort and a free gingival graft was advised. b) A graft bed is prepared by making a split thickness dissection. c) A graft taken from the palate is transferred and sutured in position. This free graft initially receives nutrients from plasma exuding from the graft bed. Rapid vascularisation then occurs. d) The healed graft after 10 days. This will provide a zone of tissue which will be easier for the patient to maintain in health
Aesthetic problems
Small defects in gingival contour may improve once the restoration emerges through the gingiva. The contours of the restorative components may provide enough support to the soft tissue to give them a perfectly satisfactory appearance without the need for grafting (figs 11 and 12). In addition remodelling of the soft tissues can continue for some time after the prosthesis has been placed.
An implant was placed 6 months previously and abutment connection surgery is to be carried out. The profile of the ridge is very flat. b) The implant was exposed, an abutment connected, and a provisional crown (with a good emergence profile) constructed and fitted. The profile of the soft tissue has been considerably enhanced
However, larger more obvious soft tissue defects will require grafting and this is best performed as a preparatory procedure before implant placement. It can also be performed at the time of implant placement but it may be extremely difficult (or impossible) after the prosthesis has been fitted.
The ideal augmentation material is the patient's own tissue and both free gingival and connective tissue grafts can usually be used to deal with all but the most severe soft tissue deficiencies. Larger deficiencies will also require augmentation of the hard tissues.
Interdental papillary regeneration has been the cause of much surgical enterprise during the past few years and is desirable particularly in the partially dentate patient and around single tooth implants. The papillary regeneration technique basically involves preservation and rotation of attached gingiva at the time of abutment connection surgery. While this is undoubtedly a valid technique, natural papillary remodelling occurs around single teeth and limited span bridges once the prosthesis has been in place for some time. This stands as testimony to the ultimate biocompatability of the well made implant reconstruction and the soft tissue moulding effect of a prosthesis with anatomical emergence profiles.
Conclusion
It can be seen therefore that a myriad of solutions exist to overcome anatomical problems. It is important however to remember the desired treatment outcome and to explore all the possible solutions. By keeping the techniques as simple and predictable as possible and using the patients own tissue the likelihood of success increases greatly.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Palmer, P., Palmer, R. Implant surgery to overcome anatomical difficulties. Br Dent J 187, 532–540 (1999). https://doi.org/10.1038/sj.bdj.4800325
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800325
This article is cited by
-
Recent advances in dental implants
Maxillofacial Plastic and Reconstructive Surgery (2017)
-
An investigation of post-operative morbidity following chin graft surgery
British Dental Journal (2004)
-
Ridge augmentation using mandibular tori
British Dental Journal (2001)