Abstract
Aim At two contrasting centres, to describe the provision of dental general anaesthesia (DGA) for simple non-surgical extractions in terms of the type of treatment provided, including the number of primary and permanent teeth extracted, and the characteristics of child patients attending in terms of their age group and gender.
Design Retrospective analysis of hospital records.
Method Data were drawn from records of services over a 12-month period in 1996/97 at: a) a London dental hospital (Centre 1), and b) in the community dental services in Rochdale, Lancashire (Centre 2). Information was collated and analysed using the SPSS statistical software package.
Results The majority of patients at both centres were aged less than 9 years. Almost one third (31%) of those seen at Centre 1 were below 5 years of age, but fewer of this age group were treated at Centre 2. Children aged 9 years or less had an average of 5.4 (SD = 3.0) primary teeth extracted at Centre 1 and 3.0 (SD = 2.0) at Centre 2. For permanent teeth, an average of 3.2 (SD = 1.2) and 2.7 (SD= 1.4) were extracted at Centres 1 and 2 respectively.
Conclusions Both services were used primarily for the extraction of primary teeth although the services differed in the ages of patients who used them and in the numbers of teeth extracted. Numbers of patients attending the service at Centre 1 had declined over time but numbers of teeth extracted per child had increased.
Similar content being viewed by others
Main
Dental General Anaesthesia (DGA) is used primarily for the extraction of teeth for child patients. It has traditionally been available through primary care and through hospital based services. There has been a marked reduction in the use of general anaesthesia for dental extraction in dental practice.1 Caries is the most common indication for extractions and this reduction may in part be a result of the decrease in prevalence of dental caries seen in children. While this may be inferred on a national level a study in the north of England found only weak correlations between DGA rates in primary care and the level of dental caries.2 Improvement in the level of dental caries among children in the United Kingdom has also been greater in permanent than in primary teeth, and it is for extractions of primary teeth that DGA is more often used. More stringent requirements for services introduced in the early 1990s in response to the Poswillo report may also have contributed to the reductions in DGA services provided through General Dental Services.3 However, the reduction may have been partly offset by an increase in referrals to hospitals and the Community Dental Services,4,5since, despite the changes, a large review in the UK found few problems in access to DGA in primary dental care.5
Socio-demographic variables such as geography, social background and culture are known to affect caries experience and dental care.6,7,8,9 In the north of England, although disease levels were not obviously associated with experience of DGA, socio-demographic factors may have influenced access to and demand for services.2 Not only may provision and use of services vary, but treatment provided using DGA also differs. This may relate to differing need and also be a result of differences in treatment planning among dentists working in the service.4
New guidance was issued in respect of general anaesthesia and resuscitation by the General Dental Council in November 1998. This includes standards for those administering the anaesthetic and a requirement for written protocols to include appropriate arrangements to ensure the immediate transfer of a patient to a critical care facility when needed.10 These recommendations are likely to reduce further the services provided through the General Dental Services and increase the burden on secondary and tertiary referral centres, at least in the short term. Greater use of alternatives may also serve to change patterns of treatment through DGA with time. Information about current use of DGA in differing centres is necessary if changes are to be effectively monitored.
The aims of this paper were to describe (at two contrasting centres) the provision of DGA for simple non-surgical extractions in terms of the type of treatment provided, including the number of primary and permanent teeth extracted, and the characteristics of child patients attending, in terms of their age group and gender. Further, to determine whether there were differences between patients attending the two centres in their characteristics and the treatment they received.
Information and method
Data used for this study related to the provision of dental general anaesthesia (DGA) for child outpatients for purposes of simple (non surgical) extraction of teeth at two centres: Eastman Dental Hospital, London (Centre 1) and Rochdale, Lancashire (Centre 2). The two centres provided available data but had not been selected in any systematic way. The study represented an audit from records at each centre.
Referrals to Centre 1 are primarily from general dental practitioners and the community dental service. On referral, a paediatric dentist first evaluates each child and treatment plans are formulated and agreed with parents, who sign a formal consent. Children are then assessed for fitness by an anaesthetist and, if appropriate, an appointment is given for an outpatient dental general anaesthesia. Only in cases of particular emergency do child patients have an anaesthetic administration on their first visit to the centre.
As at Centre 1 referrals to Centre 2 come primarily from general dental practitioners and from dentists working in the Community Dental Services. At the time of the study, practice was that the parent signed a formal consent, the referring practitioner completed and signed a standard form and provided the patient with instructions. The appointment for dental general anaesthesia was given by telephone and the general health of patients was discussed at this time. At Centre 2, on the appointed day, the anaesthetist undertook to recheck the medical history and ensure that pre-operative instructions had been followed. The operating dentist carried out a dental examination and checked the treatment plan made by the referring dentist. If any change to the plan was proposed this was first discussed and agreed with the parents. If the dentist or anaesthetist considered the child to be unfit for outpatient general anaesthesia at the centre the visit was either deferred or the child re-appointed to an in-patient dental list.
Information for patients at Centre 1 was drawn from the anaesthetic register and collected by one individual (RDH). Data collected were for children who received an out-patient general anaesthetic during the 12-month period between 1.4.1996 and 26.3.1997. The information obtained included age, gender, number of teeth extracted (primary and permanent), and date of extraction. Information for Centre 2 had been collected from patient records of those children who received an outpatient DGA during the period 1-4-1996 to 26-3-1997. The same information was collected as for Centre 1.
A total of 952 and 1,151 child patients had received treatment under out patient general anaesthesia at Centres 1 and 2 respectively. Information on age and/or teeth extracted was missing for 21 patients from Centre 1 and one from Centre 2. These patients were excluded from the study; the final analysis included 931 patients from Centre 1 and 1,150 from Centre 2. All analyses were undertaken using SPSS (SPSS 7.5.1, 1997) and graphical output generated by Microsoft Excel (Windows 1995) software.
Results
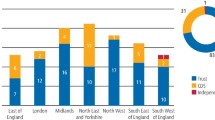
Of the 931 child patients receiving an anaesthetic at Centre 1, 488 were boys (52.4%) and 443 (47.6%) were girls. Of those receiving treatment at Centre 2, 592 (51.4%) were boys and 558 (48.549%) were girls. Age groups are listed in Table 1 and shown in fig. 1. At both centres, children aged 5 to 9 years made up more than half of the total (58% at Centre 1 and 59% at Centre 2.). Children aged 4 or less made up almost a third (31%) of those at Centre 1 but there were greater numbers of children aged 10 years or over among those receiving DGA at Centre 2 (Fig 1). Differences in these age groups were reflected in differences in mean age 6.2 (SD = 2.7) years at Centre 1 and 8.2 (SD = 3.0) years at Centre 2, (t-test: P < 0.001).
Type of treatment
The numbers of patients having primary and permanent teeth extracted at the two centres are shown in Table 2. At both centres, more than three-quarters of patients having DGA during the study period had only primary teeth removed. Very few had only permanent teeth extracted. Fewer patients at Centre 1, 56 (6%) compared with 187 at Centre 2 (16%) had permanent teeth extracted and few at either centre had both primary and permanent teeth removed. (χ2-test: P < 0.001). At both centres, the majority of children aged 9 years or less had primary teeth only extracted. The mean, median and range in numbers of primary and permanent teeth removed, for those having that type of extraction, are shown in relation to age and Centre in Table 3.
0–4-year-old children On average, 0–4-year-old children attending Centre 1 for DGA had 5.4 (SD = 3.2) primary teeth extracted. Values ranged from 1 to 14 teeth with 38 children (13%) having 10 or more teeth removed. At Centre 2, the range of values was similar, at 1–13 but the mean number of primary teeth extracted per child was 3.3 (SD = 2.2), more than 2 teeth fewer. Furthermore, fewer children (5; 3%) had 10 or more teeth extracted. Numbers of extractions were not normally distributed, and the Mann Whitney U test was used to test for statistical significance (Mann Whitney U test: P < 0.001).
5–9-year-old children At Centre 1, among 5–9-year-old children who had primary teeth extracted, between 1 and 14 teeth per child were removed, with a mean of 5.4 teeth (SD = 2.9). Sixty-one children (11% of those aged 5–9 years) had 10 or more teeth extracted. The range in number of extractions was the same at Centre 2 but the average per child was just over half that at Centre 1 (2.9; SD = 2.0). At Centre 2, 8 patients (1%) had 10 or more teeth removed. Fewer children at Centre 1 had permanent teeth extracted but for those who did, more teeth per child were removed than at Centre 2: 2.7 (SD = 1.3) at Centre 1 and 1.8 (SD = 1.0) at Centre 2 (Mann Whitney U tests: P < 0.001 for primary teeth; P < 0.05 for permanent teeth).
10–14-year-old children The pattern seen in numbers of teeth extracted at the two centres for younger children was also evident in 10-14-year-old children but was less marked. Numbers of primary teeth extracted (for those who had primary teeth removed), was greater among those having DGA at Centre 1 (3.7; SD = 3.1), than at Centre 2 (2.8; SD = 1.9). The median number of permanent teeth removed at each centre was 4, the range was greater at Centre 2, but the mean number of teeth removed was higher at Centre 1. Differences in numbers of teeth extracted were not statistically significant for primary teeth but attained significance for permanent teeth (Mann Whitney U test: P < 0.05).
Discussion
This investigation of dental services was carried out on data from two centres providing DGA, one in the North of England and one in London. As well as being in different regions the centres also differed in their place within service provision, Centre 1 representing a dental teaching hospital centre and Centre 2 a community-based service. Both were similar however in providing a service for patients referred by general dental practitioners and by dentists working in the Community Dental Services. Both were dedicated almost entirely to treatment of child patients and results showed that both centres served a spectrum of patients in terms of age and ethnic background.
As has been evident in previous studies, a high proportion of patients receiving DGA at the two centres was aged 9 years or less.4,11 It was of note that children aged 0–4 years made up a much smaller proportion of those from Centre 2 but children aged 10 years or more made up a higher proportion. The difference in numbers of the older children is likely to relate to orthodontic extractions. Extractions for orthodontic purposes are not always an indication for DGA and policy at Centre 1 is that patients should have these carried out with local anaesthesia, with the addition of inhalational sedation if necessary.
A greater number of primary teeth per child were extracted in Centre 1. As an example, children aged 5-9 years, (the largest group), had an average of more than 5 primary teeth extracted whereas the equivalent value for children attending Centre 2 was less than 3 teeth per child. This difference between Centres in numbers of teeth removed was apparent for all age groups and may reflect variations in referrals and/or in treatment planning. Thus it may be in part a consequence of selective referrals -- children requiring single tooth extractions may, for example, be encouraged to have this carried out using local anaesthesia. Treatment planning may also be more radical at Centre 1. General anaesthesia is not without risk and current thinking would appear to encourage more radical treatment planning to reduce repeat general anaesthetic administrations.12 Incorporation of orthodontic treatment planning, with planned balancing and compensating extractions, may also result in larger numbers of teeth being removed at a single administration.
In contrast to the increase seen at the end of the 1980s,4,11 there had been a decline in numbers treated at Centre 1. DGA had been provided for, on average, 5.7 child patients compared with 9.5 per day in 1990/91. During the 1990s, specialist centres for DGA have been opened in several areas. These have been reported to affect numbers of DGA administrations in some areas and may also have influenced numbers at Centre 1. Changes in health service management with greater restriction on referrals may also have influenced the numbers of patients treated. Greater use of alternatives, such as inhalational sedation, may also have helped to reduce numbers. Alternatives to attendance at Centre 1, either in the form of other DGA services or through alternative forms of treatment may have been made more attractive by having to attend twice for administration of DGA. All patients have an anaesthetic assessment at their first attendance and are offered an appointment for the DGA administration, effectively doubling the cost to families. This may have the advantage of discouraging inappropriate use of DGA 'on request' but have the drawback of reducing accessibility in some cases.
The age profile of those attending Centre 1 was very similar to that seen previously at the same centre, with almost a third of the patients being aged less than 5 years,4,11 but average numbers of teeth removed were higher. Children under 9 years had, on average, more than 5 teeth removed, in comparison to the average of 3.9 recorded in a previous study at the same Centre.4 DGA may continue to be of particular value for children who are too young to tolerate treatment using local anaesthesia, even with the addition of inhalational sedation, and for those with severe and extensive forms of caries, including rampant caries. It has been shown that prevalence of this form of the disease in the area of Centre 1 has changed little since the mid-1980s.13
It may be concluded that there were differences between the centres in the characteristics of patients treated and in the nature of treatment provided. Differences in treatment may have been related to treatment philosophy and policy at the centres at least as much as to differences in the populations served. New recommendations from the General Dental Council are likely to have profound effects on all DGA services; specialist services such as the two included in this study will face increasing demand and the pattern of service they provide is likely to change as a result. Alternatives may become more widely available but it is important that services continue to be available for children who need them. It will be important to monitor the role of these services in response to the new recommendations in order to assess their impact on access and use of DGA for young children.
References
Murray J J . General Anaesthesia and Children's Dental Health: Present Trends and Future Needs. Anesth Pain Control Dent 1993; 2: 209–216.
Whittle J G, Jones C M, Hannon C P . Trend in the provision of primary care dental general anaesthesia in the north of England, 1991/92 to 1994/95. Br Dent J 1998; 184: 230–234.
Poswillo D E. (Chair) Standing Dental Advisory Committee. General anaesthesia, sedation and resuscitation in dentistry, Report of an expert working party. London: HMSO, 1990.
Holt R D, Rule D C, Davenport E S, Fung D E . The use of general anaesthesia for tooth extraction in child in London: a multi-centre study. Br Dent J 1992; 173: 333–339.
Clinical Standards Advisory Group. Dental General Anaesthesia. Report of CSAG Committee on General Anaesthesia for Dentistry. London: HMSO 1995.
Pitts N B, Evans D J . The dental caries experience of 14-year-old children in the United Kingdom. Surveys co-ordinated by British Association for the Study of Community Dentistry in 1994/1995. Community Dent Health 1996; 13: 51–58.
Prendergast M J, Beal J F, Williams A . The relationship between deprivation, ethnicity and dental health in 5-year-old children in Leeds, UK. Community Dent Health 1997; 14: 18–21.
Bradnock G, Marchment M D, Anderson R J . Social Background, Fluoridation and Caries Experience in 5-year-old Population in the West Midlands. Br Dent J 1984; 156: 127–131.
O'Brien M . Children's Dental Health in the United Kingdom 1993. London: HMSO, 1994.
General Dental Council. General Dental Council: Maintaining Standards, Guidance to Dentists on Professional and Personal Conduct. Amendments November, 1998.
Smallridge J S, Al Ghanim N, Holt R D . The use of general anaesthesia for tooth extraction for child out-patients at a London dental hospital. Br Dent J 1990; 168: 438–440.
Landes D P, Bradnock G . Demand for dental extractions performed under general anaesthesia for children by Leicestershire Community Dental Service. Community Dent Health 1996; 13: 105–110.
Holt R D, Winter G B, Downer M C, Hay I, Bellis W . A fourth study of caries in preschool children in Camden. Br Dent J 1996: 181; 405–410.
Acknowledgements
The authors are grateful to A J Doyle, Specialist in Dental Public Health.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Holt, R., Al, S., Bedi, R. et al. Provision of dental general anaesthesia for extractions in child patients at two centres. Br Dent J 187, 498–501 (1999). https://doi.org/10.1038/sj.bdj.4800314
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800314
This article is cited by
-
Characteristics of children undergoing dental extractions under general anaesthesia in Wolverhampton: 2007-2012
British Dental Journal (2016)
-
The effect of premature extraction of primary teeth on the subsequent need for orthodontic treatment
European Archives of Paediatric Dentistry (2014)
-
The behaviour, social status and number of teeth extracted in children under general anaesthesia: A referral centre revisited
British Dental Journal (2006)
-
Tooth extraction: A referral centre revisited
British Dental Journal (2006)
-
The use of general anaesthesia for the extraction of children’s teeth. Results from two UK Dental Hospitals
European Archives of Paediatric Dentistry (2006)