Abstract
Objective To evaluate the clinical effectiveness, common complications and maintenance associated with hydroxylapatite (HA) coated cylindrical implants when used to support single crowns.
Design A prospective medium term clinical study of the Calcitek HA-coated implant.
Setting Implant placement, crown fabrication and follow-up procedures were carried out at the Leeds Dental Institute, between 1990 and 1998.
Subjects and method 26 patients (33 implants) participated in the trial. They were referred from general dental practitioners because of their suitability for single tooth implant placement.
Main outcome measures The implants were assessed using recognised clinical review procedures eg radiographs and soft tissue assessments.
Results At exposure there was 100% implant integration. The cumulative survival rate over 4 years was 100%. In five implants there was cervical bone loss of more than 4 mm and these were classified as failing. This gave an overall cumulative success rate of 58% by year 4.
Conclusion The Calcitek HA-coated single tooth implant shows exceptionally high initial integration however, the longer term results suggest that the cervical bone level adjacent to the implant failed to establish a steady state. Doubts remain regarding the long-term prognosis of these cylindrical HA-coated implants.
Similar content being viewed by others
Main
The use of endosseous dental implants for single tooth restorations offers a number of advantages over conventional treatment. Implants do not involve preparation of the adjacent teeth. They preserve the residual bone, and excellent aesthetics can be achieved. The successful application of implants for rehabilitating edentulous or partially edentulous jaws has been well documented in many multicentre studies.1,2,3 However, the use of implants is expensive, the patient requires surgery, the procedure is time consuming, and technically complex. There is a lack of long-term data on single tooth implants. In addition the long-term success of implants especially when placed in the maxilla is still in question.4
Studies have indicated success rates ranging from 100%5 to 85%6 for single tooth implants. The success of endosseous implants depends on the continued integrity of the interface between implant and bone. Attempts have been made to decrease the incidence of breakdown of this implant/bone interface by modifying the implant surface. One such method has been to coat titanium implants with hydroxylapatite (HA). HA is a bioactive ceramic that has been shown to form a strong ionic bond with bone mineral.7,8 HA-coated implants may integrate more often than non-coated ones in sites with poor quality bone.9,10 Histological investigations have shown an absence of intervening fibrous tissue between implant and bone. HA is thought to accelerate healing as bone is laid down simultaneously on the coating and on the site of the prepared socket.11,12 There are several HA-coated implant systems on the market and they vary widely among manufacturers in their composition, crystallinity, density, purity and structure. Several retrospective 5 to 8 year clinical studies on these implants from centres in the USA13,14,15,16 show overall cumulative survival rates which range from 71% to 97%.
The purpose of this prospective medium term study has been: (1) To evaluate the success of Calcitek Omniloc cylindrical HA-coated implants (Calcitek Inc – A company of Sulzer Medica, Carlsbad, CA, USA) when used to support single tooth restorations, (2) to report on the maintenance requirements and complications following completion of treatment.
Materials and methods
Implants
The Calcitek Integral dental implant system was developed in 1984. In 1990 they introduced the Omniloc implant which specifically dealt with the single tooth situation. The implant consists of a cylindrical titanium alloy core (Ti6Al4V) coated with a 50–70 μm layer of dense highly crystalline HA. The implant is un-collared, and available in 8, 10, 13, 15 and 18 mm lengths and diameters of 3.25 and 4.0 mm. The implant contains an anti-rotational device, a recessed octagon. This is engaged by the corresponding male component at the base of the abutment. The two are secured by means of a floating screw contained in the abutment (fig. 1).
Patient selection
Between 1990 and 1994, 26 patients were selected to take part in this clinical evaluation, for which ethical approval was obtained in 1989. Their ages ranged between 22 and 63 years, 16 were males. Patients were excluded from the study if they were medically compromised, had poor oral hygiene, smoked heavily (20 or more a day), had inadequate bone volume or suffered severe psychiatric disorders. The patients underwent an extensive introduction to implant treatment, designed to inform them of the procedure, the benefit and risks, follow-up and maintenance required. They were then invited to sign a detailed informed consent form.
Clinical procedure
Before placement of implants, a thorough history and examination was completed. Potential implant sites were identified and the quantity and quality of bone assessed both by clinical examination, ridge mapping and radiographic views. The magnification of the radiographs was determined by using either a brass rod or ball bearing of known dimension held in position with wax over the implant site. Surgical stents were constructed for optimum positioning of the implants.
The surgical placement of the implants was undertaken by one of two consultant oral surgeons. Surgery was completed under standard aseptic techniques according to the guidelines set out by the manufacturer, with appropriate antibiotic cover. The size of the implant selected depended on the quantity of bone available, but as a general rule the longest and widest implant possible was selected. The patients were requested not to wear their partial dentures for 2 weeks post surgery after which the dentures were modified with a tissue conditioner over the implant site.
The implants were left buried for 3 months in the mandible and 6 months in the maxilla before exposure and placement of a temporary titanium gingival cuff. Three to four weeks following this, the restorative stage of treatment began and was completed by one of two senior restorative clinicians. Impressions were taken of the implant head by means of an impression post using a putty and light bodied silicone wash. Where implant alignment allowed, the crowns were designed to be screw retained, but if this was not possible they were cemented using zinc oxyphosphate or a temporary luting cement.
Review appointments
The first examination after placement of the prosthesis provided the baseline for follow-up. The patients subsequently underwent bi-annual clinical and annual radiographic examination.
Radiographic evaluation
Baseline radiographs were taken when the implants were exposed. Follow-up radiographs were recorded annually thereafter. The radiograph of first choice was a periapical view standardised using a Rinn film holder (Dentsply, Weybridge, UK).
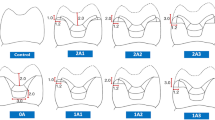
Calculations of marginal bone height were undertaken from a fixed reference point at the junction of the abutment and the implant shoulder. For each implant the distance from the reference point to the first marginal bone contact was measured at the mesial and distal surfaces. The distance was measured with a 2x lens, by two observers to an accuracy of ±0.5 mm and the mean of the two measurements calculated. There was 90% agreement between the observers. A mean and cumulative bone loss was then calculated with a normalisation ratio, which corrected for radiographic magnification.
In this study implant survival was defined as 'a retained non-mobile implant capable of supporting a crown during normal function'. Implant success was defined as 'an implant, which was functional, symptom free, had no obvious clinical pathology or radiographic signs of progressive cervical bone loss, which exceeded 4 mm or over a third of the implant length'. This was first described by Spiekermann et al. as a method of determining failure of cylindrical designed implants.17
Lifetime tables were tabulated using survival/success analysis.18
Results
Twenty-six patients were treated with 33 implants (28 in the maxilla, 5 in the mandible). All the maxillary implants were placed mesial to the second premolar and the mandibular ones distal to the canines in type III or IV bone.19 All 33 implants were found to be integrated when exposed and to date none have exfoliated giving a 100% survival rate. In some patients where the implant appeared clinically to be a success, there were examples of saucerisation and vertical bone loss seen on the radiographs (fig. 2). The mean annual bone loss in year 1 was 1.5 mm with a range from 0–6mm. This reduced by year four to 0.4 mm with a range of 0–2.5 mm. The mean cumulative bone loss after 4 years was 2.8 mm and ranged from 0–9 mm.
The radiograph on the left shows a gutta percha point placed in the sinus seen in figure 5
Table 1 shows the distribution of cervical bone loss in each year of the study. Half the implants showed less than 1 mm bone loss in the first year. By the fourth year all 24 implants available for review showed some bone loss although in five this was less than 2 mm. In a further five implants the loss exceeded 4 mm and clearly these were classified as failing. Eight implants lost significant bone in the first 2 years then stabilised showing no further bone loss. However, 9 implants showed signs of bone loss in excess of 0.2 mm/year for each of the 4 years of the study.
Bone loss can also be expressed as a percentage of the implant length. The mean bone loss after 4 years was 17% and ranged from 0 to 69%. Table 2 shows this bone loss in years 1–4. By the end of year 4, five implants were seen to have bone loss in excess of a third (> 30%) of the implant length.
Table 3 shows the interval (per year) and cumulative success rates. By year 4 of the study the cumulative failure rate had risen to 42 %. Table 4 shows the failure rates related to implant length and diameter.
In this study, seven patients were diagnosed clinically as having chronic periodontitis (patients with periodontal pockets greater than 4 mm and radiographic evidence of cervical bone loss around natural teeth). None of their implants were classified as failing.
Of the 10 implants placed in smokers three were classified as failing. Of the 23 implants placed in non-smokers only two were failing.
It is difficult to determine if occlusal forces influence failure in this study as all the crowns were constructed to have either light, or no occlusal contact in centric jaw relation. Fourteen implants were restored with 15 degree pre-angled abutments and 19 with straight. It is notable that four of the five failing implants were fitted with the angled abutment.
The crowns were retained by a screw in 15 cases and cemented in 18. The majority of crowns were the conventional bullet shape. However, five had to be ridge-lapped to provide acceptable aesthetics from an unfavourable implant position (fig. 3).
Of the restored implants, 24 (73%) encountered some problems. Table 5 details the common restorative complications. Twelve crowns (36%) became loose during function on one occasion. Eight of these were caused by the abutment screw becoming loose. In two patients, the crowns were not retrievable (cemented) and their crowns had to be sectioned to obtain access to the floating screw. These crowns were re-fabricated. Three patients had their crowns remade because of unacceptable aesthetics resulting from an error in the emergence profile or subsequent gingival recession.
Of the 26 patients, 13 required only two visits for construction of the artificial crown. Nine patients required three to four, and four needed more than five visits to complete restorative treatment.
After crown insertion the mean number of visits per annum including 6-monthly reviews was 2.4 in year 1 which reduced to 1.5 by year 3 as some of the patients failed to attend every 6 months. One patient (a dentist) failed to attend any review appointments. Two patients required more than four visits every year.
Discussion
This prospective study of 33 Calcitek HA-coated single tooth implants found no surgical complications during or after implant placement and patients reported minimal post-operative discomfort. The surgical kit is simple to use. The drill set allows internal irrigation while preparing the bone for implant placement. The push fit design of the implant enables simpler surgical placement compared with that needed for threaded implants. The packaging of the implant, with the cover-screw already in position further simplifies the procedure. The 3.25 mm diameter implants were an advantage in cases of limited alveolar bone width.
In an attempt to achieve primary fixation with the non-threaded implant, socket preparation must be undertaken with great care. Over preparation will lead to a lack of primary stability of the implant. When under prepared the implant must be pushed firmly into the socket with a potential risk of displacement into the maxillary antrum, or damage to the fragile HA coating.
At surgical exposure all the implants in our study were found to be integrated, giving a survival rate of 100% which equates favourably with other studies.20,21,22,23
In this study, assessment of soft tissues was completed using various indices: plaque and gingival indices;24,25 pocket depth measurements using a calibrated periodontal probe (Vivacare) at a controlled force of 25 g; peri-implant crevicular fluid volume, measured using a Periotron (Perioflow);26 percussion tests using the Periotest (Siemens AG).27 Base-line radiographs were taken when the implants were exposed. Follow-up radiographs were recorded annually thereafter. Of all the clinical data collected we found that only the radiographic monitoring could reliably predict implant failure.28,29 So details of the other clinical assessments used, are not reported here.
There are a number of criteria used to determine implant failure. Smith and Zarb28 specify that successful implants should show a progressive vertical bone loss of 0.2 mm or less after the first year of service. Using this criterion it was found that 9 of the 24 (38%) implants available to follow-up after 4 years of service were failing. However, the rate of bone loss was very different among these nine patients. In some patients it was less than 0.5 mm per year and in others as high as 1.5 mm. To make it easier to classify a failing implant the authors of this paper elected to use the criteria developed by Spiekermann et al.17 These workers considered a cylindrical implant to be failing if there was cervical bone loss of greater than a third of the implant length or more than 4 mm. Using this criterion five implants (four maxilla, one mandible) were classified as failing.
By classifying these five implants as failing the cumulative success rate, according to our criteria, reduced to 58% by year 4. The progressive bone loss gives cause for concern and is in line with other long-term studies on HA-coated implants which have shown a failure to achieve a stable state with respect to cervical bone levels.30,31,32
The reason for this progressive bone loss is not clear. From other studies factors such as implant size, existing periodontal disease, smoking, bone quality, and occlusal load have all been implicated in implant failure.33,34,35 The small number of smokers in this study meant that meaningful data on failure rates in this group was not available.
It is thought that the length of the implant is related to its survival. Guttenberg in 1993 reported that nearly 80% of implants lost in his review study were either 8 or 10 mm in length.36 Saadoun and LeGall reported significantly higher success rates with implants longer than 14 mm.37 Implants in our study were selected to fully use the available width and height of bone. At the present time our study gives no clear evidence to suggest that the diameter or length of an implant influences bone loss but it would seem logical that longer implants would take longer to fail. Ichikawa et al.38 have reported from their clinical and histological findings that the bone at the neck of HA-coated implants appears over-stressed caused by rigid bio-integration of HA to the thin surrounding bone. They speculate this to be the cause of rapid bone resorption in HA-coated implants. This may also explain why there is no clear correlation between implant diameter and failure in our study, as it may be the residual bone thickness that is the critical factor.
Surprisingly the presence of chronic periodontal disease seemed to have no detrimental influence on implant survival and this agrees with the findings of Mengel.6 Seven implants were placed in patients with radiographic evidence of periodontal disease and none of these implants have as yet been classified as failing.
The availability of angled abutments and various cuff lengths resolved all potential restorative problems. However, four of the five failing implants had crowns constructed on angled abutments. This suggests that non-axial functional forces may be a contributing factor to implant failure in the long term.
A degree of retrievability was possible if implant alignment allowed the retaining screw to emerge from the palatal aspect of the crown. This allowed cementation of the abutment to the crown out of the mouth prior to placement, which prevented extrusion of cement into the gingival crevice. Screw retained crowns were an advantage when completing maintenance of the implants at a later stage. An advantage of the Omniloc system is that the clinician or technician can modify the abutment and prepare the shoulder if required, in order to achieve the optimal aesthetic result for the final crown.
The authors did find some restorative complications with the Calcitek system. Each time the impression post or abutment was attached to the implant it was not self-seating because of the shallow octagon, and required a periapical radiograph to confirm accurate location (fig. 4). The Calcitek impression post had insufficient flat surfaces for confident relocation in the impression. The design was later modified by the manufacturer. A potential hazard existed when preparing the shoulder on the abutment. If this was too deep in the region of the weld joint, the housing became weak and had the potential to fracture. This has occurred in three restorations.
Achieving an aesthetic emergence profile for the final crown was difficult, especially when the narrower 3.25 mm diameter implant was used. This small diameter implant is significantly different to the natural tooth/root it replaces.
After completion of the restorative phase of treatment complications were common. The remake of crowns (15%) was mostly caused by aesthetic problems as a result of gingival recession or porcelain fracture. The soft tissue complications included peri-implantitis, gingival contour problems and sinus formation. Sinus formation only occurred when the transmucosal abutment became loose (fig. 5).
The incidence of abutment loosening caused by the internal screw becoming loose was high with eight implants (24%) being affected. Some studies on the Branemark implant have shown similar problems with a 43–45% incidence of loose abutment screws.39,40 The problem in our study was related to the Omniloc design which clinicians found difficult to locate. It did not appear to give secure anti-rotation under occlusal load. The manufacturers now recognise this problem and have altered the design accordingly, incorporating a splined interface which is a series of interlocking turrets. The authors have no experience of this new interface.
Conclusions
Calcitek hydroxylapatite-coated single tooth implants have a high integration rate. With proper treatment planning and technique, surgical complications are few. The mean bone loss in the first year after implant placement was 1.5 mm. By the fourth year the mean cumulative bone loss was found to be 2.8 mm. Complications with abutment or crown loosening are a common problem with the Calcitek Omniloc system. This is related to the design of the anti-rotational device. Radiographic follow-up has shown that five implants have developed progressive bone loss, which now exceeds more than one third the length of the implant. These implants are now classified as failing although they still support a restoration.
References
Henry P, Tolman D E, Boldender C . The applicability of osseointegrated implants in the treatment of partially edentulous patients. Three-year results of a prospective multicentre study. Quintessence Int 1993; 24: 123–129.
Albrektsson T, Bergman B, Folmer T . A multicentre report of osseointegrated oral implants. J Prosthet Dent 1988; 60: 75–84.
Laney W R, Harris D, Krogh P H J, Zarb G A . Osseointegrated implants for single tooth replacement. Progress report from a multicentre prospective study after 3 years. Int J Oral Maxillofac Implants 1994; 9: 49–54.
Jemt T and Lekholm U . Implant treatment in the edentulous maxillae: A 5-Year follow-up report on patients with different degrees of jaw resorption. Int J Oral Maxillofac Implants 1995; 10: 303–310.
Kemppainen P, Eskola S, Ylipaavalniemi P . A comparative prospective clinical study of two single tooth implants: A preliminary report of 102 implants. J Prosthet Dent 1997; 77: 382–387.
Mengel R, Stelzel M, Hasse C, Flores-de-Jacoby L . Osseointegrated implants in patients treated for generalised severe adult periodontitis. An interim report. J Periodontol 1996; 67: 782–787.
Jarcho M . Calcium phosphate ceramics as hard tissue prosthetics. Clin Orthop 1981; 157: 259–278.
Cook S D, Kay J F, Thomas K A, Jarcho M . Interface mechanics and histology of titanium and hydroxylapatite coated titanium for dental implant application. Int J Oral Maxillofac Implants 1987; 2: 15–22.
Biesbrock A R, Edgerton M . Evaluation of the clinical predictability of hydroxylapatite-coated endosseous dental implants: A review of the literature. Int J Oral Maxillofac Implants 1995; 10: 712–720.
Block M S, Kent J N . Long- term follow up on hydroxylapatite coated cylindrical dental implants: A comparison between developmental and recent periods. Int J Oral Maxillofac Surg 1994; 52: 937–943.
Boyne P J . Hydroxylapatite coatings on dental implants (bone response to Hydroxylapatite). J Oral Implantol 1994; 20: 227–231.
Soballe K . Hydroxylapatite ceramic coating for bone implant fixation. Acta Orthop Scand 1993; 64 (suppl 155): 1–58.
Golec T S, Krauser J T . Long-term retrospective studies on hydroxyapatite-coated endosteal and subperiosteal implants. Dent Clin North Am 1992; 36: 39–65.
Stultz E R, Lofland R, Sendax I V and Hornbuckle C . A multicentre 5-year retrospective survival analysis of 6200 Integral implants. Compend Contin Educ Dent 1993; 14: 478–486.
Wheeler S L . Eight-year clinical retrospective study of titanium plasma-sprayed and hydroxylapatite-coated cylinder implants. Int J Oral Maxillofac Implants 1996; 11: 340–350.
Block M S, Gardiner D, Kent J N, Misiek D J, Finger I M, Guerra L . Hydroxylapatite-coated cylindrical implants in the posterior mandible: 10-year observations. Int J Oral Maxillofac Implants 1996; 11: 626–633.
Spiekermann H, Jansen V K and Richter E J . A ten-year follow-up study of IMZ and TPS implants in the edentulous mandible using bar-retained overdentures. Int J Oral Maxillofac Implants 1995; 10: 231–243.
Babbush C A, Kent J N, Misiek D J . Titanium Plasma-sprayed (TPS) screw implants for the reconstruction of the edentulous mandible. J Oral Maxillofac Surg 1986; 44: 274–282.
Misch C . Density of bone: effect on treatment plans, surgical approach, healing and progressive loading. Int J Oral Implant 1990; 6: 23–31.
Avivi-Arber L, Zarb G A . Clinical effectiveness of implant supported single tooth replacement: The Toronto study. Int J Oral Maxillofac Implants 1996; 11: 311–321.
Andersson B, Odman P, Lindvall A M, Lithner B . Single tooth restorations supported by osseointegrated implants: Results and Experiences from a prospective study after 2 to 3 years. Int J Oral Maxillofac Implants 1995; 10: 702–711.
Gomez-Roman G, Schulte W, d'Hoedt B, Axman-Krcmar D . The Frialit-2 implant system: five year clinical experience in single tooth and immediately post-extraction applications. Int J Oral Maxillofac Implants 1997; 12: 299–309.
Watson R M, Gaukroger M C, Newman P M . Single tooth, implant-stabilised crowns replacing anterior teeth: A clinical comparison of two systems. Dent Update 1995; 22: 412–419.
O, Leary T J, Drake R B, Nailor J E . The plaque control record. J Periodontol 1972; 43: 38.
Loe H, Silness J . Periodontal disease in pregnancy. Prevalence and severity. Acta Odontol Scand 1963; 21: 532–551.
Last K S, Cawood J I, Howell R A, Embrey G . Monitoring of Tubingen endosseous dental implants by glycossaminoglycans analysis of gingival cervicular fluid. Int J Oral Maxillofac Impl 1991; 6: 42–49.
d'Hoedt B, Lukas D, Muhlbradt L, Scholz F, Schulte W, Quante F & Topkaya A . The periotest — research and clinical trials. Dtsch Zahnarztl Z 1985; 40: 113–125.
Smith D E, Zarb G A . Criteria for success of osseointegrated endosseous implants. J Prosthet Dent 1989; 62: 567–572.
Cox J F, Zarb G A . The longitudinal clinical efficacy of osseointegrated implants. A 3-year report. Int J Oral and Maxillofac Implants 1987; 2: 91–100.
Teixeira E R, Sato Y, Akagawa Y and Kimoto T . Correlation between mucosal inflammation and marginal bone loss around hydroxyapatite-coated implants: A 3-year cross sectional study. Int J Oral Maxillofac Implants 1997; 12: 74–81.
Jovanoivic S A, Kenney B, Carranza F A, Donath K . The regenerative potential of plaque induced peri-implant bone defects treated by a submerged membrane technique: An experimental study. Int J Oral Maxillofac Implants 1993; 8: 13–18.
Albrektsson T . On long term maintenance of the osseointegrated response. Aust Prosthodont J 1993; 7(suppl): 15–24.
Watson C J, Ogden A R, Tinsley D, Russell J, Davison E M . A three to six year study of overdentures supported by hydroxylapatite coated endosseous dental implants. Int J Prosthodont 1998; 11: 610–619.
Bain C A . Smoking and implant failure — benefits of smoking cessation protocol. Int J Oral Maxillofac Implants 1996; 11: 756–759.
Bain C A . Influence of smoking on the periodontium and dental implants. Dent Update 1997; 24: 328–330.
Guttenberg S A . Longitudinal report on Hydroxylapatite-coated implants and advanced surgical techniques in a private practice. Compend Contin Educ Dent 1993; suppl 15: 549–553.
Saadoun A P, LeGall M . Clinical results and guidelines on Steri-Oss endosseous implants. Int J Periodontics Restorative Dent 1992; 12: 487–499.
Ichikawa T, Hirota K, Kanitani H . Rapid bone resorption adjacent to hydroxylapatite-coated implants. J Oral Implantol 1996; 22: 232–235.
Jemt T, Pettersson P . A 3-year follow-up study on single implant treatment. J Dent 1993; 2l: 203–208.
Ekfeldt A, Carlsson G E, Borjesson G . Clinical evaluation of single-tooth restorations supported by osseointegrated implants. A retrospective study. Int J Oral Maxillofac Implants 1994; 9: 79–183.
Acknowledgements
The authors are grateful to the Dental Illustrations Unit of the Leeds Dental Institute, for preparing the illustrative material. Funding for this study was provided by the Special Trustees, Leeds General Infirmary and the Calcitek Corporation, Carlsbad, California.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Watson, C., Tinsley, D., Ogden, A. et al. A 3 to 4 year study of single tooth hydroxylapatite coated endosseous dental implants. Br Dent J 187, 90–94 (1999). https://doi.org/10.1038/sj.bdj.4800211
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800211
This article is cited by
-
A systematic review on the long-term success of calcium phosphate plasma-spray-coated dental implants
Odontology (2016)
-
Good occlusal practice in the provision of implant borne prostheses
British Dental Journal (2002)
-
Hydroxylapatite coated dental implants
British Dental Journal (1999)