Abstract
Objective To assess the quality of panoramic radiographs in a sample of general dental practices, to determine the relative frequency of errors and to identify those errors directly responsible for diagnostically inadequate images.
Materials and methods Examination of 1,813 panoramic radiographs obtained from 41 general dental practitioners and recording of faults. The study was carried out in 1998. Radiographs were judged as being 'excellent', 'diagnostically acceptable' or 'unacceptable'.
Results Only 0.8% of films were 'excellent', 66.2% were 'diagnostically acceptable' and 33% were 'unacceptable'. The most common faults which directly contributed to failure of the radiographs were antero-posterior positioning errors, low density and low contrast.
Conclusions The quality of panoramic radiographs was considerably lower than standards recently set for primary dental care. The quality of panoramic radiography could be improved by careful attention to radiographic technique and processing.
Similar content being viewed by others
Main
The use of panoramic radiology in general dental practice has shown a remarkable expansion over the past 20 years. Recently, it was estimated that around 1.7 million panoramic films are exposed annually in NHS practice in England and Wales alone (Dental Practice Board; personal communication, 1997). This figure excludes radiographs produced in the rest of the United Kingdom and those taken in hospitals, community dental services and as part of non-NHS dental practice.
The quality of any radiograph is dependent upon accurate technique and careful processing. Compared with intra-oral radiography, panoramic radiography poses particular challenges in both of these aspects of image production. Accurate positioning and preparation of patients is needed to ensure the image is not distorted or affected by ghost images,1 while quality control is critical when screen film is processed.2
The principal aim of this study was to assess the quality of panoramic radiographs in a sample of general dental practices. The subsidiary aims were to determine the relative frequency of errors and to identify those errors directly responsible for diagnostically inadequate images.
Material and methods
The dentists participating in this study were recruited by direct mailing from a list of responders to a previous questionnaire on aspects of panoramic radiology carried out in 1997. Details of the questionnaire are reported in detail elsewhere3 but, briefly, 819 dentists using panoramic radiography in their practices were identified using lists obtained from 22 randomly selected family health service authorities (FHSAs) in England and Wales and by subsequent telephone enquiry. There were 542 responders to the questionnaire (response rate of 73.3% after excluding 58 dentists who were subsequently found to be unavailable due to retirement, sickness, etc). These dentists were circulated with an invitation to participate in a study on panoramic radiology.
Forty-one dentists agreed to take part in the study (7.6% positive response). The work was carried out during 1998. Each dentist was invited to submit 50 consecutive panoramic radiographs of adult patients (18 years or over) to the investigators. The radiographs were viewed by two observers (VER and KH) simultaneously and a consensus assessment of quality made. All radiographs were viewed under identical conditions using a standard 15 cm by 30 cm light box in a room with subdued lighting. Each radiograph was scored for the absence or presence of a range of technical and processing faults:
Technical faults
Poor film/intensifying screen contact
Image of foreign objects (and/or their ghost shadows) on film
Antero-posterior patient positioning errors
Angulation of occlusal plane errors
Incorrect sagittal plane position
Slumped position with spinal column shadow
Tongue not in contact with palate
Patient movement
Absence of orientation (left/right) markers
Other technical faults
Processing faults
Faults in density
Faults in contrast
Developer/fixer splashes
Localised film fogging artefacts (leak in cassette)
Generalised film fogging
Chemical streaks/contamination
Screen artefacts (screen damage or foreign body in cassette)
Inadequate fixation or washing
Automatic processor roller marks
Pressure artefacts
Other processing faults
Finally, the observers made a consensus judgement upon the diagnostic acceptability of each radiograph as 'excellent', 'diagnostically acceptable' or 'unacceptable' according to previously published guidelines.4 The term 'excellent' is applicable where there are no errors of technique or processing. In any case where the two observers were unable to reach a consensus the radiograph was scored as 'diagnostically acceptable'. Where a radiograph was judged to be unacceptable, the fault or faults which directly contributed to failure were specifically recorded.
The frequencies of individual faults on all radiographs were calculated. The frequencies of faults which directly contributed to failure of radiographs were then calculated for the unacceptable radiographs. A one-way analysis of variance F-ratio test was carried out to test for differences between the mean numbers of technical and processing faults recorded for each dentist. Data tabulation and analysis was performed using the SPSS PC+ statistical package.
Ten per cent of radiographs were re-examined by the observers to determine the repeatability of assessments. Repeatability was calculated both in terms of percentage agreement and by calculation of the kappa (κ) statistic.5
Results
The 41 participating dentists submitted a total of 1,813 panoramic radiographs for the study. Only 28 dentists each returned a complete allocation of 50 radiographs, the remaining dentists having submitted less than 50 before time and financial constraints necessitated the termination of the study.
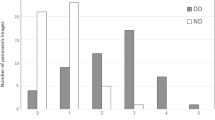
Only 14 (0.8%) of radiographs were free of faults and therefore classifiable as 'excellent' using the recommended criterion.4 Twelve hundred (66.2%) were 'diagnostically acceptable', containing errors which did not detract from the diagnostic utility of the radiograph. The remaining 599 (33.0%) were 'unacceptable'.
When all 1,813 radiographs were considered, the mean number of technical faults per radiograph was 2.75 (SD = 1.48). Table 1 lists these faults and the proportions of radiographs affected by them. The mean number of processing faults per radiograph was 2.96 (SD = 1.55). Table 2 lists the processing faults and the proportions of radiographs exhibiting them.
When the 599 unacceptable radiographs were considered in isolation, the mean number of technical faults per radiograph was 3.54 (SD = 1.47), while the mean number of processing faults was 3.63 (SD = 1.48). The faults which most frequently made a direct contribution to diagnostic inadequacy of films were antero-posterior positioning errors and faults in film density and contrast. Table 3 lists all the faults recorded as contributing to unacceptability and the proportions of the 599 unacceptable radiographs affected.
Analysis of variance identified highly significant differences in the numbers of technical (F = 13.72, two degrees of freedom; P < 0.001;) and processing (F = 12.40, two degrees of freedom; P < 0.001) faults between the dentists. Similarly, the proportion of 'unacceptable' radiographs varied markedly from dentist to dentist, ranging from a lowest figure of 10% to the highest of 72%. The highest proportion of 'excellent' radiographs recorded was 11.1%, with no other dentist achieving a figure exceeding 4%.
Table 4 shows the results of the repeatability of assessments by the observers. According to Landis & Koch,6 values of κ (Greek kappa) exceeding 0.75 indicate excellent agreement beyond chance, values between 0.4 and 0.75 indicate fair to good agreement beyond chance, while values below 0.4 indicate poor agreement. In those cases where faults had frequencies lower than 5% at the first assessment of radiographs, the use of the kappa statistic was not appropriate. However, for all these uncommon faults, not included in Table 4, percentage agreement was in every case higher than 96%.
Discussion
In any study where a sample of dentists is involved it is important to consider whether that sample can be considered as representative of dentists as a whole. This is particularly true where evidence of considerable variation in performance is seen between practitioners, as here. The 41 dentists were recruited after a positive response to a questionnaire and a subsequent invitation to participate in a study. It would seem unlikely that dentists who perceive their own radiographic quality as poor would be eager to expose their deficiencies to others. Thus it is unlikely that the method of recruitment would attract dentists who had poor standards of radiography. Indeed, it could be argued that any bias in the study design would have favoured recruitment of dentists with an interest in research and in radiography, who might be expected to have higher standards. Consequently, some caution should be applied before trying to extrapolate the results of this study to all dentists using panoramic radiography. Clearly, a more representative sample would have been possible only by compulsory involvement of a random sample of dentists using panoramic radiography, an option not available to us.
This study only included radiographs of adult (≥ 18 years) patients. This criterion was dictated by other aspects of the study not reported here. No study appears to have been carried out comparing panoramic film quality for adult and paediatric patients, but a greater incidence of certain technical faults (movement, positioning errors) might be expected with children. It would be interesting to investigate the quality of panoramic radiographs of children, particularly bearing in mind that many panoramic films are taken for orthodontic purposes and that concerns over radiation protection are greater in the young.
Films were assessed by consensus of two observers, both experienced teachers of dental radiology. Consensus viewing has been previously shown to be superior to assessment by an individual in terms of reproducibility.7,8 In this study, agreement between repeated assessments was assessed using the kappa statistic. For the majority of errors there was good or excellent agreement in repeated assessments and there was no error for which the value was lower than 0.40 (Table 4). However, agreement was only fair for five errors. Generally, we noted that agreement was lower where the error lacked a clear threshold separating 'presence' or 'absence'. For example, in some cases we found it difficult to achieve consistency in recognising 'automatic processor roller marks'; a mark might sometimes be scored as a fault while on another occasion it might be judged as being an intrinsic feature of an automatically processed radiograph. Nevertheless, it was reassuring to note that agreement was excellent for the assessment of overall film acceptability.
The high frequency of positioning errors was striking. The limited dimensions of the focal plane (image layer) in panoramic radiography mean that minor errors in positioning manifest as distortions due to unequal vertical and horizontal magnification, overlap of teeth and a loss of image sharpness. We have no information as to the age of the panoramic equipment used by the dentists in the study, but previous work on the large sample from which these practitioners were recruited showed that many dentists use old (>10 years) machines.3 Newer equipment tends to incorporate more sophisticated positioning aids and it is possible that the inevitable replacement of older machines might help reduce error rates.
The commonest technical fault was failure to place the tongue in contact with the palate. The resulting air in the mouth is visible on the radiograph as a band of radiolucency, or 'burn out', over the maxillary teeth. This can markedly reduce diagnostic quality, although in this study it was extremely unusual for it to result in an unacceptable radiograph. Experience suggests that patients may find it difficult, or become a little confused, when asked to place the tongue against the palate. As this fault was rarely significant, its prominent position at the head of Table 1 should not be allowed to overshadow the less frequent, but highly significant, positioning faults.
Low image density and contrast were also common contributing factors to inadequacy of radiographs. While this may have been caused by underexposure, it is probable that it was largely related to under-development. Careful attention to processing quality control, including timely replacement of chemicals, time/temperature control and automatic processor maintenance can do much to avoid density and contrast errors. The use of digital radiography would eliminate this problem, but expense may mean that this solution will not be widely adopted for many years in general dental practice.
The commonest processing fault was the presence of artefacts due to dirty intensifying screens or foreign bodies and scratches on the screen surface. While this did not result in a proportionately high number of non-diagnostic radiographs, the presence of such artefacts is unsatisfactory. Regular cleaning of screens, ensuring cassettes are closed except during loading or unloading film and replacement when screens are significantly damaged can eliminate this as a problem.
The Guidelines on Radiology Standards for Primary Dental Care set quality standards for dental radiography, defining the terms 'excellent', 'diagnostically acceptable' and 'unacceptable'.4 The basic standard was that the rate of 'unacceptable' radiographs should not exceed 10%. If the current sample is a representative one then this standard will be a challenge for the majority of dentists. Good quality radiography aids diagnosis. Furthermore, it maximises the benefits to the patient which must be balanced against the radiation risk and the financial outlay. Some of the radiographs in the study were unequivocally of no diagnostic value, yet involved the payment of a fee. Thus, in addition to being an issue of radiation protection, the production of non-diagnostic radiographs becomes a consumer issue for the patient and/or health service purchaser.
A target of not less than 70% 'excellent' (fault-free) films was also suggested in the guidelines.4 The results of the study, similar to those in a previous study9 suggests that this standard may prove to be a considerable challenge. Almost all radiographs (99.2%) exhibited some fault, usually several. However, many of these faults were essentially unimportant. In view of the results of this study, it might be appropriate to re-think the quality standards set in the guidelines, removing any mention of 'excellent' films and concentrating upon achieving a significant reduction in 'unacceptable' radiographs. It is likely that efforts to improve quality and reduce reject rates would inevitably lead to an increase in 'excellent' films thereafter.
We were assessing the radiographs in a manner divorced from the clinical situation. Thus it is possible that some of the films we judged as 'inadequate' might have had some diagnostic value for the dentists. Nevertheless, all the films in the study were 'routine' screening radiographs, presumably taken with a view to identifying all types of dental pathology. Thus poor film quality would inevitably have reduced the diagnostic yield in some respect.
Comparison of the results of this study with previously published work is difficult when different assessment criteria were used. For example, Akesson determined adequacy of radiographs on the basis of the image quality of the marginal periodontal bone support only.10 Nevertheless, her figure of 31% inadequate radiographs in a small sample from various Swedish primary care clinics is similar to ours. In contrast, Brezden and Brooks recorded that only 18.2% of panoramic radiographs were inadequate.9 The difference may be explained by the fact that the radiographs in the American study9 had been submitted to a third party payment authority for pre-authorisation or claim processing. It is likely that in this situation dentists would repeat poor quality films to avoid the risk of a claim being rejected. In contrast, British dentists are far less likely to have to submit a radiograph to a third party.
Akesson10 found better image quality was obtained in samples of radiographs obtained from a hospital department than from those taken in primary care clinics. This finding echoed the results of Schiff et al.,11 who found that radiographs taken by trained technicians had fewer technical faults. These results indicated, predictably, that highly trained operators are likely to produce better quality radiographs. In this study we did not ask dentists to reveal who in the practice took the radiographs. However, we have previously reported that over one third of dentists in a questionnaire survey used unqualified personnel to take panoramic radiographs.3 The results of this and previous studies are, therefore, an encouragement to better training of dentists and/or ancillary staff in panoramic radiography and quality control.
Conclusion
What else can be done to improve panoramic radiographic quality in general practice? An aggressive stance might be to restrict the technique to hospitals and a few specialised practices with established quality assurance programmes. However, this would probably be unreasonable bearing in mind the large numbers of panoramic x-ray machines in practice and the associated significant investment made by dentists. 'Blanket' recommendations on improving quality may not be effective, bearing in mind that significant variations were seen between dentists in the numbers and types of faults recorded. As with all radiographic quality assurance it is essential to carry out a film reject analysis4,12 as a means of individualising quality control measures. Of course, to do this effectively it is necessary to recognise faults and what causes them. This suggests that education, both undergraduate and postgraduate, should include a prominent component of film fault analysis.
Quality assurance efforts are often more effectively carried out with the aid of individuals who are not part of the immediate dental team. Panoramic radiographic quality might, therefore, be a particularly useful subject for peer review and clinical audit groups. However, only a proportion of dentists take part in such activities. A more effective method of raising quality might be by the direct involvement of third party payment agencies, such as the Dental Practice Board or private medical insurance companies, a suggestion first made by Brezden & Brooks.9 Such agencies could ask for sight of a random sample of panoramic radiographs from dentists and feed back a report on the image quality, along with suggestions about how any errors might be eliminated. This simple procedure, which could be performed by a suitably trained lay person, deserves further investigation to determine its efficacy in raising standards.
This work was supported by a grant from the North West NHS Reactive Funding Scheme.
References
Langland O E, Sippy F H, Morris C R, Langlais R P . Principles and practice of panoramic radiology. 2nd ed. Philadelphia: WB Saunders, 1992.
Thorogood J, Horner K, Smith N J D . Quality control in the processing of dental radiographs. Br Dent J 1988; 164: 282–287.
Rushton V E, Horner K . Aspects of panoramic radiology in general dental practice. Br Dent J 1999; 186: 342–344.
Report by the Royal College of Radiologists and the National Radiological Protection Board. Guidelines on radiology standards for primary dental care. Documents of the NRPB 1994; 5(3): 30.
Cohen J . A coefficient of agreement for nominal scales. Educ Psychol Measur 1960; 20: 37–46.
Landis J R, Koch G G . The measurement of observer agreement for categorical data. Biometrics 1977; 33: 159–174.
Marken K E . Studies of deviations between observers in clinico-odontological recording. Publications of the Umea Research Library Series 1962; 2: 8. Uppsala: Almqvist & Wiksells.
Koran L M . The reliability of clinical methods, data and judgements. N Engl J Med 1975; 293: 642–646 and 695–701.
Brezden N A, Brooks S L . Evaluation of panoramic dental radiographs taken in private practice. Oral Surg Oral Med Oral Pathol 1987; 63: 617–621.
Akesson L . Panoramic radiography for the assessment of marginal bone level. Swed Dent J 1991; Supplement 78: 101–129.
Schiff T, D'Ambrosio J, Glass B J, Langlais R P, McDavid W D . Common positioning and technical errors in panoramic radiography. J Am Dent Assoc 1986; 113: 422–426.
Horner K . Quality assurance I: reject analysis, operator technique and the x-ray set. Dent Update 1992; 19: 75–80.
Author information
Authors and Affiliations
Additional information
Refereed Paper
Rights and permissions
About this article
Cite this article
Rushton, V., Horner, K. & Worthington, H. The quality of panoramic radiographs in a sample of general dental practices. Br Dent J 186, 630–633 (1999). https://doi.org/10.1038/sj.bdj.4800182
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.4800182
This article is cited by
-
Tooth detection for each tooth type by application of faster R-CNNs to divided analysis areas of dental panoramic X-ray images
Radiological Physics and Technology (2022)
-
Panoramic and Personalised Intelligent Healthcare Mode
Journal of Shanghai Jiaotong University (Science) (2022)
-
Challenges in X-ray diagnosis: a review of referrals for specialist opinion
British Dental Journal (2017)
-
Comparison of clinical and dental panoramic findings: a practice-based crossover study
BMC Oral Health (2013)
-
Modern dental imaging: a review of the current technology and clinical applications in dental practice
European Radiology (2010)