Abstract
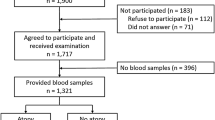
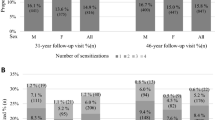
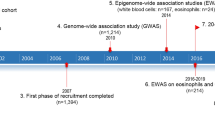
Several studies have suggested an association between IgE-mediated atopic allergies and depression. The present study extends our understanding about putative gender differences of this association and provides further epidemiological evidence for our previous finding that the association between atopy and depression may be characteristic for females only. In order to clearly determine the presence of atopic disorders and depression, we used more valid tools than had been employed earlier and we had access to a database (the Northern Finland 1966 Birth Cohort), in which individuals were followed up prospectively until the age of 31 years. The information on allergic symptoms, verified by skin-prick tests and comprising data of 5518 individuals, was used to ascertain the presence of atopy. Depression was assessed with the help of Hopkins' Symptom Checklist-25 and self-reported doctor-diagnosed depression. After adjusting for a father's social class, mother's parity, and place of residence, logistic regression analyses showed that the risk of developing depression increased in parallel with the increasing severity of depression and, when compared with nonatopic subjects, was 3.0 to 4.7-fold up in atopic females and statistically significant. In atopic males, the association between atopy and depression was statistically significant only in the highest depression scores, the odds ratio being 6.3-fold. The results indicate that females suffering from atopic diseases might possess an elevated risk of developing depression already during early adulthood. In males, the association between these two disorders is evident only among the most severe manifestations of depression. Possible background theories, that is, genetic abnormalities in serotonin metabolism, HPA-axis dysfunction, and histamine theory are discussed.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Bell I, Jasnoski M, Kagan J, King D . Depression and allergies: survey of a nonclinical population. Psychother Psychosom 1991; 55: 24–31.
Centanni S, Di Marco F, Castagna F, Boveri B, Casanova F, Piazzini A . Psychological issues in the treatment of asthmatic patients. Respir Med 2000; 94: 742–749.
Goethe JW, Maljanian R, Wolf S, Hernandez P, Cabrera Y . The impact of depressive symptoms on the functional status of inner-city patients with asthma. Ann Allergy Asthma Immunol 2001; 87: 205–210.
Hashiro M, Okumura M . The relationship between the psychological and immunological state in patients with atopic dermatitis. J Dermatol Sci 1998; 16: 231–235.
Herbert TB, Cohen S . Depression and immunity: a meta-analytic review. Psychol Bull 1993; 113: 472–486.
Irwin M . Immune correlates of depression. Adv Exp Med Biol 1999; 461: 1–24.
Miller GE, Cohen S, Herbert TB . Pathways linking major depression and immunity in ambulatory female patients. Psychosom Med 1999; 61: 850–860.
Olff M . Stress, depression and immunity: the role of defense and coping styles. Psychiatry Res 1999; 85: 7–15.
Schleifer SJ, Keller SE, Barlett JA . Depression and immunity: clinical factors and therapeutic course. Psychiatry Res 1999; 85: 63–69.
Dantzer F, Bluthe RM, Laye S, Bret-Dibat JL, Parnet P, Kelley KW . Cytokines and sickness behavior. Ann NY Acad Sci 1998; 840: 586–590.
Maes M . A review on the acute phase response in major depression. Rev Neurosci 1993; 4: 407–416.
Mössner R, Daniel S, Schmitt A, Albert D, Lesch KP . Modulation of serotonin transporter function by interleukin-4. Life Sci 2001; 68: 873–880.
Wamboldt MZ, Hewitt JK, Schmitz S, Wamboldt FS, Räsänen M, Koskenvuo M et al. Familial association between allergic disorders and depression in adult Finnish twins. Am J Med Genet (Neuropsychiatr Genet) 2000; 96: 146–153.
Wamboldt M, Weintraub P, Krafchick D, Wamboldt F . Psychiatric family history in adolescents with severe asthma. J Am Acad Child Adolesc Psychiatry 1996; 35: 1042–1049.
Bartlett SJ, Kolodner K, Butz AM, Eggleston P, Malveaux FJ, Rand CS . Maternal depressive symptoms and emergency department use among inner-city children with asthma. Arch Pediatr Adolesc Med 2001; 155: 347–353.
Wamboldt M, Schmitz S, Mrazek D . Genetic association between atopy and behavioral symptoms in middle childhood. J Child Psychol Psychiatry 1998; 39: 1007–1016.
Timonen M, Hakko H, Miettunen J, Karvonen JT, Herva A, Räsänen P et al. Association between atopic disorders and depression: findings from the Northern Finland 1966 birth cohort study. Am J Med Genet (Neuropsychiatr Genet) 2001; 105: 216–217.
Timonen M, Jokelainen J, Silvennoinen-Kassinen S, Herva A, Zitting P, Xu P et al. Association between skin-test diagnosed atopy and professionally diagnosed depression: a Northern Finland 1966 birth cohort study. Biol Psychiatry 2002; 52: 349–355.
Rantakallio P . Groups at risk in low birth weight infants and perinatal mortality. Acta Paediatr Scand Suppl 1969; 193: 1–71.
Rantakallio P . The longitudinal study of the Northern Finland birth cohort of 1966. Pediatr Perinatal Epidemiol 1988; 2: 59–88.
Degoratis LR, Lipman RS, Covi L . SCL-90: an outpatients psychiatric rating scale-preliminary report. Psychopharmacol Bull 1973; 9: 13–28.
Nettelbladt P, Hansson L, Stefansson CG, Borgquist L, Nordstrom G . Test characteristics of the Hopkins Symptom Checklist-25 (HSCL-25) in Sweden, using the Present State Examination (PSE-9) as a caseness criterion. Soc Psychiatry Psychiatr Epidemiol 1993; 28: 130–133.
Sandanger I, Moum T, Ingebrigtsen G, Dalgard OS, Sörensen T, Bruusgaard D . Concordance between symptom screening and diagnostic procedure: the Hopkins Symptom Checklist-25 and the composite international diagnostic interview I. Soc Psychiatry Psychiatr Epidemiol 1998; 33: 345–354.
Winokur A, Winokur DF, Rickels K, Cox DS . Symptoms of emotional distress in a family planning service: stability over a four-week period. Br J Psychiatry 1984; 144: 395–399.
Kilpeläinen M, Terho EO, Helenius H, Koskenvuo M . Farm environment in childhood prevents the development of allergies. Clin Exp Allergy 2000; 30: 201–208.
Pekkanen J, Xu B, Järvelin MR . Gestational age and occurence of atopy at age 31—a prospective birth cohort study in Finland. Clin Exp Allergy 2001; 31: 95–102.
Williams HC, Strachan DP, Hay RJ . Childhood eczema: disease of the advantaged? BMJ 1994; 308: 1132–1135.
Kemppainen L, Makikyro T, Jokelainen J, Nieminen P, Jarvelin MR, Isohanni M . Is grand multiparity associated with offsprings' hospital-treated mental disorders? A 28-year follow-up of the North Finland 1966 birth cohort. Soc Psychiatry Psychiatr Epidemiol 2000; 35: 104–108.
Lenzi A, Lazzerini F, Marazziti D, Raffaelli S, Rossi G, Cassano GB . Social class and mood disorders: clinical features. Soc Psychiatry Psychiatr Epidemiol 1993; 28: 56–59.
Väisänen E . Psychiatric disorders in Finland. Acta Psychiat Scand 1975; 65 (Suppl 263): 167–178.
Rantakallio P, Läärä E, Isohanni M, Moilanen I . Maternal smoking during pregnancy and delinquency of the offspring: an association without causation? Int J Epidemiol 1992; 21: 1106–1113.
Agresti A . Categorial Data. John Wiley & Sons: New York, 1990.
Kronfol Z, Remick DG . Cytokines and the brain: implications for clinical psychiatry. Am J Psychiatry 2000; 157: 683–694.
Kelley DS . Modulation of human immune and inflammatory responses by dietary fatty acids. Nutrition 2001; 17: 669–673.
Dantzer R . Cytokine-induced sickness behavior: where do we stand? Brain Behav Immun 2001; 15: 7–24.
Prescott SL, Macaubas C, Smallacombe T, Holt BJ, Sly PD, Holt PG . Development of allergen-specific T-cell memory in atopic and normal children. Lancet 1999; 353: 196–200.
Abbas AK, Lichtman AH, Pober JS . Immediate hypersensitivity. In: Abbas AK, Lichtman AH, Pober JS (eds). Cellular and Molecular Immunology, 4th edn. WB Saunders Company: Philadelphia, PA, 2000, pp 424–445.
Mössner R, Lesch KP . Role of serotonin in the immune system and in neuroimmune interactions. Brain Behav Immun 1998; 12: 249–271.
Lesch KP . Serotonergic gene expression and depression: implications for developing novel antidepressants. J Affect Disord 2001; 62: 57–76.
Elenkov IJ, Wilder RL, Chrousos GP, Vizi ES . The sympathetic nerve—an integrative interface between two supersystems: the brain and the immune system. Pharmacol Rev 2000; 52: q595–638.
Hurwitz EL, Morgenstern H . Immediate and longterm effects of immune stimulation: hypothesis linking the immune response to subsequent physical and psychological wellbeing. Med Hypotheses 2001; 56: 620–624.
Elenkoc IJ, Chrousos GP . Stress hormones, Th1/Th2 patterns, pro/anti-inflammatory cytokines and susceptibility to disease. Trends Endocrinol Metab 1999; 10: 359–368.
Maes M, Smith RS . Fatty acids, cytokines, and major depression. Biol Psychiatry 1998; 43: 313–314.
Musselman DL, Miller AH, Porter MR, Manatunga A, Gao F, Penna S et al. Higher than normal plasma interleukin-6 concentrations in cancer patients with depression: preliminary findings. Am J Psychiatry 2001; 158: 1252–1257.
Pariante CM, Pearce BD, Pisell TL, Sanchez CI, Po C, Su C et al. The proinflammatory cytokine, interleukin-1 alpha, reduces glucocorticoid receptor translocation and function. Endocrinology 1999; 140: 4359–4366.
Holsboer F . Stress, hypercortisolism and corticosteroid receptors in depression: implications for therapy. J Affect Disord 2001; 62: 77–91.
Pariante CM, Miller AH . Glucocorticoid receptors in major depression: revalence to pathophysiology and treatment. Biol Psychiatry 2001; 49: 391–404.
Elenkov IJ, Webster E, Papanicolaou DA, Fleisher TA Chrousos GP, Wilder RL . Histamine potently suppresses human IL-12 and stimulates IL-10 production via H2 receptors. J Immunol 1998; 161: 2586–2593.
Elenkov IJ, Webster EL, Torpy DJ, Chrousos GP . Stress, corticotropin-releasing hormone, glucocorticoids, and the immune/inflammatory response: acute and chronic effects. Ann NY Acad Sci 1999; 876: 1–11.
Ito C . The role of brain histamine in acute and chronic stresses. Biomed Pharmacother 2000; 54: 263–267.
Ito C, Shen H, Toyota H, Kubota Y, Sakurai E, Watanabe T et al. Effects of the acute and chronic restraint stresses on the central histaminergic neuron system of Fischer rat. Neurosci Lett 1999; 262: 143–145.
Hibbeln JR . Fish consumption and major depression (letter). Lancet 1998; 351: 1213.
Peet M, Murphy B, Shay J, Horrobin D . Depletion of omega-3 fatty acid levels in red blood cell membranes of depressive patients. Biol Psychiatry 1998; 43: 315–319.
Tanskanen A, Hibbeln JRH, Hintikka J, Haatainen K, Honkalampi K, Viinamäki H . Fish consumption, depression, and suicidality in a general populaiton. Arch Gen Psychiatry 2001; 58: 512–513.
Duchen K . Are human milk polyunsaturated fatty acids (PUFA) related to atopy in the mother and her child? Allergy 2001; 56: 587–592.
Horrobin DF, Peet M . A dose ranging study of the effects of ethyl-eicosapentaenoate in patients with ongoing depression despite apparently adequate treatment with standard drugs. Arch Gen Psychiatry 2002; 59: 913–919.
Nemets B, Stahl Z, Beimaker RH . Addition of omega-3 fatty acid to maintenance medication treatment for recurrent unipolar depressive disorder. Am J Psychiatry 2002; 159: 477–479.
Bierut LJ, Heath AC, Bucholz KK, Dinwiddie SH, Madden PA, Statham DJ et al. Major depressive disorder in a community-based twin sample: are there different genetic and environmental contributions for men and women? Arch Gen Psychiatry 1999; 56: 557–563.
Kendler KS, Gardner CO, Neale MC, Prescott CA . Genetic risk factors for major depression in men and women: similar or different heritabilities and same or partly distinct genes. Psychol Med 2001; 31: 605–616.
Enoch M, Greenberger BD, Murphy DL, Goldman D . Sexually dimorphic relationship of a 5-HT(2A) promoter polymorphism with obsessive-compulsive disorder. Biol Psychiatry 2001; 49: 385–388.
Kokkonen P, Karvonen JT, Veijola J, Laksy K, Jokelainen J, Jarvelin MR et al. Prevalence and sociodemographic correlates of alexithymia in a population sample of young adults. Compr Psychiatry 2001; 42: 471–476.
Epperly TD, Moore KE . Health issues in men: part II. Common psychosocial disorders. Am Fam Physician 2000; 62: 117–124.
The European Academy of Allergology and Clinical Immunology. Position paper: allergen standardization and skin tests. Allergy 1993; 48 (Suppl 14): 48–82.
Acknowledgements
This study was supported by grants from the Allergiatutkimussäätiö (Foundation of Allergy Research).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Timonen, M., Jokelainen, J., Hakko, H. et al. Atopy and depression: results from the Northern Finland 1966 Birth Cohort Study. Mol Psychiatry 8, 738–744 (2003). https://doi.org/10.1038/sj.mp.4001274
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.mp.4001274
Keywords
This article is cited by
-
Association of atopic dermatitis with depressive symptoms and suicidal behaviors among adolescents in Korea: the 2013 Korean Youth Risk Behavior Survey
BMC Psychiatry (2017)
-
Mental Health in Allergic Rhinitis: Depression and Suicidal Behavior
Current Treatment Options in Allergy (2017)
-
Patient-reported allergies cause inferior outcomes after total knee arthroplasty
Knee Surgery, Sports Traumatology, Arthroscopy (2016)
-
The Psychological Burden of Skin Diseases: A Cross-Sectional Multicenter Study among Dermatological Out-Patients in 13 European Countries
Journal of Investigative Dermatology (2015)
-
The relationship between allergy and asthma control, quality of life, and emotional status in patients with asthma: a cross-sectional study
Allergy, Asthma & Clinical Immunology (2014)