Abstract
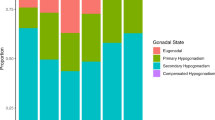
Hypogonadism, a disorder associated with aging, can cause significant morbidity. As clinical manifestations of hypogonadism can be subtle, the challenge and the burden of diagnosis remain the responsibility of the clinician. Four different analytic methods were used to predict hypogonadism in men based upon age, the presence of erectile dysfunction (ED) and depression. 218 men were classified by age, serum testosterone level, the presence of ED and depression. Depression was determined by the Center for Epidemiologic Studies Depression Scale (CES-D). ED was assessed by the Sexual Health Inventory for Men (SHIM). Hypogonadism was defined as a serum testosterone level <300 ng/dl. An artificial neural network (ANN) was programmed and trained to predict hypogonadism based upon age, SHIM, and CES-D scores. Subject data was randomly partitioned into a training set of 148 (67.9%) and a test set of 70 (32.1%). The ANN processed the test set only after the training was complete. The discrete predicted binary output was set to (0) if testosterone level was <300 ng/dl or (1) if >300 ng/dl. The data was also analyzed by standard logistic regression (LR), linear and quadratic discriminant function analysis (LDFA and QDFA, respectively). Reverse regression (RR) analysis evaluated the statistical significance of each risk factor. The ANN can accurately predict hypogonadism in men based upon age, the presence of ED, and depression (receiver-operating characteristic=0.725). A four hidden node network was found to have the highest accuracy. RR revealed the depression index score to be most significant variable (P=0.0019), followed by SHIM score (P=0.00602), and then by age (P=0.015). Hypogonadism can be predicated by an ANN using the input factors of age, ED, and depression. This model can help clinicians assess the need for endocrinologic evaluation in men.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 8 print issues and online access
$259.00 per year
only $32.38 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Harman SM, Metter EJ, Tobin JD, Pearson J, Blackman MR . The Baltimore Longitudinal Study of Again: Longitudinal effects of aging on serum total and free testosterone levels in health men. J Clin Endocrinol Metab 2001; 86: 724–731.
Morales A . The andropause: bare facts for urologists. Br J Urol 2003; 91: 311–313.
Wang C, Swedloff RS, Iranmanesh A, Dobs A, Snyder PJ, Cunningham G et al. Transdermal testosterone gel improves sexual function, mood, muscle strength, and body composition parameters in hypogonadal men. J Clin Endocrinol Metab 2000; 85: 2839–2853.
Radloff LS . The CES-D Scale: a self-report depression scale for research in the general population. Appl Psychol Meas 1977; 1: 385–401.
Capperelli JC, Siegal RL, Glasser DB, Osterloh IH, Rosen RC . Relationship between patient self-assessment of erectile dysfunction and the sexual health inventory for men. Clin Ther 2001; 3: 1707–1719.
Fiesler E, Beale R, Axelrod T, Blayo F, Cios KH, Doerschuk PI et al. Handbook of Neural Computation. New York: IOP Publishing and Oxford University Press, 1997, pp. G5 4: 1–6.
Werbos P . Beyond regression: new tools for prediction and analysis in the behavioral sciences. PhD Thesis. Cambridge, MA: Harvard University, 1974.
Golden RM . Mathematical Methods for Neural Network Analysis and Design. Cambridge, MA: MIT Press, 1996.
Michaels EK, Niederberger CS, Golden RM, Brown B, Cho L, Hong Y . Use of a neural network to predict stone growth after shock wave lithotripsy. Urology 1998; 51: 335–358.
Wickens TD . Elementary Signal Detection Theory. New York: Oxford University Press, 2002.
DeLong ER, DeLong DM, Clarke-Pearson DL . Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 1988; 44: 837–845.
Wespes E, Schulman CC . Male andropause: myth, reality, and treatment. Int J Impot Res 2002; 14: S93–S98.
Rubens R, Dhont M, Vermeulen A . Further studies on Leydig cell function in old age. J Clin Endocrinol Metab 1974; 39: 40–45.
Neaves WB, Johnson L, Porter JC, Parker Jr CR, Petty CS . Leydig cell numbers, daily sperm production, and serum gonadotropin levels in aging men. J Clin Endocrinol Metab 1984; 59: 756–763.
Szulc P, Claustrat B, Marchand F, Delmas PD . Increased risk of falls and increased bone resorption in elderly men with partial androgen deficiency: the MINOS study. J Clin Endocrinol Metab 2003; 88: 5240–5247.
Bacon CG, Mittleman MA, Kawachi I, Giovanucci E, Glasser DB, Rimm EB . Sexual function in men older than 50 years of age: results from the health professional follow-up study. Ann Intern Med 2003; 139: 161–168.
Tsujimura A, Matsumiya K, Matsuoka Y, Takahashi T, Koga M, Iwasa A et al. Bioavailable testosterone with age and erectile dysfunction. J Urol 2003; 170: 2345–2347.
Aversa A, Isidori AM, De Marino MU, Caprio M, Fabbrini E, Rocchietti-March M et al. Androgens and penile erection: evidence for a direct relationship between free testosterone and cavernous vasodilation in men with erectile dysfunction. Clin Endocrinol 2000; 53: 517–522.
Becker AJ, Ückert S, Stief CG, Truss MC, Machtens S, Friedemann S et al. Cavernous and systemic testosterone levels in different phases of human penile erection. Urology 2000; 56: 125–129.
Greenstein A, Plymate SR, Katz PG . Visually stimulated erection in castrated men. J Urol 1995; 153: 650–652.
Wald M, Seftel AD, Ross LS, Mohamed MAB, Niederberger CS . Computational models for detection of erectile dysfunction. J Urol 2005; 173: 167–174.
Rosen RC, Riley A, Wagner G, Osterloh IH, Kirkpatrick J, Mishra A . The International Index of Erectile Dysfunction (IIEF): a multidimensional scale for the assessment of erectile dysfunction. Urology 1997; 49: 823–830.
Shores MM, Sloan KL, Matsumoto AM, Moceri VM, Felker B, Kivlahan DR . Increased incidence of diagnosed depressive illness in hypogonadal older men. Arch Gen Psychiatry 2004; 61: 162–167.
Azad N, Pitale S, Barnes WE, Friedman N . Testosterone treatment enhances regional brain perfusion in hypogonadal men. J Clin Endocrinol Metab 2003; 88: 3064–3068.
Siedman SN, Rabkin JG . Testosterone replacement therapy for hypogonadal men with SSRI-refractory depression. J Affect Disord 1998; 48: 157–161.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kshirsagar, A., Seftel, A., Ross, L. et al. Predicting hypogonadism in men based upon age, presence of erectile dysfunction, and depression. Int J Impot Res 18, 47–51 (2006). https://doi.org/10.1038/sj.ijir.3901369
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijir.3901369
Keywords
This article is cited by
-
A systematic review of the applications of Expert Systems (ES) and machine learning (ML) in clinical urology
BMC Medical Informatics and Decision Making (2021)
-
Orthodontic Treatment Planning based on Artificial Neural Networks
Scientific Reports (2019)
-
Androgens and male aging: current evidence of safety and efficacy
Asian Journal of Andrology (2010)
-
Efficacy and safety of two different testosterone undecanoate formulations in hypogonadal men with metabolic syndrome
Journal of Endocrinological Investigation (2010)
-
Hypogonadism is associated with overt depression symptoms in men with erectile dysfunction
International Journal of Impotence Research (2008)