Abstract
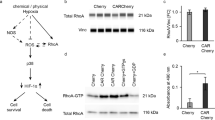
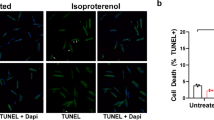
Hypoxia represents an endogenous pathophysiological signal underlying cell growth, adaptation and death in a variety of diseases, including ischemic heart diseases, stroke and solid tumors. A vigilant vector system depends on a gene switch which can sense the hypoxia signal occurring in ischemic events and turn on/off protective gene expressions when necessary. This system uses the oxygen-dependent degradation domain derived from hypoxia-inducible factor 1α as the hypoxia sensor and a double-vector system as signal amplifier. For treating ischemic heart diseases, a cardiac-specific MLC-2v promoter is used to deliver transgenes specifically to the heart. When tested in cardiomyocyte cultures, it produced a rapid and robust gene induction upon exposure to low oxygen. In a mouse model for myocardial infarction, the vigilant vectors turned on therapeutic genes such as heme oxygenase-1 in response to ischemia, significantly reduced apoptosis in the infarct area and improved cardiac functions. The hypoxia-regulated gene transfer afforded by the vigilant vectors may provide a powerful tool for delivering therapeutic proteins specifically to ischemic tissues with optimal physiological control.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Accession codes
References
Semenza GL et al. Hypoxia, HIF-1, and the pathophysiology of common human diseases. Adv Exp Med Biol 2000; 475: 123–130.
Acker T, Plate KH . A role for hypoxia and hypoxia-inducible transcription factors in tumor physiology. J Mol Med 2002; 80: 562–575.
Khan TA, Sellke FW, Laham RJ . Gene therapy progress and prospects: therapeutic angiogenesis for limb and myocardial ischemia. Gene Therapy 2003; 10: 285–291.
Lee RJ et al. VEGF gene delivery to myocardium: deleterious effects of unregulated expression. Circulation 2000; 102: 898–901.
Springer ML et al. VEGF gene delivery to muscle: potential role for vasculogenesis in adults. Mol Cell 1998; 2: 549–558.
Binley K et al. Hypoxia-mediated tumour targeting. Gene Therapy 2003; 10: 540–549.
Greco O et al. Novel chimeric gene promoters responsive to hypoxia and ionizing radiation. Gene Therapy 2002; 9: 1403–1411.
Su H, Arakawa-Hoyt J, Kan YW . Adeno-associated viral vector-mediated hypoxia response element-regulated gene expression in mouse ischemic heart model. Proc Natl Acad Sci USA 2002; 99: 9480–9485.
Ido A et al. Gene therapy targeting for hepatocellular carcinoma: selective and enhanced suicide gene expression regulated by a hypoxia-inducible enhancer linked to a human alpha-fetoprotein promoter. Cancer Res 2001; 61: 3016–3021.
Boast K et al. Characterization of physiologically regulated vectors for the treatment of ischemic disease. Hum Gene Ther 1999; 10: 2197–2208.
Binley K et al. An adenoviral vector regulated by hypoxia for the treatment of ischaemic disease and cancer. Gene Therapy 1999; 6: 1721–1727.
Ruan et al. A hypoxia-regulated adeno-associated virus vector for cancer-specific gene therapy. Neoplasia 2001; 3: 255–263.
Bainbridge JW et al. Hypoxia-regulated transgene expression in experimental retinal and choroidal neovascularization. Gene Therapy 2003; 10: 1049–1054.
Binley K et al. Long-term reversal of chronic anemia using a hypoxia-regulated erythropoietin gene therapy. Blood 2002; 100: 2406–2413.
Prentice H et al. Regulated expression of a foreign gene targeted to the ischaemic myocardium. Cardiovasc Res 1997; 35: 567–574.
Tang Y, Jackson M, Qian K, Phillips MI . Hypoxia inducible double plasmid system for myocardial ischemia gene therapy. Hypertension 2002; 39: 695–698.
Phillips M et al. Vigilant vector: heart-specific promoter in an adeno-associated virus vector for cardioprotection. Hypertension 2002; 39: 651–655.
Pachori AS et al. Hypoxia-regulated therapeutic gene as a preemptive treatment strategy against ischemia/reperfusion tissue injury. Proc Natl Acad Sci USA 2004; 101: 12282–12287.
Tang Y et al. Vigilant vectors: adeno-associated virus with a biosensor to switch on amplified therapeutic genes in specific tissues in life-threatening diseases. Methods 2002; 28: 259–266.
Semenza GL . HIF-1 and mechanisms of hypoxia sensing. Curr Opin Cell Biol 2001; 13: 167–171.
Salnikow K, Su W, Blagosklonny MV, Costa M . Carcinogenic metals induce hypoxia-inducible factor-stimulated transcription by reactive oxygen species-independent mechanism. Cancer Res 2000; 60: 3375–3378.
Richard DE, Berra E, Pouyssegur J . Nonhypoxic pathway mediates the induction of hypoxia-inducible factor 1alpha in vascular smooth muscle cells. J Biol Chem 2000; 275: 26765–26771.
Sandau KB, Fandrey J, Brune B . Accumulation of HIF-1alpha under the influence of nitric oxide. Blood 2001; 97: 1009–1015.
Stroka DM et al. HIF-1 is expressed in normoxic tissue and displays an organ-specific regulation under systemic hypoxia. FASEB J 2001; 15: 2445–2453.
Huang LE, Gu J, Schau M, Bunn HF . Regulation of hypoxia-inducible factor 1alpha is mediated by an O2-dependent degradation domain via the ubiquitin-proteasome pathway. Proc Natl Acad Sci USA 1998; 95: 7987–7992.
Sutter CH, Laughner E, Semenza GL . Hypoxia-inducible factor 1alpha protein expression is controlled by oxygen-regulated ubiquitination that is disrupted by deletions and missense mutations. Proc Natl Acad Sci USA 2000; 97: 4748–4753.
Wang Y, O'Malley Jr BW, Tsai SY, O'Malley BW . A regulatory system for use in gene transfer. Proc Natl Acad Sci USA. 1994; 91: 8180–8184.
O'Brien TX, Lee KJ, Chien KR . Positional specification of ventricular myosin light chain 2 expression in the primitive murine heart tube. Proc Natl Acad Sci USA 1993; 90: 5157–5161.
Mathey DG, Sheehan FH, Schofer J, Dodge HT . Time from onset of symptoms to thrombolytic therapy: a major determinant of myocardial salvage in patients with acute transmural infarction. J Am Coll Cardiol 1985; 6: 518–525.
Heyndrickx GR et al. Depression of regional blood flow and wall thickening after brief coronary occlusions. Am J Physiol 1978; 234: H653–H659.
Rumsey WL, Pawlowski M, Lejavardi N, Wilson DF . Oxygen pressure distribution in the heart in vivo and evaluation of the ischemic ‘border zone’. Am J Physiol 1994; 266: H1676–H1680.
Dekker M . Oxygenation of solid tumours. In: Teicher BA (ed). Drug Resistance in Oncology. Marcel Dekker, Inc.: New York, 1993.
Melo LG et al. Gene therapy strategy for long-term myocardial protection using adeno-associated virus-mediated delivery of heme oxygenase gene. Circulation 2002; 105: 602–607.
Vulapalli SR et al. Cardioselective overexpression of HO-1 prevents I/R-induced cardiac dysfunction and apoptosis. Am J Physiol Heart Circ Physiol 2002; 283: H688–H694.
Yet SF et al. Absence of heme oxygenase-1 exacerbates atherosclerotic lesion formation and vascular remodeling. FASEB J 2003; 17: 1759–1761.
Yet SF et al. Cardiac-specific expression of heme oxygenase-1 protects against ischemia and reperfusion injury in transgenic mice. Circ Res 2001; 89: 168–173.
Tang YL et al. Protection from ischemic heart injury by a vigilant heme oxygenase-1 plasmid system. Hypertension 2004; 43: 746–751.
Duan D, Yue Y, Yan Z, Engelhardt JF . A new dual-vector approach to enhance recombinant adeno-associated virus-mediated gene expression through intermolecular cis activation. Nat Med 2000; 6: 595–598.
Sun L, Li J, Xiao X . Overcoming adeno-associated virus vector size limitation through viral DNA heterodimerization. Nat Med 2000; 6: 599–602.
Nakai H, Storm TA, Kay MA . Increasing the size of rAAV-mediated expression cassettes in vivo by intermolecular joining of two complementary vectors. Nat Biotechnol 2000; 18: 527–532.
Rendahl KG et al. Regulation of gene expression in vivo following transduction by two separate rAAV vectors. Nat Biotechnol 1998; 16: 757–761.
Acknowledgements
We thank Dr Sean M Sullivan for providing pCMV and advice on the double vector system; Dr Gregg L Semenza for providing pCEP4/HIF-1alpha. This work was supported by the NIH MERIT award HL 27334 to MIP, Postdoctoral Fellowship from American Heart Association to Yao Liang Tang (0325378B) and Predoctoral Fellowship from American Heart Association to Yi Tang (0110140B).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tang, Y., Tang, Y., Zhang, Y. et al. A hypoxia-inducible vigilant vector system for activating therapeutic genes in ischemia. Gene Ther 12, 1163–1170 (2005). https://doi.org/10.1038/sj.gt.3302513
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.gt.3302513
Keywords
This article is cited by
-
Suxiao Jiuxin pill promotes exosome secretion from mouse cardiac mesenchymal stem cells in vitro
Acta Pharmacologica Sinica (2018)
-
Hypoxia fate mapping identifies cycling cardiomyocytes in the adult heart
Nature (2015)
-
Heme oxygenase-1: an emerging therapeutic target to curb cardiac pathology
Basic Research in Cardiology (2014)
-
Gene, Stem Cell, and Future Therapies for Orphan Diseases
Clinical Pharmacology & Therapeutics (2012)
-
Double Oxygen–sensing Vector System for Robust Hypoxia/Ischemia-regulated Gene Induction in Cardiac Muscle In Vitro and In Vivo
Molecular Therapy (2008)