Abstract
Study design: A case report.
Objectives: To report a case of swelling of the spinal cord and an intramedullary lesion occurring after expansive laminoplasty for cervical spondylotic myelopathy.
Setting: A university hospital in Japan.
Methods: Clinical evaluation, radiography, MR imaging.
Results: A 65-year-old man with a cervical spondylotic myelopathy in whom symptoms were improved immediately after expansive laminoplasty, but became aggravated 2 weeks later. Magnetic resonance images demonstrated swelling of the spinal cord and an intramedullary lesion that extended from the medulla oblongata to C7. Nine months after surgery, the lesion was reduced to C2–6, but neurological deterioration had not improved. Six years after surgery, the patient remains confined to bed.
Conclusion: Patients with such disease conditions are rare, and it is difficult to predict postoperative swelling of the spinal cord before surgery. Spine surgeons should be aware of such rare disease conditions involving the spinal cord.
Similar content being viewed by others
Introduction
Expansive laminoplasty is a method for decompressing the spinal cord by widening the stenotic spinal canal and by posterior shift of the spinal cord, which has been established as a surgical treatment for cervical myelopathy.1 In most patients, symptoms are improved immediately after laminoplasty, and long-term results are also satisfactory.1 However, there have been a few reports of patients who showed re-aggravation of myelopathy by intramedullary lesion of unknown cause after surgery.2,3,4
We report the changes in symptoms and magnetic resonance images (MRI) of a patient with cervical spondylotic myelopathy in whom symptoms were improved after laminoplasty but were aggravated 2 weeks after surgery with swelling of the spinal cord and a spindle-shaped intramedullary lesion that extended from the medulla oblongata to C7.
Case Report
The patient was diagnosed at the age of 45 years as having radiculopathy due to cervical disc herniation and underwent anterior discectomy and fusion at C5–6 and C6–7 in another hospital. The patient had no further symptoms, but dysesthesia of the bilateral long and ring fingertips appeared 18 years after the first surgery, and gradually extended to the whole bilateral upper and lower extremities. Since handling chopsticks, fastening and unfastening buttons, and walking became impossible, he was referred to our hospital at the age of 65 years.
Neurological examination revealed hyperreflexia in the bilateral upper and lower extremities and positive Hoffmann's reflex. There was a flexor plantar response. Muscle power was 4/5 in the upper and lower extremities. Light touch sensation was diminished in the regions below the middle part of the right forearm, below the left elbow, and under the T8 dermatome, while pin prick sensation was diminished in the regions below the bilateral wrists and the S3–5 dermatomes. Temperature sensation in the fingertips of both hands and in the regions below the left L4 dermatome was reduced, and vibration sensation was impaired in both legs and in both arms up to the elbows. Bladder dysfunction was exhibited with urinary retention. According to the Japanese Orthopaedic Association scoring system1 (highest score=17), the score of this patient was 4.
Blood examination was within normal ranges except for the erythrocyte sedimentation rate, which was slightly elevated (16 mm/h). Examination of cerebrospinal fluid (CSF) showed a normal level of proteins without an increase in the number of cells.
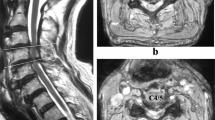
Plain film showed a slightly lordotic alignment of the cervical spine, complete anterior interbody fusion at C5–7, and retrolisthesis at C3 and C4. On the flexion-extension lateral plain film, C3–4 was stabilized by ossification of the anterior longitudinal ligament, and hypermobility was observed at C4–5. MRI demonstrated spinal cord compression at C3–4 and C4–5, and changes in the intramedullary signal intensity at C3–C5/6, which was also intense on T1-weighted image (T1WI) and high on T2-weighted image (T2WI) (Figure 1). Myelograms showed static cord compression at C3–4 and dynamic cord compression at C4–5 (Figure 2a,b).
From these results, the patient was diagnosed as having cervical spondylotic myelopathy. To rule out neuronal disorders such as multiple sclerosis, we consulted a neurologist who concurred with our diagnosis.
The patient underwent bilateral open laminoplasty at C3–7. Surgical treatment was completed without complications such as dural tears. Dysesthesia was alleviated immediately after surgery, and movements of the lower extremities were improved. The grip-and-release test (10 s test)5 was also improved from 7 times/10 s before surgery to 16 times/10 s after surgery. In the first week, the patient became delirious and stood up at night without any cervical orthosis several times, which we did not allow to continue. One week later, myelopathy was aggravated; then, the patient could no longer get up unassisted 6 weeks after surgery. On plain film, the lordotic alignment of the cervical spine was maintained. Two months after surgery, MRI revealed swelling of the spinal cord with a spindle-shaped intramedullary lesion, which showed low signal intensity on T1WI and high signal intensity on T2WI (Figure 3a). Five months after surgery, mild pseudo-bulbar palsy was observed, and the intramedullary lesion described above extended from the medulla oblongata to C7 (Figure 3b). This pseudo-bulbar palsy disappeared 7 months after surgery. Nine months after surgery, the lesion was reduced to C2–6, and this extent has persisted (Figure 3c). Gadolinium-DTPA enhancement showed horizontal linear lesions in the spinal cord at the C3/4 and C4/5 levels.
(a) A T2-weighted MR image 2 months after surgery revealing swelling of the spinal cord with a spindle-shaped intramedullary lesion, which shows high signal intensity. (b) A T2-weighted MR image 5 months after surgery demonstrating the intramedullary lesion extending from the medulla oblongata to C7. (c) A T2-weighted MR image 9 months after surgery demonstrating the swelling of the spinal cord reduced, and this extent has persisted
Six years after surgery, the patient remains confined to bed with a score of 0/17 on the Japanese Orthopaedic Association scoring system.
Discussion
There have been a number of reports of patients with intramedullary lesions observed by MRI after spinal cord injury or excision of a spinal cord tumor.6,7,8,9,10,11 Falcone et al6 considered that intramedullary lesions and swelling of the spinal cord observed after spinal cord injuries were enhanced by changes in local CSF dynamics caused by scar formation in the subarachnoid space, and called this disorder progressive post-traumatic myelomalacic myelopathy. Lee et al12 reported that this disorder was improved by untethering and expansive duraplasty.
For non-traumatic or non-neoplastic disorders, there have been a few reports of intramedullary lesions by MRI after surgery.2,3,4 However, to our knowledge, there have not been any reports of spinal cord enlargement and large intramedullary lesion as observed in our patient. In 1992, Okumura and Homma4 reported a patient with cervical spondylotic myelopathy whose disease course was clinically similar to that in our patient. In their patient, symptoms were improved immediately after surgery, then rapidly became aggravated without apparent cause 4 months after surgery. Swelling of the spinal cord was observed by MRI, and tumorous lesions in the spinal cord were imaged with Gadolinium-DTPA. The size of the lesions was reduced 15 months after surgery, with concomitant alleviation of symptoms, though the mechanism was unknown. Kato and Itoh3 reported four patients with acute diffuse spinal cord edema after laminoplasty. They considered the cause to involve irregular decompression at the kyphotic level, the re-perfusion mechanism, or iatrogenic spinal cord injuries.
Increased signal intensity in T2-weighted MR images in the patient with cervical myelopathy has been considered to reflect conditions such as myelomalacia, gliosis, edema, inflammation, ischemia, or necrosis,13,14,15 but the pathology has not yet been completely elucidated. In 1999, Fischbein et al16 considered that patients with lesions similar to those of our patient are in the ’presyrinx‘ state, and proposed that this state is due to obstruction of the CSF pathways.
In the current case, symptoms were alleviated immediately after surgery, then became aggravated 2 weeks later, which does not mean that the spinal cord was accidentally damaged at surgery. We might relate this aggravation to standing and movement without any cervical orthosis during the first week, which caused damage to the spinal cord due to C4–5 hypermobility. Additional anterior or posterior C4–5 stabilization might have prevented this condition. However, this is just a speculation, and the mechanism of this condition is not clear at this moment.
Conclusions
Patients with such disease conditions are rare, and the mechanism has not been established. Moreover, it is difficult to predict postoperative swelling of the spinal cord before surgery. Spine surgeons should be aware of such rare disease conditions.
References
Satomi K, Hirabayashi K . Ossification of the posterior longitudinal ligament In: Rothman RH, Simeone FA (eds) The Spine 3rd edn Philadelphia: WB Saunders 1992 pp 639–654
Itoh T et al. Two cases of cervical myelopathy showing spinal cord swelling after operation in MRI Rinshoseikeigeka (Jpn.) 1995 30: 755–759
Kato Y, Itoh T . En bloc laminoplasty for cervical myelopathy and acute diffuse spinal cord edema: Rapid decompression induces spinal cord edema? Cervical Spine Research Society (Program of 26th annual meeting) 1998 122–123 Abstract
Okumura H, Homma T . Tumor-like finding in MRI after decompression for cervical spondylotic myelopathy Seikeigeka (Jpn.) 1992 43: 41–46
Ono K et al. Myelopathy hand: New clinical signs of cervical cord damage J Bone Joint Surg 1987 69-B: 215–219
Falcone S et al. Progressive posttraumatic myelomalacic myelopathy: Imaging and clinical features Am J Neuroradiol 1994 15: 747–754
Fox JL et al. Central spinal cord injury: Magnetic resonance imaging confirmation and operative considerations Neurosurgery 1988 22: 340–347
Gebarski SS et al. Posttraumatic progressive myelopathy: Clinical and radiologic correlation employing MR imaging, delayed CT metrizamide myelography, and intraoperative sonography Radiology 1985 157: 379–385
MacDonald RL, Findlay JM, Tator CH . Microcystic spinal cord degeneration causing posttraumatic myelopathy: Report of two cases J Neurosurg 1988 68: 466–471
Ragnarsson TS, Durward QJ, Nordgren RE . Spinal cord tethering after traumatic paraplegia with late neurological deterioration J Neurosurg 1986 64: 397–401
Schwartz ED, Falcone SF, Quencer RM, Green BA . Posttraumatic syringomyelia: Pathogenesis, imaging, and treatment AJR 1999 173: 487–492
Lee TT et al. Progressive posttraumatic myelomalacic myelopathy: Treatment with untethering and expansive duraplasty J Neurosurg 1997 86: 624–628
Mehalic TF, Pezzuti RT, Applebraum BI . Magnetic resonance imaging and cervical spondylotic myelopathy Neurosurgery 1990 26: 217–227
Ohshio I et al. Correlation between histopathologic features and magnetic resonance images of spinal cord lesions Spine 1993 18: 1140–1149
Takahashi M, Yamashita Y, Sakamoto Y, Kojima R . Chronic cervical cord compression: Clinical significance of increased signal intensity on MR images Radiology 1989 173: 219–224
Fischbein NJ, Dillon WP, Cobbs C, Weinstein PR . The ’’presyrinx‘‘ state: A reversible myelopathic condition that may precede syringomyelia Am J Neuroradiol 1999 20: 7–20
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Nagashima, H., Morio, Y. & Teshima, R. Re-aggravation of myelopathy due to intramedullary lesion with spinal cord enlargement after posterior decompression for cervical spondylotic myelopathy: serial magnetic resonance evaluation. Spinal Cord 40, 137–141 (2002). https://doi.org/10.1038/sj.sc.3101262
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101262
Keywords
This article is cited by
-
Assessment of the treatment response of spinal meningiomas after radiosurgery focusing on serial MRI findings
Japanese Journal of Radiology (2015)
-
Do intramedullary spinal cord changes in signal intensity on MRI affect surgical opportunity and approach for cervical myelopathy due to ossification of the posterior longitudinal ligament?
European Spine Journal (2011)
-
Clinical significance of intramedullary Gd-DTPA enhancement in cervical myelopathy
Spinal Cord (2010)