Abstract
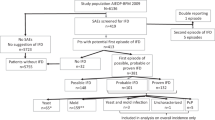
In patients with hematologic malignancy, invasive aspergillosis continues to be associated with high mortality even when treated with conventional antifungal therapy. To investigate novel antifungal agents, we compared 53 patients who received posaconazole salvage therapy to 52 contemporary control patients who received high-dose lipid formulation of amphotericin B (HD-LPD/AMB at ⩾7.5 mg kg−1 per day) and 38 other control patients who received caspofungin plus HD-LPD/AMB. Patients in the three groups had similar. The overall response rate to salvage therapy was 40% for posaconazole, 8% for HD-LPD/AMB (P⩽0.001) and 11% for combination therapy (P<0.002). Aspergillosis contributed to the death of 40% of posaconazole group, 65% of the HD-LPD/AMB group and 68% of the combination group (P⩽0.008). By multivariate analysis, posaconazole therapy independently improved response (9.5; 95% confidence interval, 2.8–32.5; P<0.001). HD-LPD/AMB alone or in combination was associated with a significantly higher rate of nephrotoxicity (P⩽0.02) and hepatotoxicity (P<0.03). In conclusion, posaconazole salvage therapy demonstrated greater efficacy and safety than HD-LPD/AMB alone or in combination with caspofungin in the salvage therapy of invasive aspergillosis in hematologic malignancy.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Patterson TF, Kirkpatrick WR, White M, Hiemenz JW, Wingard JR, Dupont B et al. Invasive aspergillosis: disease spectrum, treatment practices, and outcomes. Medicine 2000; 79: 250–260.
Marr KA, Patterson T, Denning DW . Aspergillosis: pathogenesis, clinical manifestations, and therapy. Infect Dis Clin North Am 2002; 16: 875–894.
Kontoyiannis DP, Bodey GP . Invasive aspergillosis in 2002: an update. Eur J Clin Microbiol Infect Dis 2002; 21: 161–172.
Upton A, Kirby KA, Carpenter P, Boeckh M, Marr KA . Invasive aspergillosis following hematopoietic cell transplantation: outcomes and prognostic factors associated with mortality. Clin Infect Dis 2007; 44: 531–540.
Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, et al., Invasive Fungal Infections Group of the European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med 2002; 347: 408–415.
Patterson TF, Boucher HW, Herbrecht R, Denning DW, Lortholary O, Ribaud P, et al., European Organisation for Research and Treatment of Cancer and the Global Aspergillus Study Group; Pfizer Global Aspergillus Study Group. Strategy of following voriconazole versus amphotericin B therapy with other licensed antifungal therapy for primary treatment of invasive aspergillosis: impact of other therapies on outcome. Clin Infect Dis 2005; 41: 1448–1452.
Torres HA, Hachem RY, Chemaly RF, Kontoyiannis DP, Raad II . Posaconazole: a broad-spectrum triazole antifungal. Lancet Infect Dis 2005; 5: 775–785.
Herbrecht R . Posaconazole: a potent, extended-spectrum triazole anti-fungal for the treatment of serious fungal infections. Int J Clin Pract 2004; 58: 612–624.
Hachem RY, Kontoyiannis DP, Boktour MR, Afif C, Cooksley C, Bodey GP et al. Aspergillus terreus: an emerging amphotericin B-resistant opportunistic mold in patients with hematologic malignancies. Cancer 2004; 101: 1594–1600.
Walsh TJ, Raad I, Patterson TF, Chandrasekar P, Donowitz GR, Graybill R et al. Treatment of invasive aspergillosis with posaconazole in patients who are refractory to or intolerant of conventional therapy: an externally controlled trial. Clin Infect Dis 2007; 44: 2–12.
Gavalda J, Martin T, Lopez P, Gomis X, Ramirez JL, Rodriguez D et al. Efficacy of high loading doses of liposomal amphotericin B in the treatment of experimental invasive pulmonary aspergillosis. Clin Microbiol Infect 2005; 11: 999–1004.
Martin MT, Gavalda J, Lopez P, Gomis X, Ramirez JL, Rodriguez D et al. Efficacy of high doses of liposomal amphotericin B in the treatment of experimental aspergillosis. J Antimicrob Chemother 2003; 52: 1032–1034.
Walsh TJ, Goodman JL, Pappas P, Bekersky I, Buell DN, Roden M et al. Safety, tolerance, and pharmacokinetics of high-dose liposomal amphotericin B (AmBisome) in patients infected with Aspergillus species and other filamentous fungi: maximum tolerated dose study. Antimicrob Agents Chemother 2001; 45: 3487–3496.
Ellis M, Watson R, McNabb A, Lukic ML, Nork M . Massive intracerebral aspergillosis responding to combination high dose liposomal amphotericin B and cytokine therapy without surgery. J Med Microbiol 2002; 51: 70–75.
Ryan C, McNicholsan S, O'Connell B, Forde S, Keoghan M, McCann SR . An epidemic of invasive fungal infection in a stem cell transplant unit: response to high dose liposomal amphotericin B. Hematol J 2004; 5: 548–551.
Caillot D, Thiebaut A, Herbrecht R, de Botton S, Pigneux A, Bernard F et al. Liposomal amphotericin B in combination with caspofungin versus liposomal amphotericin B high dose regimen for the treatment of invasive aspergillosis in immunocompromised patients: randomized pilot study (Combistrat Trial). Paper presented at 16th Congress of the International Society for Human and Animal Mycology (Focus on Fungal Infections 16). 8–10 March 2006; Las Vegas, NV.
Kontoyiannis DP, Andersson BS, Lewis RE, Raad II . Progressive disseminated aspergillosis in a bone marrow transplant recipient: response with a high-dose lipid formulation of amphotericin B. Clin Infect Dis 2001; 32: E94–E96.
Arikan S, Lozano-Chiu M, Paetznick V, Rex JH . In vitro synergy of caspofungin and amphotericin B against Aspergillus and Fusarium spp. Antimicrob Agents Chemother 2002; 46: 245–247.
Aliff TB, Maslak PG, Jurcic JG, Heaney ML, Cathcart KN, Sepkowitz KA et al. Refractory Aspergillus pneumonia in patients with acute leukemia: successful therapy with combination caspofungin and liposomal amphotericin. Cancer 2003; 97: 1025–1032.
Maertens J, Glasmacher A, Herbrecht R, Thiebaut A, Cordonnier C, Segal BH, et al., Caspofungin Combination Therapy Study Group. Multicenter, noncomparative study of caspofungin in combination with other antifungals as salvage therapy in adults with invasive aspergillosis. Cancer 2006; 107: 2888–2897.
Ascioglu S, Rex JH, de Pauw B, Bennett JE, Bille J, Crokaert F, et al., Invasive Fungal Infections Cooperative Group of the European Organization for Research and Treatment of Cancer; Mycoses Study Group of the National Institute of Allergy and Infectious Diseases. Defining opportunistic invasive fungal infections in immunocompromised patients with cancer and hematopoietic stem cell transplants: an international consensus. Clin Infect Dis 2002; 34: 7–14.
Hiemenz JW, Walsh TJ . Lipid formulations of amphotericin B: recent progress and future directions. Clin Infect Dis 1996; 22 (Suppl 2): 133–144.
Walsh TJ, Finberg RW, Arndt C, Hiemenz J, Schwartz C, Bodensteiner D et al. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectious Diseases Mycoses Study Group. N Engl J Med 1999; 340: 764–771.
Walsh TJ, Petraitis V, Petraitiene R, Field-Ridley A, Sutton D, Ghannoum M et al. Experimental pulmonary aspergillosis due to Aspergillus terreus: pathogenesis and treatment of an emerging fungal pathogen resistant to amphotericin B. J Infect Dis 2003; 188: 305–319.
Espinel-Ingroff A . Comparison of in vitro activities of the new triazole SCH56592 and the echinocandins MK-0991 (L-743, 872) and LY303366 against opportunistic filamentous and dimorphic fungi and yeasts. J Clin Microbiol 1998; 36: 2950–2956.
Maertens J, Raad I, Petrikkos G, Boogaerts M, Selleslag D, Petersen FB, et al., Caspofungin Salvage Aspergillosis Study Group. Efficacy and safety of caspofungin for treatment of invasive aspergillosis in patients with refractory to or intolerant of conventional antifungal therapy. Clin Infect Dis 2004; 39: 1563–1571.
Kartsonis NA, Saah AJ, Joy Lipka C, Taylor AF, Sable CA . Salvage therapy with caspofungin for invasive aspergillosis: results from the caspofungin compassion use study. J Infect 2005; 50: 196–205.
Kontoyiannis DP, Hachem R, Lewis RE, Rivero GA, Torres HA, Thornby J et al. Efficacy and toxicity of caspofungin in combination with liposomal amphotericin B as primary or salvage treatment of invasive aspergillosis in patients with hematologic malignancies. Cancer 2003; 98: 292–299.
Petraitiene R, Petraitis V, Groll AH, Sein T, Piscitelli S, Candelario M et al. Antifungal activity and pharmacokinetics of posaconazole (SCH56592) in treatment and prevention of experimental invasive pulmonary aspergillosis: correlation with galactomannan antigenemia. Antimicrob Agents Chemother 2001; 45: 857–869.
Najvar LK, Cacciapuoti A, Hernandez S, Halpern J, Bocanegra R, Gurnani M et al. Activity of posaconazole combined with amphotericin B against Aspergillus flavus infection in mice: comparative studies in two laboratories. Antimicrob Agents Chemother 2004; 48: 758–764.
Krishna G, Wexler D, Shah A, Martinho M, Patino H . The Pharmacokinetics of Oral Posaconazole in Recipients of Allogeneic Hematopoietic Stem Cell Transplantation with Graft-versus-Host Disease. Paper presented at 45th Annual Interscience Conference on Antimicrobial Agents and Chemotherapy; 16–19 December 2005; Washington, DC.
Sansone-Parsons A, Krishna G, Calzetta A, Wexler D, Kantesaria B, Rosenberg MA et al. Effect of a nutritional supplement on posaconazole pharmacokinetics following oral administration to healthy volunteers. Antimicrob Agents Chemother 2006; 50: 1881–1883.
Boucher HW, Groll AH, Chiou CC, Walsh TJ . New systemic antifungal agents: pharmacokinetics, safety and efficacy. Drugs 2004; 64: 1997–2020.
Spanakis EK, Aperis G, Mylonakis E . New agent for the treatment of fungal infections: clinical efficacy and gaps in coverage. Clin Infect Dis 2006; 43: 1060–1068.
Ullmann AJ, Lipton JH, Vesole DH, Chandrasekar P, Langston A, Tarantolo SR et al. Posaconazole or fluconazole for prophylaxis in severe graft-versus-host-disease. N Engl J Med 2007; 356: 335–347.
Raad II, Graybill JR, Bustamante AB, Cornely OA, Gaona-Flores V, Afif C et al. Safety of long-term oral posaconazole in the treatment of refractory invasive fungal infections. Clin Infect Dis 2006; 42: 1726–1734.
Cornely OA, Maertens J, Bresnik M, Ebrahimi R, Ullmann AJ, Bouza E, et al., AmBiLoad Trial Study Group. Liposomal amphotericin B as initial therapy for invasive mold infection: a randomized trial comparing a high-loading dose regimen with standard dosing (AmBiLoad Trial). Clin Infect Dis 2007; 44: 1289–1297.
Acknowledgements
Issam I Raad designed the study and wrote the paper. Hend Hanna did the statistical analysis. Maha Boktour and Harrys Torres coordinated the data collection. Claude Afif and Dimitrios P Kontoyiannis followed up on the patients. Ray Y Hachem coordinated the study and assisted Issam I Raad in writing the paper. Grant support received from Schering-Plough Research Institute, Merck & Co., Enzon, Fujisawa (Astellas).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Raad, I., Hanna, H., Boktour, M. et al. Novel antifungal agents as salvage therapy for invasive aspergillosis in patients with hematologic malignancies: posaconazole compared with high-dose lipid formulations of amphotericin B alone or in combination with caspofungin. Leukemia 22, 496–503 (2008). https://doi.org/10.1038/sj.leu.2405065
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2405065
Keywords
This article is cited by
-
Updates in the Treatment of Breakthrough Mold Infections
Current Fungal Infection Reports (2020)
-
Posaconazole Salvage Treatment for Invasive Fungal Infection
Mycopathologia (2014)
-
Treatment of invasive fungal infections in cancer patients—updated recommendations of the Infectious Diseases Working Party (AGIHO) of the German Society of Hematology and Oncology (DGHO)
Annals of Hematology (2014)
-
Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (Part 1)
Critical Care (2013)
-
Section 3: Prevention and Treatment of AKI
Kidney International Supplements (2012)