Abstract
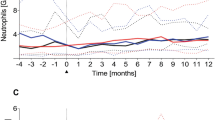
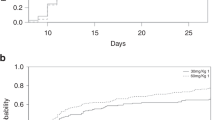
Large granular lymphocyte (LGL) proliferation typically follows a chronic course during which major features are cytopenia and immune abnormalities. Elevated numbers of LGL were reported in a few cases following allogeneic stem cell transplantation (allo-SCT). In this report, we present a retrospective analysis of LGL cases that occurred following allo-SCT in a cohort of 201 consecutive patients transplanted over a period of 7 years. Six cases were identified and LGL expansion occurred more frequently following a reduced fludarabine and anti-T lymphocyte globulin-based preparative regimen (4 cases/49), than after a conventional myeloablative regimen (2 cases/152). Expansion of LGL was seen between 3 and 15 months following allo-SCT. Hematopoiesis, with mild to severe cytopenia, was a favored target for LGL. Autoimmune manifestations including polyarthritis and hypergammaglobulinemia were also observed. LGL proliferation was observed in the context of chronic antigenic stimulation associated with recurrent viral infections especially CMV. Moreover, five out of these six high risk patients achieved a long-term complete remission concomitant or following LGL expansion. These data suggest that LGL might be a subset of effector lymphocytes which may participate to the graft-versus-tumor effect.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
McKenna RW, Parkin J, Kersey JH, Gajl-Peczalska KJ, Peterson L, Brunning RD . Chronic lymphoproliferative disorder with unusual clinical, morphologic, ultrastructural and membrane surface marker characteristics Am J Med 1977 62: 588–596
Wang EC, Lehner PJ, Graham S, Borysiewicz LK . CD8high (CD57+) T cells in normal, healthy individuals specifically suppress the generation of cytotoxic T lymphocytes to Epstein–Barr virus-transformed B cell lines Eur J Immunol 1994 24: 2903–2909
Airo P, Rossi G, Facchetti F, Marocolo D, Garza L, Lanfranchi A, Prati E, Brugnoni D, Malacarne F, Cattaneo R . Monoclonal expansion of large granular lymphocytes with a CD4+ CD8dim+/− phenotype associated with hairy cell leukemia Haematologica 1995 80: 146–149
Loughran TP Jr . Clonal diseases of large granular lymphocytes Blood 1993 82: 1–14
Mollet L, Fautrel B, Leblond V, Bergeron F, Merle-Beral H, Baumelou E, Hubert P, Debre P, Autran B . Leukemic CD3+ LGL share functional properties with their CD8+ CD57+ cell counterpart expanded after BMT Leukemia 1999 13: 230–240
Brenner MK, Reittie JE, Grob JP, Wimperis JZ, Stephens S, Patterson J, Hoffbrand AV, Prentice HG . The contribution of large granular lymphocytes to B cell activation and differentiation after T-cell-depleted allogeneic bone marrow transplantation Transplantation 1986 42: 257–261
Niederwieser D, Gastl G, Rumpold H, Marth C, Kraft D, Huber C . Rapid reappearance of large granular lymphocytes (LGL) with concomitant reconstitution of natural killer (NK) activity after human bone marrow transplantation (BMT) Br J Haematol 1987 65: 301–305
Sajeva MR, Greco MM, Cascavilla N, D'Arena G, Scalzulli P, Melillo L, Minervini MM, Bonini A, Di Mauro L, Carotenuto M, Musto P . Effective autologous peripheral blood stem cell transplantation in plasma cell leukemia followed by T-large granular lymphocyte expansion: a case report Bone Marrow Transplant 1996 18: 225–227
Dolstra H, Preijers F, Van de Wiel-van Kemenade E, Schattenberg A, Galama J, de Witte T . Expansion of CD8+CD57+ T cells after allogeneic BMT is related with a low incidence of relapse and with cytomegalovirus infection Br J Haematol 1995 90: 300–307
Gentile TC, Hadlock KG, Uner AH, Delal B, Squiers E, Crowley S, Woodman RC, Foung SK, Poiesz BJ, Loughran TP Jr . Large granular lymphocyte leukaemia occurring after renal transplantation Br J Haematol 1998 101: 507–512
Leroy E, Calvo CF, Divine M, Gourdin MF, Baujean F, Ben Aribia MH, Mishal Z, Vernant JP, Farcet JP, Senik A . Persistence of T8+/HNK-1+ suppressor lymphocytes in the blood of long-term surviving patients after allogeneic bone marrow transplantation J Immunol 1986 137: 2180–2189
Sadat-Sowti B, Debre P, Idziorek T, Guillon JM, Hadida F, Okzenhendler E, Katlama C, Mayaud C, Autran B . A lectin-binding soluble factor released by CD8+CD57+ lymphocytes from AIDS patients inhibits T cell cytotoxicity Eur J Immunol 1991 21: 737–741
Clement LT, Grossi CE, Gartland GL . Morphologic and phenotypic features of the subpopulation of Leu-2+ cells that suppresses B cell differentiation J Immunol 1984 133: 2461–2468
Halwani F, Guttmann RD, Ste-Croix H, Prud'homme GJ . Identification of natural suppressor cells in long-term renal allograft recipients Transplantation 1992 54: 973–977
Mollet L, Sadat-Sowti B, Duntze J, Leblond V, Bergeron F, Calvez V, Katlama C, Debre P, Autran B . CD8hi+CD57+ T lymphocytes are enriched in antigen-specific T cells capable of down-modulating cytotoxic activity Int Immunol 1998 10: 311–323
Mohty M, Faucher C, Gaugler B, Vey N, Sainty D, Arnoulet C, Mozziconacci MJ, Isnardon D, Gastaut JA, Maraninchi D, Olive D, Blaise D . Large granular lymphocytes (LGL) following non-myeloablative allogeneic bone marrow transplantation: a case report Bone Marrow Transplant 2001 28: 1157–1160
Mohty M, Faucher C, Vey N, Stoppa AM, Viret F, Chabbert I, Chabannon C, Bouabdallah R, Ladaique P, Collet L, Zandotti C, Maraninchi D, Blaise D . High rate of secondary viral and bacterial infections in patients undergoing allogeneic bone marrow mini-transplantation Bone Marrow Transplant 2000 26: 251–255
Hamidou M, Lamy T . Large granular lymphocyte proliferations. Clinical and pathogenic aspects Rev Med Interne 2001 22: 452–459
Semenzato G, Zambello R, Starkebaum G, Oshimi K, Loughran TP Jr . The lymphoproliferative disease of granular lymphocytes: updated criteria for diagnosis Blood 1997 89: 256–260
Semenzato G, Pandolfi F, Chisesi T, De Rossi G, Pizzolo G, Zambello R, Trentin L, Agostini C, Dini E, Vespignani M, Cafaro A, Pasqualetti D, Giubellino MC, Migone N, Foa R . The lymphoproliferative disease of granular lymphocytes. A heterogeneous disorder ranging from indolent to agressive conditions Cancer 1987 60: 2971–2978
Mohty M, Jarrossay D, Lafage-Pochitaloff M, Zandotti C, Briere F, de Lamballeri XN, Isnardon D, Sainty D, Olive D, Gaugler B . Circulating blood dendritic cells from myeloid leukemia patients display quantitative and cytogenetic abnormalities as well as functional impairment Blood 2001 98: 3750–3756
Horowitz MM, Gale RP, Sondel PM, Goldman JM, Kersey J, Kolb HJ, Rimm AA, Ringden O, Rozman C, Speck B, Truitt RL, Zwaan FE, Bortin MM . Graft-versus-leukemia reactions after bone marrow transplantation Blood 1990 75: 555–562
Zambello R, Loughran TP Jr, Trentin L, Pontisso P, Battistella L, Raimondi R, Facco M, Sancetta R, Agostini C, Pizzolo G, Semenzato G . Serologic and molecular evidence for a possible pathogenetic role of viral infection in CD3-negative natural killer-type lymphoproliferative disease of granular lymphocytes Leukemia 1995 9: 1207–1211
Wang EC, Moss PA, Frodsham P, Lehner PJ, Bell JI, Borysiewicz LK . CD8highCD57+ T lymphocytes in normal, healthy individuals are oligoclonal and respond to human cytomegalovirus J Immunol 1995 155: 5046–5056
Slavin S, Nagler A, Naparstek E, Kapelushnik Y, Aker M, Cividalli G, Varadi G, Kirschbaum M, Ackerstein A, Samuel S, Amar A, Brautbar C, Ben-Tal O, Eldor A, Or R . Nonmyeloablative stem cell transplantation and cell therapy as an alternative to conventional bone marrow transplantation with lethal cytoreduction for the treatment of malignant and nonmalignant hematologic diseases Blood 1998 91: 756–763
Mohty M, Fegueux N, Exbrayat C, Lu ZY, Legouffe E, Quittet P, Lopez-Martinez E, Latry P, Avinens O, Hertog C, Klein B, Eliaou JF, Rossi JF . Reduced intensity conditioning: enhanced graft-versus-tumor effect following dose-reduced conditioning and allogeneic transplantation for refractory lymphoid malignancies after high-dose therapy Bone Marrow Transplant 2001 28: 335–339
Badros A, Barlogie B, Morris C, Desikan R, Martin SR, Munshi N, Zangari M, Mehta J, Toor A, Cottler-Fox M, Fassas A, Anaissie E, Schichman S, Tricot G, Aniassie E . High response rate in refractory and poor-risk multiple myeloma after allotransplantation using a nonmyeloablative conditioning regimen and donor lymphocyte infusions Blood 2001 97: 2574–2579
Morecki S, Gelfand Y, Nagler A, Or R, Naparstek E, Varadi G, Engelhard D, Akerstein A, Slavin S . Immune reconstitution following allogeneic stem cell transplantation in recipients conditioned by low intensity vs myeloablative regimen Bone Marrow Transplant 2001 28: 243–249
Nahill SR, Welsh RM . High frequency of cross-reactive cytotoxic T lymphocytes elicited during the virus-induced polyclonal cytotoxic T lymphocyte response J Exp Med 1993 177: 317–327
Burrows SR, Khanna R, Burrows JM, Moss DJ . An alloresponse in humans is dominated by cytotoxic T lymphocytes (CTL) cross-reactive with a single Epstein–Barr virus CTL epitope: implications for graft-versus-host disease J Exp Med 1994 179: 1155–1161
Zambello R, Trentin L, Facco M, Siviero M, Galvan S, Piazza F, Perin A, Agostini C, Semenzato G . Analysis of TNF-receptor and ligand superfamily molecules in patients with lymphoproliferative disease of granular lymphocytes Blood 2000 96: 647–654
Camagna A, Cedrone L, Care A, Samoggia P, De Marco MC, Del Duca P, De Martinis C, Testa U . Polyclonal expansion of CD3(+)/CD4(+)/CD56(+) large granular lymphocytes and autoimmunity associated with dysregulation of Fas/FasL apoptotic pathway Br J Haematol 2001 112: 204–207
Lamy T, Liu JH, Landowski TH, Dalton WS, Loughran TP Jr . Dysregulation of CD95/CD95 ligand-apoptotic pathway in CD3(+) large granular lymphocyte leukemia Blood 1998 92: 4771–4777
Ferrara JL, Guillen FJ, van Dijken PJ, Marion A, Murphy GF, Burakoff SJ . Evidence that large granular lymphocytes of donor origin mediate acute graft-versus-host disease Transplantation 1989 47: 50–54
Tsao PW, Mills GB, Diaz RJ, Radde IC, Martell MF, Augustine JM, Parkinson D, Waddell J, Wilson GJ, Coles JG . Identification of a subpopulation of reactive large granular mononuclear cells in allogeneic heart transplantation J Heart Lung Transplant 1993 12: 230–238
Koskinen PK, Krogerus LA, Nieminen MS, Mattila SP, Hayry PJ, Lautenschlager IT . Cytomegalovirus infection-associated generalized immune activation in heart allograft recipients: a study of cellular events in peripheral blood and endomyocardial biopsy specimens Transplant Intl 1994 7: 163–171
Acknowledgements
M Mohty was supported by a grant from the ‘Société Française de Greffe de Moelle et de Thérapie Cellulaire (SFGM-TC)’, and from the ‘Fondation de France’ (Paris, France). We thank B Calmels (CTCG, Institut Paoli-Calmettes) for helpful discussions. This work was made possible through access to the tumor cell collection of the Biothèque-Tumorothèque at the Institut Paoli-Calmettes.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Mohty, M., Faucher, C., Vey, N. et al. Features of large granular lymphocytes (LGL) expansion following allogeneic stem cell transplantation: a long-term analysis. Leukemia 16, 2129–2133 (2002). https://doi.org/10.1038/sj.leu.2402645
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.leu.2402645
Keywords
This article is cited by
-
Expansion of large granular lymphocytes after autologous hematopoietic stem cell transplantation
International Journal of Hematology (2023)
-
T-cell clones of uncertain significance are highly prevalent and show close resemblance to T-cell large granular lymphocytic leukemia. Implications for laboratory diagnostics
Modern Pathology (2020)
-
Proportion of Cytotoxic Peripheral Blood Natural Killer Cells and T-Cell Large Granular Lymphocytes in Recurrent Miscarriage and Repeated Implantation Failure: Case–Control Study and Meta-analysis
Archivum Immunologiae et Therapiae Experimentalis (2019)
-
Divergent roles for antigenic drive in the aetiology of primary versus dasatinib-associated CD8+ TCR-Vβ+ expansions
Scientific Reports (2018)
-
Lymphocyte expansion after unrelated cord blood allogeneic stem cell transplantation in adults
Bone Marrow Transplantation (2017)