Summary:
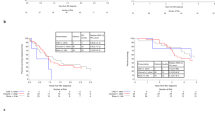
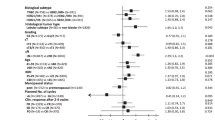
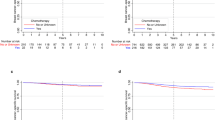
The prognosis of inflammatory breast cancer (IBC) is poor. We evaluated clinical and biopathological characteristics that could affect survival in 74 women with nonmetastatic IBC consecutively treated in our institution between 1976 and 2000. Patients received primary anthracycline-based chemotherapy at conventional doses (n=20) or high-dose chemotherapy (HDC) with haematopoietic stem cell support (HSCS) (n=54). After chemotherapy, 84% of patients underwent mastectomy, 95% were given radiotherapy and 55% tamoxifen. Immunohistochemistry data (ER, PR, ERBB2, P53) on pre-chemotherapy specimens suggested strong differences between IBC and non-IBC. The rate of pathological complete response to chemotherapy was 26% (27% with HDC and 17% with conventional doses, not significant). No single factor was found predictive of response. With a median follow-up of 48 months after diagnosis, the 5-year projected disease-free survival (DFS) was 24% and overall survival (OS) 41%. In multivariate analysis, the strongest independent prognostic factor was the delivery of HDC. The 5-year DFS and OS of patients were respectively 28 and 50% with HDC and 15 and 18% with conventional chemotherapy. These results and comparisons with other series of patients suggest a role for HDC with HSCS as part of the therapeutic approach in IBC. Further prospective studies are required to confirm it.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Jaiyesimi IA, Buzdar AU, Hortobagyi G . Inflammatory breast cancer: a review. J Clin Oncol 1992; 10: 1014–1024.
Chang S, Parker SL, Pham T et al. Inflammatory breast carcinoma incidence and survival: the surveillance, epidemiology, and end results program of the National Cancer Institute, 1975–1992. Cancer 1998; 82: 2366–2372.
Buzdar AU, Singletary SE, Booser DJ et al. Combined modality treatment of stage III and inflammatory breast cancer. M.D. Anderson Cancer Center experience. Surg Oncol Clin N Am 1995; 4: 715–734.
Maloisel F, Dufour P, Bergerat JP et al. Results of initial doxorubicin, 5-fluorouracil, and cyclophosphamide combination chemotherapy for inflammatory carcinoma of the breast. Cancer 1990; 65: 851–855.
Palangie T, Mosseri V, Mihura J et al. Prognostic factors in inflammatory breast cancer and therapeutic implications. Eur J Cancer 1994; 7: 921–927.
Cristofanilli M, Buzdar AU, Sneige N et al. Paclitaxel in the multimodality treatment for inflammatory breast carcinoma. Cancer 2001; 92: 1775–1782.
Jacquemier J, Charpin C . Reproducibility of histoprognostic grades of invasive breast cancer. Ann Pathol 1998; 18: 385–390.
Ginestier C, Charafe-Jauffret E, Bertucci F et al. Distinct and complementary information provided by use of tissue and DNA microarrays in the study of breast tumor markers. Am J Pathol 2002; 161: 1223–1233.
Chevallier B, Chollet P, Merrouche Y et al. Lenograstim prevents morbidity from intensive induction chemotherapy in the treatment of inflammatory breast cancer. J Clin Oncol 1995; 13: 1564–1571.
Viens P, Palangie T, Janvier M et al. First-line high-dose sequential chemotherapy with rG-CSF and repeated blood stem cell transplantation in untreated inflammatory breast cancer: toxicity and response (PEGASE 02 trial). Br J Cancer 1999; 81: 449–456.
Guerin M, Gabillot M, Mathieu MC et al. Structure and expression of c-erbB-2 and EGF receptor genes in inflammatory and non-inflammatory breast cancer: prognostic significance. Int J Cancer 1989; 43: 201–208.
Moll UM, Riou G, Levine AJ . Two distinct mechanisms alter p53 in breast cancer: mutation and nuclear exclusion. Proc Natl Acad Sci USA 1992; 89: 7262–7266.
Prost S, Le MG, Douc-Rasy S et al. Association of c-erbB2-gene amplification with poor prognosis in non-inflammatory breast carcinomas but not in carcinomas of the inflammatory type. Int J Cancer 1994; 58: 763–768.
Tagliabue E, Pilotti S, Gianni AM et al. Target molecules for immunotherapy of inflammatory breast carcinomas. Eur J Cancer 1998; 34: 1982–1983.
Vincent-Salomon A, Carton M, Freneaux P et al. ERBB2 overexpression in breast carcinomas: no positive correlation with complete pathological response to preoperative high-dose anthracycline-based chemotherapy. Eur J Cancer 2000; 36: 586–591.
Turpin E, Bieche I, Bertheau P et al. Increased incidence of ERBB2 overexpression and TP53 mutation in inflammatory breast cancer. Oncogene 2002; 21: 7593–7597.
MacGrogan G, Bonichon F, de Mascarel I et al. Prognostic value of p53 in breast invasive ductal carcinoma: an immunohistochemical study on 942 cases. Breast Cancer Res Treat 1995; 36: 71–81.
Ozbun MA, Butel JS . Tumor suppressor p53 mutations and breast cancer: a critical analysis. Adv Cancer Res 1995; 66: 71–141.
Faille A, De Cremoux P, Extra JM et al. p53 mutations and overexpression in locally advanced breast cancers. Br J Cancer 1994; 69: 1145–1150.
Cooke T, Reeves J, Lanigan A et al. HER2 as a prognostic and predictive marker for breast cancer. Ann Oncol 2001; 12: S23–S28.
Frei III E, Canellos GP . Dose: a critical factor in cancer chemotherapy. Am J Med 1980; 69: 585–594.
Rouesse J, Friedman S, Sarrazin D et al. Primary chemotherapy in the treatment of inflammatory breast carcinoma: a study of 230 cases from the Institut Gustave-Roussy. J Clin Oncol 1986; 4: 1765–1771.
Viens P, Penault-Llorca F, Jacquemier J et al. High-dose chemotherapy and haematopoietic stem cell transplantation for inflammatory breast cancer: pathologic response and outcome. Bone Marrow Transplant 1998; 21: 249–254.
Feldman LD, Hortobagyi GN, Buzdar AU et al. Pathological assessment of response to induction chemotherapy in breast cancer. Cancer Res 1986; 46: 2578–2581.
Noguchi S, Miyauchi K, Nishizawa Y et al. Management of inflammatory carcinoma of the breast with combined modality therapy including intraarterial infusion chemotherapy as an induction therapy. Long-term follow-up results of 28 patients. Cancer 1988; 61: 1483–1491.
Armstrong DK, Fetting JH, Davidson NE et al. Sixteen week dose intense chemotherapy for inoperable, locally advanced breast cancer. Breast Cancer Res Treat 1993; 28: 277–284.
Chevallier B, Roche H, Olivier JP et al. Inflammatory breast cancer. Pilot study of intensive induction chemotherapy (FEC-HD) results in a high histologic response rate. Am J Clin Oncol 1993; 16: 223–228.
Ayash LJ, Elias A, Ibrahim J et al. High-dose multimodality therapy with autologous stem-cell support for stage IIIB breast carcinoma. J Clin Oncol 1998; 16: 1000–1007.
Schwartzberg L, Weaver C, Lewkow L et al. High-dose chemotherapy with peripheral blood stem cell support for stage IIIB inflammatory carcinoma of the breast. Bone Marrow Transplant 1999; 24: 981–987.
Chevallier B, Asselain B, Kunlin A et al. Inflammatory breast cancer. Determination of prognostic factors by univariate and multivariate analysis. Cancer 1987; 60: 897–902.
Sataloff DM, Mason BA, Prestipino AJ et al. Pathologic response to induction chemotherapy in locally advanced carcinoma of the breast: a determinant of outcome. J Am Coll Surg 1995; 180: 297–306.
Delarue JC, May-Levin F, Mouriesse H et al. Oestrogen and progesterone cytosolic receptors in clinically inflammatory tumours of the human breast. Br J Cancer 1981; 44: 911–916.
Paradiso A, Tommasi S, Brandi M et al. Cell kinetics and hormonal receptor status in inflammatory breast carcinoma. Comparison with locally advanced disease. Cancer 1989; 64: 1922–1927.
De Boer RH, Allum WH, Ebbs SR et al. Multimodality therapy in inflammatory breast cancer: is there a place for surgery? Ann Oncol 2000; 11: 1147–1153.
Antman KH, Rowlings PA, Vaughan WP et al. High-dose chemotherapy with autologous hematopoietic stem-cell support for breast cancer in North America. J Clin Oncol 1997; 15: 1870–1879.
Somlo G, Doroshow JH, Forman SJ et al. High-dose chemotherapy and stem-cell rescue in the treatment of high-risk breast cancer: prognostic indicators of progression-free and overall survival. J Clin Oncol 1997; 15: 2882–2893.
Cagnoni PJ, Nieto Y, Shpall EJ et al. High-dose chemotherapy with autologous hematopoietic progenitor-cell support as part of combined modality therapy in patients with inflammatory breast cancer. J Clin Oncol 1998; 16: 1661–1668.
Adkins D, Brown R, Trinkaus K et al. Outcomes of high-dose chemotherapy and autologous stem-cell transplantation in stage IIIB inflammatory breast cancer. J Clin Oncol 1999; 17: 2006–2014.
Arun B, Slack R, Gehan E et al. Survival after autologous hematopoietic stem cell transplantation for patients with inflammatory breast carcinoma. Cancer 1999; 85: 93–99.
Fields JN, Kuske RR, Perez CA et al. Prognostic factors in inflammatory breast cancer. Univariate and multivariate analysis. Cancer 1989; 63: 1225–1232.
Chevallier B, Bastit P, Graic Y et al. The Centre H. Becquerel studies in inflammatory non metastatic breast cancer. Combined modality approach in 178 patients. Br J Cancer 1993; 67: 594–601.
Cristofanilli M, Buzdar AU, Hortobagyi GN . Update on the management of inflammatory breast cancer. Oncologist 2003; 8: 141–148.
Gradishar WJ . Primary (neoadjuvant) chemotherapy with docetaxel in breast cancer. Clin Breast Cancer 2001; 2 (Suppl 1): S31–S35.
Acknowledgements
This work was supported in part by the Association pour la Recherche sur le Cancer (ARC Printemps 2002, Grant No. 4719).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bertucci, F., Tarpin, C., Charafe-Jauffret, E. et al. Multivariate analysis of survival in inflammatory breast cancer: impact of intensity of chemotherapy in multimodality treatment. Bone Marrow Transplant 33, 913–920 (2004). https://doi.org/10.1038/sj.bmt.1704458
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704458
Keywords
This article is cited by
-
Photodynamic therapy as an effective therapeutic approach in MAME models of inflammatory breast cancer
Breast Cancer Research and Treatment (2015)
-
Are there candidates for high-dose chemotherapy in ovarian carcinoma?
Journal of Experimental & Clinical Cancer Research (2012)
-
Overview of preoperative radiochemotherapy in breast cancer: past or future?
Clinical and Translational Oncology (2011)
-
Update on inflammatory breast cancer
Breast Cancer Research (2005)
-
Short- and long-term cause-specific survival of patients with inflammatory breast cancer
BMC Cancer (2005)