Summary:
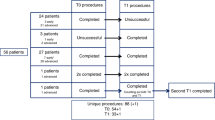
The purpose of this study was to evaluate the presence of micrometastatic cells in the apheresis products from patients with breast cancer, and also to determine if repeated infusion of contaminated products had any clinical impact. A total of 94 patients with high-risk breast cancer were enrolled in a prospective single center study to evaluate the use of dose-intensified chemotherapy (doxorubicine 75 mg/m2 and cyclophosphamide 3000 or 6000 mg/m2 for four cycles) with repeated (× 2) stem cell reinfusion. All women were monitored for the presence of metastatic cells in aphereses, collected after first course of intensive chemotherapy, and following additional mobilization with rhG-CSF. Epithelial cells were screened with monoclonal antibodies directed to cytokeratin. Eight of the 94 patients had detectable tumor cells in one or several aphereses collected after intensive chemotherapy; this was unrelated to other tumor characteristics, including size, histology, Scarff Bloom and Richardson (SBR) grading (presence or absence of hormone receptors). Hemato-poietic reconstitution was similar in the cells from these eight patients, and in the total patient population. Three of these eight patients relapsed. This study has confirmed that contamination of apheresis products remains a rare event, which does not seem to affect clinical evolution, even when reinfused into the patient.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Peters WP, Shpall EJ, Jones RB et al. High-dose combination alkylating agents with bone marrow support as initial treatment for metastatic breast cancer. J Clin Oncol 1988; 6: 1368–1376.
Antman K, Ayash L, Elias A et al. A phase II study of high-dose cyclophosphamide, thiotepa, and carboplatin with autologous marrow support in women with measurable advanced breast cancer responding to standard-dose therapy. J Clin Oncol 1992; 10: 102–110.
Basser RL, To LB, Begley CG et al. Adjuvant treatment of high-risk breast cancer using multicycle high-dose chemo-therapy and filgrastim-mobilized peripheral blood progenitor cells. Clin Cancer Res 1995; 1: 715–721.
Braun S, Pantel K, Müller P et al. Cytokeratin-positive cells in the bone marrow and survival of patients with stage I, II, or III breast cancer. N Engl J Med 2000; 342: 525–533.
Franklin WA, Glaspy J, Pflaumer SM et al. Incidence of tumor-cell contamination in leukapheresis products of breast cancer patients mobilized with stem cell factor and granulocyte colony-stimulating factor (G-CSF) or with G-CSF alone. Blood 1999; 94: 340–347.
Simpson SJ, Vachula M, Kennedy MJ et al. Detection of tumors cells in the bone marrow, peripheral blood, and apheresis products of breast cancer patients using flow cytometry. Exp Hematol 1995; 23: 1062–1068.
Mapara M, Körner IJ, Hildebrandt M et al. Monitoring of tumor cell purging after highly efficient immunomagnetic selection of CD34 cells from leukapheresis products in breast cancer patients: comparison of immunocytochemical tumor cell staining and reverse transcriptase-polymerase chain reaction. Blood 1997; 89: 337–344.
Ghossein R, Bhattacharya S, Rosai J . Molecular detection of micrometastases and circulating tumor cells in solid tumors. Clin Cancer Res 1999; 5: 1950–1960.
Diel I, Kaufmann M, Costa S et al. Micrometastatic breast cancer cells in bone marrow at primary surgery: prognostic value in comparaison with nodal status. J Natl Cancer Inst 1996; 88: 1652–1658.
Cote RJ, Rosen PP, Lesser ML et al. Prediction of early relapse in patient with operable breast cancer by detection of occult bone marrow micrometastases. J Clin Oncol 1991; 9: 1749–1756.
Mansi JL, Gogas H, Bliss JM et al. Outcome of primary-breast-cancer patients with micrometastases: a long-term follow-up study. Lancet 1999; 354.
Brugger W, Bross KJ, Glatt MG et al. Mobilization of tumor cells and hematopoietic progenitor cells into peripheral blood of patients with solid tumors. Blood 1994; 83: 636–640.
Brenner MK, Rill DR, Moen RC et al. Gene-marking to trace origin of relapse after autologous bone marrow transplantation. Lancet 1993; 341: 85–86.
Deisseroth AB, Zu Z, Claxton D et al. Genetic marking shows that Ph+ cells present in autologous transplants of chronic myelogenous leukemia (CML) contribute to relapse after autologous bone marrow in CML. Blood 1994; 83: 3068–3076.
Cooper BW, Moss TJ, Ross AA et al. Occult tumor contamination of hematopoietic stem-cell products does not affect outcome of autologus transplantation in patients with metastatic breast cancer. J Clin Oncol 1998; 16: 3509–3517.
Stadtmauer EA, Tsai DE, Sickles CJ et al. Stem cell transplantation for metastatic breast cancer: analysis of tumor contamination. Med Oncol 1999; 16: 279–288.
Shpall EJ, LeMaistre CF, Holland K et al. A prospective randomized trial of buffy coat vs CD34-selected autologous bone marrow support in high-risk breast cancer patients receiving high-dose chemotherapy. Blood 1997; 90: 4313–4320.
Chabannon C, Cornetta K, Lotz JP et al. High-dose chemo-therapy followed by reinfusion of selected CD34+ peripheral blood cells in patients with poor-prognosis breast cancer: a randomized multicentre study. Br J Cancer 1998; 78: 913–921.
Stewart AK, Vescio R, Schiller G et al. Purging of autologous peripheral-blood stem cells using CD34 selection does not improve overall or progression-free survival after high-dose chemotherapy for multiple myeloma: results of a multicenter randomized controlled trial. J Clin Oncol 2001; 19: 3771–3779.
Yanovich S, Mitsky P, Cornetta K et al. Transplantation of CD34+ peripheral blood cells selected using a fully automated immunomagnetic system in patients with high-risk breast cancer: results of a prospective randomized multicenter clinical trial. Bone Marrow Transplant 2000; 25: 1165–1174.
Kruger WH, Kroger N, Togel F et al. Disseminated breast cancer cells prior to and after high-dose therapy. J Hematother Stem Cell Res 2001; 10: 681–689.
Chabannon C, Le Coroller AG, Faucher C et al. Patient condition affects the collection of peripheral blood progenitors after priming with recombinant granulocyte colony-stimulating factor. J Hematother 1995; 4: 171–179.
Mozziconacci MJ, Arnoulet C, Novakovitch G et al. Contamination des cytaphérèses par des cellules tumorales: à propos de 39 cas de cancer du sein. Bull Cancer 1996; 83: 649–653.
Pantel K, Cote RJ, Fodstad O . Detection and clinical importance of micrometastatic disease. J Natl Cancer Inst 1999; 91: 1113–1124.
Braun S, Cevatli BS, Assemi C et al. Comparative analysis of micrometastasis to the bone marrow and lymph nodes of node-negative breast cancer patients receiving no adjuvant therapy. J Clin Oncol 2001; 19: 1468–1475.
Gebauer G, Fehm T, Merkle E et al. Epithelial cells in bone marrow of breast cancer patients at time of primary surgery: clinical outcome during long-term follow-up. J Clin Oncol 2001; 19: 3669–3674.
Braun S, Pantel K . Micrometastatic bone marrow involvement detection and prognosis significance. Med Oncol 1999; 16.
Osborne MP, Shuirin A, Wong GY et al. Immunofluorescent monoclonal antibody detection of breast cancer in bone marrow: sensitivity in a model system. Cancer Res 1989; 49: 2510–2513.
Pantel K, Schlimok G, Angstwurm M et al. Methodological analysis of immunocytochemical screening for disseminated epithelial tumor cells in bone marrow. J Hemathother 1994; 3: 165–173.
Chaiwun B, Saad AD, Groshen S et al. Immunohistochemical detection of occult carcinoma in bone marrow and blood. Diagn Oncol 1992; 2: 267–276.
Fetsch PA, Cowan KH, Weng DE et al. Detection of circulating tumor cells and micrometastases in stage II, III, and IV breast cancer patients utilizing cytology and immunocytochemistry. Diagn Cytopathol 2000; 22: 323–328.
Weaver CH, Moss T, Schwartzberg LS et al. High-dose chemotherapy in patients with breast cancer: evaluation of infusing peripheral blood stem cells containing occult tumor cells. Bone Marrow Transplant 1998; 21: 1117–1124.
Vredenburgh JJ, Peters WP, Rosner G et al. Detection of tumor cells in the bone marrow of stage IV breast cancer patients receiving high-dose chemotherapy: the role of induction chemotherapy. Bone Marrow Transplant 1995; 16: 815–821.
Braun S, Kentenich C, Janni W et al. Lack of effect of adjuvant chemotherapy on the elimination of single dormant tumor cells in bone marrow of high-risk breast cancer patients. J Clin Oncol 2000; 18: 80–86.
Shpall EJ, Jones RB . Release of tumor cells from bone marrow. Blood 1994; 83: 623–625.
Fox SB, Leek RD, Bliss J et al. Association of tumor angiogenesis with bone marrow micrometastases in breast cancer patients. J Natl Cancer Inst 1997; 89: 1044–1049.
Brandt B, Roetger A, Heidl S et al. Isolation of blood-borne epithelium-derived c-erbB-2 oncoprotein-positive clustered cells from the peripheral blood of breast cancer patients. Int J Cancer 1998; 76: 824–828.
Schlimok G, Funke I, Bock B et al. Epithelial tumor cells in bone marrow of patients with colorectal cancer: immunocytochemical detection, phenotypic characterization, and prognostic significance. J Clin Oncol 1990; 8: 831–837.
Pantel K, Schlimok G, Kutter D et al. Frequent down-regulation of major histocompatibility class I antigen expression on individual micrometastatic carcinoma cells. Cancer Res 1991; 51: 4712–4715.
Pantel K, Schlimok G, Braun S et al. Differential expression of proliferation-associated molecules in individual micrometastatic carcinoma cells. J Natl Cancer Inst 1991; 85: 1419–1424.
Acknowledgements
This work was supported by special grants from the ‘Association pour la Recherche sur le cancer’.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Viret, F., Chabannon, C., Sainty, D. et al. Occult tumor cell contamination in patients with stage II/III breast cancer receiving sequential high-dose chemotherapy. Bone Marrow Transplant 32, 1059–1064 (2003). https://doi.org/10.1038/sj.bmt.1704283
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1704283