Summary:
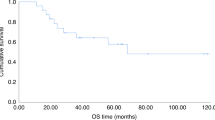
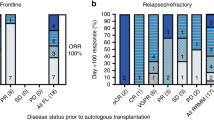
This study was conducted to evaluate the efficacy of high-dose thiotepa, melphalan and carboplatin (TMCb) regimen in 27 patients undergoing autologous stem cell transplantation (ASCT) for metastatic breast cancer. A total of 27 patients with stage IV breast cancer underwent ASCT following thiotepa (500 mg/m2), melphalan (100 mg/m2) and carboplatin (1200–1350 mg/m2). Of 27 patients, 17 had refractory relapse, eight had responding relapse, and two had no evidence of disease (NED) at the time of transplant. In all, 11 patients had only bone disease, nine had bone plus visceral disease, three had only visceral disease, and two had locoregional recurrent disease. The median time from diagnosis to transplant was 1081 days (range 180–2341). Staging for evaluation of response was performed 4–6 months after transplantation. Five patients were not evaluable (NE) for response because of NED at transplant (n=2) or early death due to transplant-related complications (n=3) (two of viral pneumonia and one of regimen-related toxicity) occurring at a median of 4 days (range 11–46) post-transplant. One of the two patients who was NED at the time of transplant is still NED on day 760 post-transplant. Seven of 15 refractory (47%) and 5/7 (71%) responsive patients with evaluable disease achieved a complete response of all measurable disease or all soft-tissue disease with at least improvement in bone lesions. Of 27 patients (37%),10 are alive and progression-free, a median of 582 days (range 410–1380) after treatment, 6/17 (35%) with refractory disease and 4/10 (40%) with responsive disease. The probability of progression-free survival (PFS) for all patients was 0.50. The probabilities of PFS at 2 years for patients with refractory (n=17) and responsive (n=10) disease were 0.42 and 0.60, respectively. PFS at 2 years for the 14 patients who were NED or achieved CR/PR* following-HDC was 0.67. PFS at 2 years for patients who did not achieve CR/PR* following-DHC was 0.33. These preliminary data suggest that high-dose TMCb followed by autologous stem cell transplantation is an effective regimen for patients with advanced breast cancer and may be comparable to some previously used regimens.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Sarosy G, Leyland-Jones B, Soochan P et al. The systemic administration of intravenous melphalan. J Clin Oncol 1988; 6: 1768–1782.
Wright JC, Golomb FM, Gumport SL et al. Summary of results with triethylenethiophosphoramide. Ann NY Acad Sci 1958; 68: 937–966.
Lemaistre CF, Herqıg GP, Herqıg RH et al. High-dose thiotepa and autologous bone marrow rescue for the treatment of breast cancer. Breast Cancer Res Treat 1987; 10: 89.
Maranichi D, Pıana L, Blaise D et al. Phase I–II studies of high-dose alkylating agents in poor risk patients with breast cancer with autologous bone marrow transplant. In: ABMT: Proceedings of the Third International Symposium. Dicke K, Spitzer TR, Jagannath S (eds). University of Texas MD Anderson Hospital: Houston, TX, 1987; 475–480.
Corringham R, Gılmore M, Prentice H et al. High-dose melphalan with autologous bone marrow transplant: treatment of poor prognosis tumors. Cancer 1983; 52: 1783–1787.
Weaver CH, Bensinger WI, Appelbaum FR et al. Phase I study of high-dose busulfan, melphalan, and thiotepa with autologous stem cell support in patients with refractory malignancies. Bone Marrow Transplant 1994; 14: 813–819.
Schiffman K, Bensinger W, Appelbaum F et al. Phase-II of high-dose busulfan, melphalan and thiotepa with autologous peripheral blood stem cell support in patients with malignant disease. Bone Marrow Transplant 1996; 17: 943–950.
Bensinger W, Schiffman K, Holmberg L et al. High-dose busulfan, melphalan, thiotepa and peripheral blood stem cell infusion for the treatment of metastatic breast cancer. Bone Marrow Transplant 1997; 19: 1183–1189.
Eder JP, Elıas A, Shea TC et al. A phase I–II study of cyclophosphamide, thiotepa, and carboplatin with autologous bone marrow transplantation in solid tumor patients. J Clin Oncol 1990; 8: 1239–1245.
Shea TC, Flaherty M, Elias A et al. A phase I clinical and pharmacokinetic study of carboplatin and autologous bone marrow support. J Clin Oncol 1989; 7: 651–655.
Antman K, Ayash L, Elias A et al. A phase II study of high-dose cyclophosphamide, thiotepa, and carboplatin with autologous marrow support in women with measurable advanced breast cancer responding to standard-dose therapy. J Clin Oncol 1992; 10: 102–110.
Holland K, Dix SP, Geller RB et al. Minimal toxicity and mortality in high-risk breast cancer patients receiving high-dose cyclophosphamide, thiotepa, and carboplatin plus autologous marrow/stem-cell transplantation and comprehensive supportive care. J Clin Oncol 1996; 14: 1156–1164.
Ayash L, Elias A, Ibrahim J et al. High-dose multimodality therapy with autologous stem-cell support for stage IIIB breast carcinoma. J Clin Oncol 1998; 16: 1000–1007.
Demirer T, Ilhan O, Mandel NM et al. A phase I dose escalation study of high-dose thiotepa, melphalan and carboplatin (TMCb) followed by autologous peripheral blood stem cell transplantation (PBSCT) in patients with solid tumors and hematologic malignancies. Bone Marrow Transplant 2000; 25: 697–703.
Demirer T, Buckner CD, Bensinger WI et al. Peripheral blood stem cell (PBSC) collections after taxol, cyclophosphamide and recombinant human granulocyte-colony-stimulating factor (rhG-CSF). J Clin Oncol 1995; 13: 1714–1719.
Demirer T, Buckner CD, Storer B et al. Effect of different chemotherapy regimens on peripheral-blood stem-cell collections in patients with breast cancer receiving granulocyte-colony stimulating factor. J Clin Oncol 1997; 15: 684–690.
Weaver CH, Schwartzberg LS, Birch R et al. Collection of peripheral blood progenitor cells following the administration of cyclophosphamide, etoposide and granulocyte-colony stimulating factor: an analysis of 497 patients. Transfusion 1997; 37: 896–903.
Rowley SD, Bensinger WI, Gooley T et al. Effect of cell concentration on bone marrow and peripheral blood stem cell cryopreservation. Blood 1994; 83: 2731–2736.
Bearman SI, Appelbaum FR, Buckner CD et al. Regimen related toxicity in patients undergoing bone marrow transplantation. J Clin Oncol 1988; 6: 1562–1568.
Ayash LJ, Wheeler C, Fairclough D et al. Prognostic factors for prolonged progression-free survival with high-dose chemotherapy with autologous stem-cell support for advanced breast cancer. J Clin Oncol 1995; 13: 2043–2049.
Kaplan EL, Meier P . Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958; 53: 457–481.
Hyrniuk WM . Relative dose intensity and the impact on design of clinical trials. Semin Oncol 1987; 14: 65–74.
Broder LE, Tormey DC . Combination chemotherapy of carcinoma of the breast cancer. Cancer Treat Rev 1974; 1: 183–203.
Antman K, Rowlings PA, Vaughan WP et al. High-dose chemotherapy with autologous hematopoietic stem-cell support for breast cancer in North America. J Clin Oncol 1997; 15: 1870–1879.
Demirer T, Buckner CD, Appelbaum FR et al. High-dose busulfan, and cyclophosphamide followed by autologous transplantation in patients with advanced breast cancer. Bone Marrow Transplant 1996; 17: 769–774.
Peters WP, Shpall EJ, Jones RB et al. High-dose combination alkylating agents with bone marrow support as initial treatment for metastatic breast cancer. J Clin Oncol 1988; 6: 1368–1376.
Williams SF, Mick R, Desser R et al. High-dose consolidation therapy with autologous stem cell rescue in stage IV breast cancer. J Clin Oncol 1989; 7: 1824–1830.
Klumpp TR, Mangan KF, Glenn LD et al. Phase II pilot study of high-dose busulfan and CY followed by autologous BM of peripheral blood stem cell transplantation in patients with advanced chemosensitive breast cancer. Bone Marrow Transplant 1993; 11: 337–339.
Eder JP, Antman K, Peters W et al. High-dose combination alkylating agent chemotherapy with autologous bone marrow support for metastatic breast cancer. J Clin Oncol 1986; 4: 1592–1597.
Dunphy FR, Spitzer G, Buzdar A et al. Treatment of estrogen receptor negative or hormonally refractory breast cancer with double high-dose chemotherapy intensification and bone marrow support. J Clin Oncol 1990; 8: 1207–1216.
Williams SF, Gilewski T, Mick R et al. High-dose consolidation therapy with autologous stem cell rescue in stage IV breast cancer: follow-up report. J Clin Oncol 1992; 10: 1743–1747.
Ayash LJ, Wheeler C, Reich E et al. Double dose-intensive chemotherapy with autologous marrow and peripheral blood progenitor-cell support for metastatic breast cancer: a feasibility study. J Clin Oncol 1994; 12: 37–44.
Vaughan WP, Reed EC, Kessinger A et al. High-dose cyclophosphamide, thiotepa and hydroxyurea with autologous hematopoietic stem cell rescue: an effective consolidation chemotherapy regimen for early metastatic breast cancer. Bone Marrow Transplant 1994; 13: 619–624.
Gutierrez-Delgado F, Holmberg LA, Hooper H et al. High-dose busulfan, melphalan and thiotepa as consolidation for non-inflammatory high-risk breast cancer. Bone Marrow Transplant 2000; 26: 51–59.
Antman K, Gale RP . Advanced breast cancer: high-dose chemotherapy and bone marrow autotransplants. Ann Intern Med 1988; 108: 570–574.
Berry DA, Broadwater G, Klein JP et al. High-dose versus standard dose chemotherapy in metastatic breast cancer: comparison of Cancer and Leukemia Group B trials with data from the Autologous Blood and Marrow Transplant Registry. J Clin Oncol 2002; 20: 743–750.
Lotz JP, Cure H, Janvier M et al. High dose chemotherapy with hematopoietic stem cell transplantation for metastatic breast cancer: results of the French protocol PEGASE 04. Proc Am Soc Clin Oncol 1999; 18: 43a.
Stadtmauer EA, O'Neill A, Goldstein LJ et al. Conventional-dose chemotherapy compared with high-dose chemotherapy plus autologous hematopoietic stem cell transplantation for metastatic breast cancer. N Engl J Med 2000; 342: 1069–1076.
Madan B, Broadwater G, Rubin P et al. Improved survival with consolidation high-dose CBP compared with observation followed by transplant at relapse in women with metastatic breast cancer and only bone metastases treated with induction AFM: a phase III prospective randomized comparative trial. Proc Am Soc Clin Oncol 2000; 19: 48a(184).
Peters WP, Jones RB, Vredenburgh J et al. A large, prospective, randomized trial of high-dose combination alkylating agent (CBP) with autologous cellular support as consolidation for patients with metastatic breast cancer achieving complete remission after intensive doxorubicin-based induction therapy (AFM). Proc Am Soc Clin Oncol 1996; 15: 149a.
Crump M, Gluck S, Stewart D et al. Randomized trial of high-dose chemotherapy with autologous peripheral blood stem cell support compared to standard therapy in women with metastatic breast cancer: a National Cancer Institute of Canada (NCIC) Clinical Trials Group Study. Proc Am Soc Clin Oncol 2001; 20: 21a.
Weaver CH, West WH, Schwartzberg LS et al. Induction, mobilization of peripheral blood stem cells (PBSC), high-dose chemotherapy and PBSC infusion in patients with untreated stage IV breast cancer: outcomes by intent to treat analyses. Bone Marrow Transplant 1997; 19: 661–670.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Demirer, T., Uysal, V., Aylı, M. et al. High-dose thiotepa, melphalan and carboplatin (TMCb) followed by autologous stem cell transplantation in patients with advanced breast cancer: a retrospective evaluation. Bone Marrow Transplant 31, 755–761 (2003). https://doi.org/10.1038/sj.bmt.1703918
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bmt.1703918
Keywords
This article is cited by
-
The novel alkylating prodrug J1: diagnosis directed activity profile ex vivo and combination analyses in vitro
Investigational New Drugs (2008)
-
High-dose thiotepa, melphalan and carboplatin (TMCb) followed by autologous peripheral blood stem cell transplantation in patients with lymphoma – a retrospective evaluation
Bone Marrow Transplantation (2004)