Abstract
Drugs that increase dopamine levels in the brain can cause psychotic symptoms in healthy individuals and worsen them in schizophrenic patients. Psychological stress also increases dopamine release and is thought to play a role in susceptibility to psychotic illness. We hypothesized that healthy individuals at elevated risk of developing psychosis would show greater striatal dopamine release than controls in response to stress. Using positron emission tomography and [11C]raclopride, we measured changes in synaptic dopamine concentrations in 10 controls and 16 psychometric schizotypes; 9 with perceptual aberrations (PerAb, ie positive schizotypy) and 7 with physical anhedonia (PhysAn, ie negative schizotypy). [11C]Raclopride binding potential was measured during a psychological stress task and a sensory-motor control. All three groups showed significant increases in self-reported stress and cortisol levels between the stress and control conditions. However, only the PhysAn group showed significant stress-induced dopamine release. Dopamine release in the entire sample was significantly negatively correlated with smooth pursuit gain, an endophenotype linked to frontal lobe function. Our findings suggest the presence of abnormalities in the dopamine response to stress in negative symptom schizotypy, and provide indirect evidence of a link to frontal function.
Similar content being viewed by others
INTRODUCTION
Stressful stimuli lead to dopamine (DA) release in the brains of animals (Abercrombie et al, 1989; Rouge-Pont et al, 1993) and humans (Adler et al, 2000; Pruessner et al, 2004). Considerable evidence links psychotic states and a hyperdopaminergic response to physiological or psychological stressors (Moore et al, 1999). In schizophrenia, a prototypical psychotic illness, there is clinical evidence of abnormal DA response to pharmacological challenge, metabolic stressor, and psychological stressor. For example, schizophrenic patients have a higher DA response to amphetamine than controls as measured by receptor binding studies (Laruelle et al, 1996; Breier et al, 1997), and do not show the expected decrease in plasma homovanillic acid (HVA, a DA metabolite) in response to a mental stressor (Sumiyoshi et al, 1999). Schizotypal personality disorder patients also show greater amphetamine-induced DA release than controls, though less than that seen in acute schizophrenic patients (Abi-Dargham et al, 2004). A metabolic stressor, 2-deoxy-glucose, induced significantly larger increases in plasma HVA in schizophrenic patients than controls (Elman et al, 2003). Interestingly, the same stressor produced HVA elevation in schizotypal personality disorder patients only equivalent to controls, along with a blunted cortisol response, possibly indicating that these patients possess a buffering mechanism against hypothalamic–pituitary–adrenal axis stress activation (Mitropoulou et al, 2004). Stress, like DA agonist drugs, can trigger relapse in schizophrenic patients (Norman and Malla, 1993; Nuechterlein et al, 1994). It has been proposed that exaggerated responses to stress are key in the etiology of psychosis in vulnerable individuals (Thompson et al, 2004). However, it is not clear whether differences in dopaminergic responsiveness precede psychosis or develop subsequent to onset.
In the current study, we compared acute stress-related DA release in healthy individuals at elevated risk for psychosis and demographically similar normal controls. High-risk subjects were two groups of ‘psychometric schizotypes’ with elevated scores on either positive or negative symptom dimensions. Recent research on schizotypy indicates that schizotypal symptoms divide into the same three factors found in schizophrenia, ie positive, negative, and disorganized (Reynolds et al, 2000; Suhr and Spitznagel, 2001). Here, we chose to focus on the positive and negative dimensions of schizotypy, since these have been associated in longitudinal studies with elevated rates of psychosis and social dysfunction (Erlenmeyer-Kimling et al, 1993; Chapman et al, 1994; Kwapil et al, 1997; Freedman et al, 1998). We identified positive and negative symptom schizotypy using the perceptual aberration (PerAb) and physical anhedonia (PhysAn) scales, respectively (Chapman et al, 1976, 1978). These scales have a low intercorrelation, suggesting the two groups represent divergent aspects of vulnerability to psychosis (Chapman et al, 1980).
We performed [11C]raclopride positron emission tomography (PET) while exposing subjects to a psychological stressor previously shown to induce significant striatal DA release in healthy volunteers with poor maternal care (Pruessner et al, 2004). Because of these previous findings, we also assessed maternal care using the Parental Bonding Inventory (Parker et al, 1979). We hypothesized that schizotypal individuals would show greater striatal DA responses than control subjects. Finally, because theoretical models have linked DA release with frontal lobe dysfunction in schizophrenia (Davis et al, 1991), smooth pursuit eye movements were measured as an index of frontal lobe function (O'Driscoll et al, 1999; Bagary et al, 2004).
MATERIALS AND METHODS
Subjects
The individuals who participated in the current study are a subgroup of participants recruited for a larger study (Holahan and O'Driscoll, 2005). Students in 10 of the largest undergraduate classes at McGill University completed a 300-item questionnaire on ‘perceptions and experiences’ consisting of 35 items from the PerAb Scale (Chapman et al, 1978), 61 items from the PhysAn Scale (Chapman et al, 1976), and 204 distracter items from the Minnesota Multiphasic Personality Inventory-2 (MMPI-2) (Hathaway and McKinley, 1989). Elevated scores on the MMPI Social Desirability Scale (scores >2 SD above the control mean) were used to exclude subjects with a test-taking style that could invalidate results. A total of 1914 questionnaires were completed for a 60% return rate. Potential schizotypal subjects were individuals who scored >1.95 SD above the mean of their sex on only one of the two schizotypy scales while potential control subjects scored 0.5 SD below the mean on both scales. Cutoffs used were similar to those reported in previous college samples (O'Driscoll et al, 1998; Gooding et al, 2000). Subjects were screened for Axis I diagnoses using the computerized Diagnostic Interview Schedule Screening Instrument (Robins et al, 1981). When this yielded Axis I diagnoses, subjects were interviewed by one investigator (AVH) using the Structured Clinical Interview for DSM-IV (First et al, 1996) and excluded if they met criteria. Additional exclusion criteria included any neurological condition, use of prescription medication other than oral contraceptives, pregnancy, claustrophobia, metal in the body, or radiological procedures in the past year.
The Chapman questionnaires identify subjects based on their reported experience of different classes of subclinical symptoms hypothesized to be related to schizophrenia. Individuals with elevated scores on the PerAb scale have an elevated risk of psychosis (Chapman et al, 1980, 1994), an elevated rate of schizophrenia in first-degree relatives (Lenzenweger and Loranger, 1989) and a myriad of cognitive and psychophysiological deficits that are associated with schizophrenia (Simons, 1982; Allen et al, 1987; Jutai, 1989; Lenzenweger, 1991; Simons and Giardina, 1992; Kwapil et al, 1996; Suhr, 1997; Nuchpongsai et al, 1999; Gooding et al, 2001). Elevated PhysAn scores in the adolescent offspring of schizophrenic patients are associated with increased rates of psychosis and poorer social adjustment in young adulthood (Erlenmeyer-Kimling et al, 1993; Freedman et al, 1998). Healthy individuals with elevated scores on the PhysAn scale also show many attributes of a high-risk population: they have an increased incidence of the cognitive, behavioral, and social abnormalities associated with schizophrenia, including impaired attention (Jutai, 1989; Wilkins and Venables, 1992; Erlenmeyer-Kimling et al, 1993), reaction time crossover (Simons, 1982), abnormal P300 amplitude (Miller, 1986), skin conductance nonresponsiveness (Dawson and Nuechterlein, 1984), and poorer social competence (Garnet et al, 1993; Blanchard et al, 1998). Further, PhysAn scores may have a familial component as they are higher in schizophrenic patients and their relatives than controls (Katsanis et al, 1990; Clementz et al, 1991; Franke et al, 1993), and are higher in individuals with schizophrenia-related personality disorders who have a genetic loading of schizophrenia than in those without it (Thaker, 2000).
Twenty-eight healthy volunteers participated in the imaging study: 10 controls, 10 PerAb, and 8 PhysAn subjects. The three groups were demographically similar (Table 1). The experiments were approved by the Research Ethics Committee of the Montreal Neurological Institute and Hospital. After complete description of the study to the subjects, written informed consent was obtained. Subjects were compensated for their participation.
Stress Task
Psychological stress was induced using a mental arithmetic task similar to that used in a previous PET study (Pruessner et al, 2004). The task consists of arithmetic problems that have to be answered under time pressure. Subjects were trained outside the scanner prior to the first PET session. For the stress PET condition, the time constraint was set slightly below the average time needed during the pre-scan session. During the scan, the time constraint was adjusted for each 3-min segment based on performance in the previous segment, to maintain constant difficulty. This ensures that all subjects perform the same number of problems with the same success rate. Arithmetic questions were presented in the scanner via a computer screen and answered using a computer mouse. The same computer screen also displayed information about the total number of errors, the expected average number of errors, the time spent on the current problem, and the performance feedback for each problem (correct, incorrect, timeout). There were three blocks of 12 min each (in four 3-min segments) of mental arithmetic. A confederate, blinded to each individual's group membership, wearing a lab coat and standing beside the scanner, gave the subject negative feedback after each 3-min segment. Feedback included a report of the subject's inferior standing with regard to ‘expected’ performance and a recommendation to improve their score. This task has been shown to induce behavioral and physiological stress and anxiety responses (Pruessner et al, 1999) and DA release in the ventral striatum as measured by [11C]raclopride PET (Pruessner et al, 2004). After the end of the testing session, subjects were debriefed and told that the task was designed to be impossible to accomplish and that it did not assess their ability to perform mental arithmetic. During the nonstress control PET session, subjects performed a similar arithmetic task, but without time constraints, visible progress bar, or negative verbal feedback.
PET Procedure
Each subject underwent two [11C]raclopride PET scans, one during the stress task, and one during the control task, conducted on different days with the order counterbalanced across subjects and groups. For the stress scanning session, subjects performed the mental arithmetic task continuously from approximately 10 min before until 20 min after the [11C]raclopride injection, except for the verbal feedback blocks in between each 3-min arithmetic task block. The control session was identical except that there was no contact with the confederate and no time limit. The two scans were done at the same time of day, within four weeks of each other. The groups did not differ in inter-scan interval. PET scans were obtained with a CTI/Siemens HR+ tomograph. Ten minutes after beginning the stress or control task 8–10 mCi of [11C]raclopride was injected into an antecubital vein over 60 s and emission data were then acquired over a period of 60 min. Two subjects were excluded from analysis—one from the PerAb group due to an interstitial raclopride injection during one of the PET scans, the other from the PhysAn group due to a serious traumatic personal event that occurred just prior to the nonstress PET session.
Each subject underwent a T1-weighted magnetic resonance imaging (MRI) scan for anatomical localization. PET emission frames were summed, registered to the individual MRI (Woods et al, 1993), and transformed into Montreal Neurological Institute space (Collins et al, 1994). We also used an automated head movement detection and correction procedure described previously (Zald et al, 2004).
Voxel-wise [11C]raclopride binding potential (BP) was calculated using a simplified reference tissue compartmental model (Lammertsma and Hume, 1996; Gunn et al, 1997) to generate statistical parametric images of change in BP (Aston et al, 2000). The reference method assumes that nonspecific binding of the tracer is equivalent in the striatum and reference region. Raclopride has been shown to have negligible nonspecific binding (Farde et al, 1985). We have demonstrated that this method is insensitive to changes in cerebral blood flow (Aston et al, 2000). There is considerable evidence from studies in nonhuman primates that the reduction in [11C]raclopride binding is proportional to DA release (Endres et al, 1997; Hartvig et al, 1997; Laruelle et al, 1997). Only peaks within the striatum were considered, since this is the only brain structure where receptor-specific [11C]raclopride binding is detected with certainty. T-maps of the change in BP were thresholded at a level of t>3.8, which corresponds to P<0.05, corrected for multiple comparisons (Worsley et al, 1996). The t threshold is based on a search volume for striatum of 37 264 mm3, an effective image filter of 12 mm full width at half maximum, and 230 degrees of freedom (Worsley et al, 1996; Aston et al, 2000). The search volume was set as the total number of striatal voxels with BP >1 in the averaged (across subjects) [11C]raclopride BP map. A mask was made of all striatal voxels with a T >3.2 to extract BP values from each individual's parametric images. These values were compared with pairwise t-tests between groups, and correlated with the smooth pursuit data (see below).
Psychological and Physiological Measures
Subjects completed the Spielberger State-Trait-Anxiety inventory (Spielberger et al, 1977), the questionnaire for competence and control for the assessment of self-concept related self-esteem (Krampen, 1991) and the parental bonding index (PBI), a well-validated self-report scale of parenting style (Parker et al, 1979; Parker, 1981). The last two measures were included because they were linked to stress response in our previous study (Pruessner et al, 2004). Assignment to the ‘high’ or ‘low’ maternal care category was based on a cutoff score of 27.0 (Parker et al, 1979). Perception of stress was assessed after each PET session by asking subjects to complete a state anxiety questionnaire (Spielberger et al, 1977) and visual analogue scales (VAS) (Pruessner et al, 2004) to assess feelings of negativity and uncontrollability at the end of the PET scan, prior to debriefing.
Saliva samples were collected every 12-min throughout the experiment. Saliva-derived cortisol was analyzed using a time-resolved fluorescence immunoassay (Dressendorfer et al, 1992) and the area under the curve (AUC; μg/dl/min) was calculated for each subject and each scanning session (Pruessner et al, 2003). Heart rate, electromyography (EMG), and skin conductance were measured throughout each PET session by electrodes placed on the left arm and chest (F1000 system, Focused Technology, Ridgecrest, CA 93556). Quantification of autonomic data was done using AUC calculations for each measure (Pruessner et al, 2003, 2004).
Smooth pursuit eye movements, a putative endophenotype for schizophrenia (Gottesman and Gould, 2003), were measured in 23 of the 26 subjects as part of a larger study (Holahan and O'Driscoll, 2005). Subjects were asked to follow the movement of a small square (0.5° × 0.5°) that moved across 20° of visual angle with a sinusoidal velocity profile at 0.4 Hz (for more details see Holahan and O'Driscoll, 2005). Eye movements were monitored using an Eyelink infrared video-based tracking system (SR Research, Mississauga, Canada) and data were analyzed with custom software (Holahan and O'Driscoll, 2005). The dependent measure was peak pursuit gain, a measure previously found to be correlated with frontal activation (O'Driscoll et al, 1999) and frontal structural integrity (Bagary et al, 2004). Pursuit gain was compared across groups with a one-way ANOVA. Correlations with were assessed with Pearson's r.
RESULTS
Behavioral Measures
A multivariate general linear model showed no group differences in self-esteem or trait anxiety scores. Subjects reported higher state anxiety scores (F=13.5, df=1, p<0.001) and higher VAS scores (F=16.749, df=1, p<0.001) after the stress session than after the nonstress session. There was no main effect of Group, and Group did not interact with Condition.
Although the software is designed to continuously vary task time constraints to ensure the same success rate and number of problems attempted for each subject, we calculated the rate of correct responses since differences in performance and feedback might influence the neural response. The success rate was 43±5% (mean±SD) and there were no differences between groups (F=0.13, df=2,22; p=0.88). There were also no significant group differences in percent correct during the nonstress session, or in total number of problems attempted or solved in either session.
D2 Binding Potential Maps
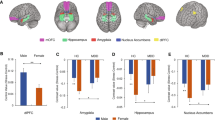
There was a significant reduction in [11C]raclopride BP in the stress condition compared to the control condition, indicative of DA release, only in the PhysAn group (peak t=7.8). The area of significantly reduced BP included bilateral ventral striatum, putamen, and caudate, with the highest t values located in the ventral striatum (Figure 1). There were no significant BP reductions in either the Control (peak t=3.0) or PerAb (peak t=2.89) groups.
Negative and positive schizotypy and stress-dopamine response. Decrease in binding potential (BP) during the stress condition compared to nonstress (indicative of dopamine release) in control and schizotype groups. One axial, one sagittal, and one coronal section of the statistical parametric map of the change in [11C]raclopride BP overlaid on the average MRI of all subjects in stereotaxic space. The color scale represents the t-statistic. (*p<0.001)
Region of interest data drawn from the area of significant DA release confirmed the t-map findings (Table 1; Figure 2). The reduction in BP from nonstress to stress was 9.8±13.6% in the PhysAn group (control BP and SD: 1.79±0.36, stress BP: 1.63±0.44, p=0.03). In the other two groups there was no evidence of DA release; indeed there was a slight nonsignificant increase in BP (control group nonstress: 1.56±0.34, stress: 1.60±0.44, 2.67% increase, p>0.2; PerAb group control: 1.61±0.26, stress: 1.63±0.22, 2.57% increase, p>0.2). We performed pairwise group comparisons on the region of interest data. Given our directional hypothesis that schizotypes would show greater DA release than controls, and the existing literature supporting this hypothesis (Breier et al, 1997; Abi-Dargham et al, 1998, 2004), t-tests between schizotypes and controls were one-tailed. PhysAn showed a trend toward a difference compared to the controls (p=0.08) but there was no difference between PerAb and controls (p=0.43). PhysAn demonstrated a trend toward greater DA release than PerAb (p=0.08, two-tailed). The PhysAn had higher nonstress BP than the other two groups but this did not reach statistical significance (p=0.1 compared to controls; p=0.12 compared to PerAb). There was a small (0.4 cm3) negative peak (greater BP in the stress condition) in the control group (t=−5.3) located in the left posterior putamen, but there were no negative peaks in either of the schizotypy groups. Although order was counterbalanced (stress or nonstress scan first) we confirmed that there were no order effects on stress-induced DA release (F=2.70; df=1,26; n.s.).
Binding potential (BP) in each condition. Mean [11C]raclopride BP extracted from the region of interest in the ventral striatum (see Materials and Methods). There was a significant difference in [11C]raclopride BP between stress and nonstress in the PhysAn group (p=0.03, one-tailed), but not in the other two groups.
We also measured parental bonding (Parker et al, 1979) based on our previous work (Pruessner et al, 2004). Changes in [11C]raclopride BP were significantly related to maternal care score across all subjects (r=−0.719; p<0.001). Subjects reporting low maternal care showed the greatest stress-induced reduction in BP, replicating our previous finding (Pruessner et al, 2004).
Relationship between Schizotypy And Maternal Care
ANOVA revealed a significant main effect of Group on maternal care scores (F=6.84; df=2,23; p=0.015). Contrasts indicated that both schizotypy groups reported significantly lower maternal care than controls (p<0.04) but did not differ from each other.
We did a stepwise discriminant function analysis of the data to predict membership in the three groups (PhysAn, PerAb, and control) using all the self-report measures, physiological measures of stress, and change in D2 binding. The best-fit two functions grouped 72% of the original cases correctly, even when adjusting for group size (df=4,25, Wilks' Lambda=0.437, p=0.003). The two significant predictors of group membership were change in D2 BP between control and stress sessions and perceived maternal care; the functions classified 100% of controls, 71.4% of PhysAn subjects, and 44.4% of PerAb subjects correctly. No misclassified schizotype subjects were assigned to the control group.
Endocrine and Physiological Stress Response
The stress session resulted in significant increases in salivary cortisol compared with the nonstress session (AUC units, μg/dl/min: mean difference 0.62±0.07; F=85.51; df=1,22; p<0.001). There were no group differences in cortisol response between the two schizotype and control groups nor between the two maternal care groups, and DA release was not correlated with cortisol levels. The stress paradigm also resulted in higher heart rate (mean difference 102.8±21.2 beats/min2; F=10.64; df=1,22; p=0.004), and EMG response (mean difference 32.8±12.1 contractions/min−2; F=6.99; df=1,22; p=0.015) but not skin conductance. There was no main effect of Group on any physiological variables and no Group–Condition interactions.
Smooth Pursuit Gain
There was no main effect of Group on pursuit gain in this small sample (Table 1). Smooth pursuit gain was significantly correlated with measures of [11C]raclopride BP; nonstress BP was correlated with pursuit gain (r=−0.43, n=23, p=0.04) as was stress-induced change in BP (r=−0.41, n=23, p=0.05) (Figure 3).
Smooth pursuit and dopamine function. Correlations between smooth pursuit gain (eye velocity/target velocity) and nonstress [11C]raclopride binding potential (BP) (left panel, p=0.04) and stress-induced change in [11C]raclopride BP (nonstress—stress, right panel, p=0.05). The subjects with lower smooth pursuit gain had greater nonstress BP and greater stress-induced dopamine release.
DISCUSSION
Negative symptom psychometric schizotypes showed significant striatal DA release in response to stress. This effect was not observed in the PerAb group or in controls.
Previous studies have shown that schizophrenic and schizotypal personality disorder patients have an exaggerated DA response to amphetamine (Laruelle et al, 1996; Breier et al, 1997; Abi-Dargham et al, 2004). Our data extend these findings by showing an elevated DA response to an ecological social stress as opposed to a pharmacological challenge. Moreover, this increased DA response occurred in a group at elevated risk for psychosis that had no Axis I psychopathology.
We found the two psychometric schizotype groups to differ in their stress-induced DA release, with only the PhysAn group (negative schizotypy) showing an exaggerated DA response. In schizophrenic patients, increases in striatal DA release have generally been associated with the presence of positive symptoms (Laruelle et al, 1996, 1999; Abi-Dargham et al, 1998). However, the genetic liability for schizophrenia is thought to be better indexed by negative than positive symptom schizotypy (Tsuang et al, 1991). For example, PhysAn scores are elevated in the relatives of schizophrenic patients while PerAb scores are not (Katsanis et al, 1990; Clementz et al, 1991) and lifetime risk of schizophrenia-spectrum disorders is higher in relatives of anhedonic schizophrenia probands than in nonanhedonic probands (Schurhoff et al, 2003). Negative, but not positive, symptoms are also elevated in schizophrenia families (Tsuang et al, 1991), and PhysAn is a major component of the stable familial set of traits referred to as ‘schizotaxia’, which is observed in a subset of relatives (Tsuang et al, 2002). That PhysAn but not PerAb subjects showed an elevated DA response to stress is consistent with the idea that positive and negative schizotypy represent different forms of risk that may follow divergent paths to symptom development (Fanous et al, 2001).
A possible neural basis for the striatal DA hyperreactivity in our PhysAn group is reduced frontal lobe function (Davis et al, 1991). A large body of literature has linked negative symptoms with poor frontal function, and impaired frontal activation is associated with elevated striatal DA neurotransmission in schizophrenic patients (Meyer-Lindenberg et al, 2002). Grace's revision of the classic DA hypothesis (Grace, 1991, 2003) differentiates between phasic and tonic DA release in the striatum, and posits that low tonic activity is associated with the expression of negative symptoms. Compensatory changes resulting from low tonic DA, such as reduced stimulation of presynaptic DA receptors, are hypothesized to produce a heightened phasic DA response to stressors, which may be associated with psychosis. In this model, the abnormalities in subcortical DA are a downstream effect of reduced activity in prefrontal cortex, and in particular hypoactivity of prefrontal glutamatergic neurons (Moore et al, 1999). The reduction of frontal excitatory input to mesolimbic and mesocortical DA neurons could reduce tonic activity, while also resulting in an excessive mesolimbic response to exogenous stimuli such as stress (Moore et al, 1999; Laruelle et al, 2003). This model is consistent with our findings, as it predicts that psychosis-susceptible individuals will have higher [11C]raclopride BP, reflecting low tonic DA, as shown here (Figure 2), larger stress-induced DA release (Figures 1 and 2), and that these should be associated with measures of frontal dysfunction (Figure 3).
We do not have direct measures of frontal function in this population. However, it has been reported that smooth pursuit quality (measured by pursuit gain or catch-up saccade rate) is significantly associated with measures of frontal structural integrity (Bagary et al, 2004) and frontal activation in schizophrenic patients (Ross et al, 1995; Hong et al, 2005; Keedy et al, 2006) and unaffected relatives (O'Driscoll et al, 1999). Although the PhysAn group did tend towards poorer pursuit gain, the small number of subjects made these results insignificant here. Nonetheless, in the larger samples tested (Holahan and O'Driscoll, 2005), schizotypes did have significantly lower pursuit gain than controls, and this was most significant for the PhysAn group In the current study, we correlated smooth pursuit gain with [11C]raclopride BP measures and found the hypothesized significant association with both nonstress BP and stress-induced DA release (Figure 3), with subjects with lower pursuit gain having higher nonstress BP (ie lower tonic DA activity) and higher DA release (ie higher phasic DA activity). This evidence, although indirect, supports the notion of a link between frontal dysfunction and striatal DA function.
We should highlight our study limitations. First, since the parametric images shown represent thresholded statistical maps, the area of DA release might have been larger than that displayed in the figures. Moreover, because we report PET data to minimize false-positive results, we cannot exclude the presence of small changes in [11C]raclopride undetected by our method. Also, we cannot exclude the possibility that variations in cerebral blood flow during the scan could have affected our measurement of [11C]raclopride BP (Slifstein et al, 2004), since our simulations showing that the compartmental model used here adequately separates tracer delivery from binding to receptors were made under the assumption of constant blood flow (Aston et al, 2000). Second, the tracer [11C]raclopride only displays specific binding in subcortical areas. Though the striatum is thought to be a critical region for DA dysfunction in schizophrenia, there may also be differences in frontal cortical DA systems that our method could not detect. Third, although our particular interest is in schizophrenia vulnerability, our personality measures of vulnerability are sensitive to risk for psychosis, including affective psychosis (Erlenmeyer-Kimling et al, 1993; Chapman et al, 1994). Increased DA release in response to stress may represent a risk factor for psychosis in general, rather than a risk factor for schizophrenia per se (Yui et al, 2004). Fourth, we did not find DA release to be correlated with cortisol levels, as was found in our previous study (Pruessner et al, 2004), nor did we observe differences in cortisol between groups, a result likely due to our low number of participants. Fifth, it is possible that factors other than schizotypy influenced the stress-induced DA and neuroendocrine responses we observed. The exclusion of schizotypal individuals meeting Axis 1 criteria, albeit to remove possible confounds, might have eliminated some ‘true positive’ individuals, and thus could have reduced our ability to find dopaminergic abnormalities in the PerAb group. Moreover, since groups were composed primarily of females, neuroendocrine responses to psychosocial stress could have been influenced by the sex composition of the groups (Kirschbaum et al, 1992). Differences between the stress and nonstress conditions may also have been a factor; the conditions were balanced for motor and visual stimuli, but only the stress condition involved contact with a confederate. Although unlikely, the possibility that nonstressful aspects of the interaction (eg attention, auditory input) could have caused DA release cannot be excluded. Besides these limitations, our data do not address the question of causality and mechanism. For example, it is unclear to what extent stress-induced differences in DA release seen in the PhysAn group are attributable to the differences in the distribution of low/high maternal care in the different groups, since in a previous study (Pruessner et al, 2004) low maternal care participants showed greater stress-induced DA release. However, the discriminant function analysis showed that both DA release and maternal care score independently predicted schizotypy group membership, indicating that DA release improves the identification of PhysAn subjects beyond that provided by maternal care scores. The cross-sectional design and the low number of subjects in this imaging study preclude speculation about the basis of the relationship between maternal care and schizotypy.
Notwithstanding, this is to our knowledge the first demonstration of increased stress-induced DA release in a population at risk for any psychotic disorder; future work will be necessary to determine to what extent it may be relevant for one disorder more than others. Our stimulus, stress, is distinctive and relevant in two ways: it is associated with psychosis-onset (Norman and Malla, 1993; Nuechterlein et al, 1994; Walker and Diforio, 1997) and it is not a pharmacological challenge. Additional strengths of the study include individual adjustment of the stress paradigm to produce performance matching in the scanner across groups, and that the task produced the expected physiological, endocrine, and self-report changes associated with stress in all the three groups. Thus our findings of increased stress-related DA release in the PhysAn group cannot be attributed to methodological confounds such as clinical manifestation of disease, comorbidity, performance differences, or differences in perceived stress or state anxiety.
References
Abercrombie ED, Keefe KA, DiFrischia DS, Zigmond MJ (1989). Differential effect of stress on in vivo dopamine release in striatum, nucleus accumbens, and medial frontal cortex. J Neurochem 52: 1655–1658.
Abi-Dargham A, Gil R, Krystal J, Baldwin RM, Seibyl JP, Bowers M et al (1998). Increased striatal dopamine transmission in schizophrenia: confirmation in a second cohort. Am J Psychiatry 155: 761–767.
Abi-Dargham A, Kegeles LS, Zea-Ponce Y, Mawlawi O, Martinez D, Mitropoulou V et al (2004). Striatal amphetamine-induced dopamine release in patients with schizotypal personality disorder studied with single photon emission computed tomography and [123I]iodobenzamide. Biol Psychiatry 55: 1001–1006.
Adler CM, Elman I, Weisenfeld N, Kestler L, Pickar D, Breier A (2000). Effects of acute metabolic stress on striatal dopamine release in healthy volunteers. Neuropsychopharmacology 22: 545–550.
Allen JJ, Chapman LJ, Chapman JP (1987). Cognitive slippage and depression in hypothetically psychosis-prone college students. J Nerv Ment Dis 175: 347–353.
Aston JAD, Gunn RN, Worsley KJ, Ma Y, Evans AC, Dagher A (2000). A statistical method for the analysis of positron emission tomography neuroreceptor ligand data. Neuroimage 12: 245–256.
Bagary MS, Hutton SB, Symms MR, Barker GJ, Mutsatsa SH, Barnes TR et al (2004). Structural neural networks subserving oculomotor function in first-episode schizophrenia. Biol Psychiatry 56: 620–627.
Blanchard JJ, Mueser KT, Bellack AS (1998). Anhedonia, positive and negative affect, and social functioning in schizophrenia. Schizophr Bull 24: 413–424.
Breier A, Su TP, Saunders R, Carson RE, Kolachana BS, de Bartolomeis A et al (1997). Schizophrenia is associated with elevated amphetamine-induced synaptic dopamine concentrations: evidence from a novel positron emission tomography method. Proc Natl Acad Sci USA 94: 2569–2574.
Chapman LJ, Chapman JP, Kwapil TR, Eckblad M, Zinser MC (1994). Putatively psychosis-prone subjects 10 years later. J Abnorm Psychol 103: 171–183.
Chapman LJ, Chapman JP, Raulin ML (1976). Scales for physical and social anhedonia. J Abnorm Psychol 85: 374–382.
Chapman LJ, Chapman JP, Raulin ML (1978). Body-image aberration in schizophrenia. J Abnorm Psychol 87: 399–407.
Chapman LJ, Edell WS, Chapman JP (1980). Physical anhedonia, perceptual aberration, and psychosis proneness. Schizophr Bull 6: 639–653.
Clementz BA, Grove WM, Katsanis J, Iacono WG (1991). Psychometric detection of schizotypy: perceptual aberration and physical anhedonia in relatives of schizophrenics. J Abnorm Psychol 100: 607–612.
Collins DL, Neelin P, Peters TM, Evans AC (1994). Automatic 3D intersubject registration of MR volumetric data in standardized Talairach space. J Comput Assist Tomogr 18: 192–205.
Davis KL, Kahn RS, Ko G, Davidson M (1991). Dopamine in schizophrenia: a review and reconceptualization. Am J Psychiatry 148: 1474–1486.
Dawson ME, Nuechterlein KH (1984). Psychophysiological dysfunctions in the developmental course of schizophrenic disorders. Schizophr Bull 10: 204–232.
Dressendorfer RA, Kirschbaum C, Rohde W, Stahl F, Strasburger CJ (1992). Synthesis of a cortisol-biotin conjugate and evaluation as a tracer in an immunoassay for salivary cortisol measurement. J Steroid Biochem Mol Biol 43: 683–692.
Elman I, Lukas S, Shoaf SE, Rott D, Adler C, Breier A (2003). Effects of acute metabolic stress on the peripheral vasopressinergic system in schizophrenia. J Psychopharmacol 17: 317–323.
Endres CJ, Kolachana BS, Saunders RC, Su T, Weinberger D, Breier A et al (1997). Kinetic modeling of [11C]raclopride: combined PET-microdialysis studies. J Cereb Blood Flow Metab 17: 932–942.
Erlenmeyer-Kimling L, Cornblatt BA, Rock D, Roberts S, Bell M, West A (1993). The New York High-Risk Project: anhedonia, attentional deviance, and psychopathology. Schizophr Bull 19: 141–153.
Fanous A, Gardner C, Walsh D, Kendler KS (2001). Relationship between positive and negative symptoms of schizophrenia and schizotypal symptoms in nonpsychotic relatives. Arch Gen Psychiatry 58: 669–673.
Farde L, Ehrin E, Eriksson L, Greitz T, Hall H, Hedstrom CG et al (1985). Substituted benzamides as ligands for visualization of dopamine receptor binding in the human brain by positron emission tomography. Proc Natl Acad Sci USA 82: 3863–3867.
First M, Spitzer R, Gibbon M, Williams J (1996). Structured Clinical Interview for DSM-IV Axis I Disorders. New York State Psychiatric Institute: New York.
Franke P, Maier W, Hardt J, Hain C (1993). Cognitive functioning and anhedonia in subjects at risk for schizophrenia. Schizophr Res 10: 77–84.
Freedman LR, Rock D, Roberts SA, Cornblatt BA, Erlenmeyer-Kimling L (1998). The New York High-Risk Project: attention, anhedonia and social outcome. Schizophr Res 30: 1–9.
Garnet KE, Glick M, Edell WS (1993). Anhedonia and premorbid competence in young, nonpsychotic psychiatric inpatients. J Abnorm Psychol 102: 580–583.
Gooding DC, Miller MD, Kwapil TR (2000). Smooth pursuit eye tracking and visual fixation in psychosis-prone individuals. Psychiatry Res 93: 41–54.
Gooding DC, Tallent KA, Hegyi JV (2001). Cognitive slippage in schizotypic individuals. J Nerv Ment Dis 189: 750–756.
Gottesman II, Gould TD (2003). The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry 160: 636–645.
Grace AA (1991). Phasic versus tonic dopamine release and the modulation of dopamine system responsivity: a hypothesis for the etiology of schizophrenia. Neuroscience 41: 1–24.
Grace AA (2003). Developmental dysregulation of the dopamine system and the pathophysiology of schizophrenia. In: Keshavan M, Kennedy JL, Murray RM (eds). Neurodevelopment and Schizophrenia. Cambridge University Press: New York, pp 273–294.
Gunn RN, Lammertsma AA, Hume SP, Cunningham VJ (1997). Parametric imaging of ligand-receptor binding in PET using a simplified reference region model. Neuroimage 6: 279–287.
Hartvig P, Torstenson R, Tedroff J, Watanabe Y, Fasth KJ, Bjurling P et al (1997). Amphetamine effects on dopamine release and synthesis rate studied in the Rhesus monkey brain by positron emission tomography. J Neural Transm 104: 329–339.
Hathaway SR, McKinley JC (1989). Minnesota Multiphasic Personality Inventory-2. University of Minnesota Press: Minneapolis.
Holahan A-LV, O'Driscoll GA (2005). Antisaccade and smooth pursuit performance in positive- and negative-symptom schizotypy. Schizophr Res 76: 43–54.
Hong LE, Tagamets M, Avila M, Wonodi I, Holcomb H, Thaker GK (2005). Specific motion processing pathway deficit during eye tracking in schizophrenia: a performance-matched functional magnetic resonance imaging study. Biol Psychiatry 57: 726–732.
Jutai JW (1989). Spatial attention in hypothetically psychosis-prone college students. Psychiatry Res 27: 207–215.
Katsanis J, Iacono WG, Beiser M (1990). Anhedonia and perceptual aberration in first-episode psychotic patients and their relatives. J Abnorm Psychol 99: 202–206.
Keedy SK, Ebens CL, Keshavan MS, Sweeney JA (2006). Functional magnetic resonance imaging studies of eye movements in first episode schizophrenia: smooth pursuit, visually guided saccades and the oculomotor delayed response task. Psychiatry Res 146: 199–211.
Kirschbaum C, Wust S, Hellhammer D (1992). Consistent sex differences in cortisol responses to psychological stress. Psychosom Med 54: 648–657.
Krampen G (1991). Fragebogen zu Kompetenz- und Kontrollueberzeugungen (FKK). Hogrefe: Göttingen.
Kwapil TR, Chapman JP, Chapman LJ, Miller MB (1996). Deviant olfactory experiences as indicators of risk for psychosis. Schizophr Bull 22: 371–382.
Kwapil TR, Miller MB, Zinser MC, Chapman J, Chapman LJ (1997). Magical ideation and social anhedonia as predictors of psychosis proneness: a partial replication. J Abnorm Psychol 106: 491–495.
Lammertsma AA, Hume SP (1996). Simplified reference tissue model for PET receptor studies. Neuroimage 4: 153–158.
Laruelle M, Abi-Dargham A, Gil R, Kegeles L, Innis R (1999). Increased dopamine transmission in schizophrenia: relationship to illness phases. Biol Psychiatry 46: 56–72.
Laruelle M, Abi-Dargham A, van Dyck CH, Gil R, D'Souza CD, Erdos J et al (1996). Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proc Natl Acad Sci USA 93: 9235–9240.
Laruelle M, Iyer RN, al-Tikriti MS, Zea-Ponce Y, Malison R, Zoghbi SS et al (1997). Microdialysis and SPECT measurements of amphetamine-induced dopamine release in nonhuman primates. Synapse 25: 1–14.
Laruelle M, Kegeles LS, Abi-Dargham A (2003). Glutamate, dopamine, and schizophrenia: from pathophysiology to treatment. Ann NY Acad Sci 1003: 138–158.
Lenzenweger MF (1991). Confirming schizotypic personality configurations in hypothetically psychosis-prone university students. Psychiatry Res 37: 81–96.
Lenzenweger MF, Loranger AW (1989). Detection of familial schizophrenia using a psychometric measure of schizotypy. J Abnorm Psychol 46: 902–907.
Meyer-Lindenberg A, Miletich RS, Kohn PD, Esposito G, Carson RE, Quarantelli M et al (2002). Reduced prefrontal activity predicts exaggerated striatal dopaminergic function in schizophrenia. Nat Neurosci 5: 267–271.
Miller GA (1986). Information processing deficits in anhedonia and perceptual aberration: a psychophysiological analysis. Biol Psychiatry 21: 100–115.
Mitropoulou V, Goodman M, Sevy S, Elman I, New AS, Iskander EG et al (2004). Effects of acute metabolic stress on the dopaminergic and pituitary-adrenal axis activity in patients with schizotypal personality disorder. Schizophr Res 70: 27–31.
Moore H, West AR, Grace AA (1999). The regulation of forebrain dopamine transmission: relevance to the pathophysiology and psychopathology of schizophrenia. Biol Psychiatry 46: 40–55.
Norman RM, Malla AK (1993). Stressful life events and schizophrenia. I: a review of the research. Br J Psychiatry 162: 161–166.
Nuchpongsai P, Arakaki H, Langman P, Ogura C (1999). N2 and P3b components of the event-related potential in students at risk for psychosis. Psychiatry Res 88: 131–141.
Nuechterlein KH, Dawson ME, Ventura J, Gitlin M, Subotnik KL, Snyder KS et al (1994). The vulnerability/stress model of schizophrenic relapse: a longitudinal study. Acta Psychiatr Scand Suppl 382: 58–64.
O'Driscoll GA, Benkelfat C, Florencio PS, Wolff AL, Joober R, Lal S et al (1999). Neural correlates of eye tracking deficits in first-degree relatives of schizophrenic patients: a positron emission tomography study. Arch Gen Psychiatry 56: 1127–1134.
O'Driscoll GA, Strakowski SM, Alpert NM, Matthysse SW, Rauch SL, Levy DL et al (1998). Differences in cerebral activation during smooth pursuit and saccadic eye movements using positron-emission tomography. Biol Psychiatry 44: 685–689.
Parker G (1981). Parental reports of depressives: an investigation of several explanations. J Affect Disord 3: 131–140.
Parker G, Tupling H, Brown LB (1979). A parental bonding instrument. Br J Med Psychol 52: 1–10.
Pruessner JC, Champagne F, Meaney MJ, Dagher A (2004). Dopamine release in response to a psychological stress in humans and its relationship to early life maternal care: a positron emission tomography study using [11C]raclopride. J Neurosci 24: 2825–2831.
Pruessner JC, Hellhammer DH, Kirschbaum C (1999). Low self-esteem, induced failure and the adrenocortical stress response. Pers Indiv Dif 27: 477–489.
Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH (2003). Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology 28: 916–931.
Reynolds CA, Raine A, Mellingen K, Venables PH, Mednick SA (2000). Three-factor model of schizotypal personality: invariance across culture, gender, religious affiliation, family adversity, and psychopathology. Schizophr Bull 26: 603–618.
Robins LN, Helzer JE, Croughan J, Ratcliff KS (1981). National Institute of Mental Health Diagnostic Interview Schedule. Its history, characteristics, and validity. Arch Gen Psychiatry 38: 381–389.
Ross DE, Thaker GK, Holcomb HH, Cascella NG, Medoff DR, Tamminga CA (1995). Abnormal smooth pursuit eye movements in schizophrenic patients are associated with cerebral glucose metabolism in oculomotor regions. Psychiatry Res 58: 53–67.
Rouge-Pont F, Piazza PV, Kharouby M, Le Moal M, Simon H (1993). Higher and longer stress-induced increase in dopamine concentrations in the nucleus accumbens of animals predisposed to amphetamine self-administration. A microdialysis study. Brain Res 602: 169–174.
Schurhoff F, Szoke A, Bellivier F, Turcas C, Villemur M, Tignol J et al (2003). Anhedonia in schizophrenia: a distinct familial subtype? Schizophr Res 61: 59–66.
Simons RF (1982). Physical anhedonia and future psychopathology: an electrocortical continuity? Psychophysiology 19: 433–441.
Simons RF, Giardina BD (1992). Reflex modification in psychosis-prone young adults. Psychophysiology 29: 8–16.
Slifstein M, Narendran R, Hwang DR, Sudo Y, Talbot PS, Huang Y et al (2004). Effect of amphetamine on [(18)F]fallypride in vivo binding to D(2) receptors in striatal and extrastriatal regions of the primate brain: single bolus and bolus plus constant infusion studies. Synapse 54: 46–63.
Spielberger CD, Gorsuch RL, Lushene RE, Vagg PR, Jacobs GA (1977). State and Trait Anxiety Inventory for Adults. Mind Garden: Redwood City, CA.
Suhr JA (1997). Executive functioning deficits in hypothetically psychosis-prone college students. Schizophr Res 27: 29–35.
Suhr JA, Spitznagel MB (2001). Factor versus cluster models of schizotypal traits. I: a comparison of unselected and highly schizotypal samples. Schizophr Res 52: 231–239.
Sumiyoshi T, Saitoh O, Yotsutsuji T, Itoh H, Kurokawa K, Kurachi M (1999). Differential effects of mental stress on plasma homovanillic acid in schizophrenia and normal controls [see comment]. Neuropsychopharmacology 20: 365–369.
Thaker GK (2000). Defining the schizophrenia phenotype. Curr Psychiatry Rep 2: 398–403.
Thompson JL, Pogue-Geile MF, Grace AA (2004). Developmental pathology, dopamine, and stress: a model for the age of onset of schizophrenia symptoms. Schizophr Bull 30: 875–900.
Tsuang MT, Gilbertson MW, Faraone SV (1991). Genetic transmission of negative and positive symptoms in the biological relatives of schizophrenics. In: Marneros A, Tsuang MT, Andreasen N (eds). Positive vs Negative Schizophrenia. Springer-Verlag: New York, pp 265–291.
Tsuang MT, Stone WS, Faraone SV (2002). Understanding predisposition to schizophrenia: toward intervention and prevention. Can J Psychiatry 47: 518–526.
Walker EF, Diforio D (1997). Schizophrenia: a neural diathesis-stress model. Psychol Rev 104: 667–685.
Wilkins S, Venables PH (1992). Disorder of attention in individuals with schizotypal personality. Schizophr Bull 18: 717–723.
Woods RP, Mazziotta JC, Cherry SR (1993). MRI-PET registration with automated algorithm. J Comput Assist Tomogr 17: 536–546.
Worsley KJ, Marrett S, Neelin P, Vandal AC, Friston KJ, Evans AC (1996). A unified statistical approach for determining significant signals in images of cerebral activation. Hum Brain Mapp 4: 58–73.
Yui K, Goto K, Ikemoto S (2004). The role of noradrenergic and dopaminergic hyperactivity in the development of spontaneous recurrence of methamphetamine psychosis and susceptibility to episode recurrence. Ann NY Acad Sci 1025: 296–306.
Zald DH, Boileau I, El-Dearedy W, Gunn R, McGlone F, Dichter GS et al (2004). Dopamine transmission in the human striatum during monetary reward tasks. J Neurosci 24: 4105–4112.
Acknowledgements
This work was supported in part by operating grants from the Canadian Institutes for Health Research. We thank Mirko Diksic, Rick Fukasawa, Gary Sawchuk, Shadrack Mzengeza, Dean Jolly, and Miriam Kovacevic of the McConnell Brain Imaging Centre for their collaboration.
Author information
Authors and Affiliations
Corresponding author
Additional information
Disclosure/Conflict of Interest
The authors declare that, except for income received from a primary employer, no financial support or compensation has been received from any individual or corporate entity over the past three years for research or professional service and there are no personal financial holdings that could be perceived as constituting a potential conflict of interest.
Rights and permissions
About this article
Cite this article
Soliman, A., O'Driscoll, G., Pruessner, J. et al. Stress-Induced Dopamine Release in Humans at Risk of Psychosis: a [11C]Raclopride PET Study. Neuropsychopharmacol 33, 2033–2041 (2008). https://doi.org/10.1038/sj.npp.1301597
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301597
Keywords
This article is cited by
-
The cancer-immune dialogue in the context of stress
Nature Reviews Immunology (2024)
-
Negative schizotypal traits predict the reduction of reward motivation in effort–reward imbalance
European Archives of Psychiatry and Clinical Neuroscience (2023)
-
Identification of cerebrospinal fluid and serum metabolomic biomarkers in first episode psychosis patients
Translational Psychiatry (2022)
-
Using questionnaires and task-related EEG signals to reveal hindered reappraisal and biased suppression in individuals with high schizotypal traits
Scientific Reports (2020)
-
Migration and schizophrenia: meta-analysis and explanatory framework
European Archives of Psychiatry and Clinical Neuroscience (2020)