Abstract
Patients with schizophrenia exhibit disturbances of orienting of attention. However, findings have been inconsistent. Pharmacologic challenges with hallucinogens have been used as models for psychosis. The NMDA antagonist state (PCP, ketamine) resembles undifferentiated psychoses with positive and negative symptoms, while the 5-HT2A agonist state (LSD, dimethyltryptamine (DMT)) is thought to be an appropriate model for psychoses with prominent positive symptoms. The aim of this study was to investigate orienting of attention in the human NMDA antagonist and 5-HT2A agonist models of psychosis. A total of 15 healthy volunteers participated in a randomized, double-blind, crossover study with a low and a high dose of DMT and S-ketamine, which elicited subtle ‘prepsychotic’ or full-blown psychotic symptoms (low and high dose, respectively). Nine subjects completed both experimental days with the two doses of both drugs. Overall, both hallucinogens slowed down reaction times dose dependently (DMT >S-ketamine) and DMT diminished the general response facilitating (alerting) effect of spatially neutral cues. Inhibition of Return (IOR), that is, the normal reaction time disadvantage for validly cued trials with exogenous cues and long cue target intervals, was blunted after both doses of DMT and the low dose of S-ketamine. IOR reflects an automatic, inhibitory mechanism of attention, which is thought to protect the organism from redundant, distracting sensory information. In conclusion, our data suggest a deficit of IOR in both hallucinogen models of psychosis, with the effect being clearer in the serotonin model. Blunted IOR may underlie or predispose to different psychotic manifestations, but particularly to those with prominent positive symptoms.
Similar content being viewed by others
INTRODUCTION
Deficits in attentional functions such as sustained and divided attention are common symptoms in schizophrenia and they are important predictors of the long-term clinical and sociorehabilitative outcome of patients (Addington and Addington, 1998). Recently, there has been growing interest in spatial orienting of visual attention in patients with schizophrenia.
In typical covert orienting of attention tasks (COVATs) subjects have to maintain fixation to a central cross and respond as quickly as possible to a target that appears in a peripheral box following a cue that summons attention to the direction where the target is going to appear (valid cueing) or to the contralateral direction (invalid cueing). In principle, COVATs may use two different sorts of cues. The so-called endogenous cues depend on conscious, directed mechanisms shifting attention towards the source of stimulation. A typical endogenous cue may be an arrow located centrally and pointing to one peripheral box where the target is going to appear with high probability (predictive cue). Reaction times (RTs) in trials with endogenous valid cues are facilitated, and RTs in invalidly cued trials are particularly long, because attention has to be disengaged from the previously cued location and shifted to the direction of the target. In contrast, the so-called exogenous cues (eg brightening of one peripheral box prior to the appearance of the target) capture visual attention automatically without involvement of directed attentional mechanisms. Interestingly, when valid and invalid exogenous cues appear at the same frequency—and therefore they do not predict the subsequent location of the target—, RTs to the target critically depend on cue target intervals (stimulus onset asynchrony=SOA=time from onset of cue to onset of target): With short SOAs (<200 ms), valid cues result in an RT advantage over invalid trials, which is due to a reflexive shift of attention towards the source of stimulation. In contrast, with longer SOAs (>250 ms), valid cues result in longer RTs to the subsequent target (Posner and Cohen, 1984). Although this phenomenon is not entirely understood, it is mostly thought to reflect an automatic, inhibitory mechanism protecting the organism from redirecting attention to previously scanned, insignificant locations. This belief is reflected by the term Inhibition of Return (IOR) (Posner and Cohen, 1984).
Early studies in patients with schizophrenia reported a particularly slow detection of targets in the right visual field following invalid cues and short SOAs of about 100 ms (Posner et al, 1988; Potkin et al, 1989; Maruff et al, 1995; Wigal et al, 1997). This finding was interpreted as a lateralized deficit in disengaging attention from the previously cued location. However, evidence for this deficit has been very inconsistent including some negative (Strauss et al, 1991, 1992; Gold et al, 1992; Gouzoulis-Mayfrank et al, 2004) and even some opposite findings of an abnormal facilitation of disengagement of attention in patients with schizophrenia (Nestor et al, 1992; Oie et al, 1998). Finally, there has been some indication that the deficit in disengaging attention might be present only in acute and unmedicated, but not in chronic patients or in patients receiving neuroleptic medication (Strauss et al, 1992; Maruff et al, 1995; Wigal et al, 1997). Another interesting finding has been blunted or delayed IOR (Huey and Wexler, 1994; Carter et al, 1994; Sapir et al, 2001; Larrison-Faucher et al, 2002; Gouzoulis-Mayfrank et al, 2004, 2005a). Overall, the IOR data tend to be more consistent across publications. However, some studies reported a normal amount of IOR (Carter et al, 1992; Maruff et al, 1998; Fuentes and Santiago, 1999; Fuentes et al, 1999) and one study reported blunted IOR only in patients with the paranoid, but not with the undifferentiated type of schizophrenia (Carter et al, 1994).
In conclusion, the literature on orienting of visual attention in schizophrenia is inconsistent. Both task- and subject-related methodological issues may account for the discrepancies across studies. The literature does not always differentiate between tasks with exogenous and endogenous cues and some early studies used ‘mixed’ paradigms with exogenous, but predictive cues (eg brightening of a peripheral box followed by the target in that box with an 80% probability), thus precluding interpretation of their findings in respect to the underlying attentional mechanisms (Posner et al, 1988; Strauss et al, 1991, 1992; Gold et al, 1992; Liotti et al, 1993; Oie et al, 1998). Additional differences in the tasks used across the different studies are also likely to account for some inconsistencies (eg single cue vs cue-back paradigms, see Fuentes and Santiago, 1999; Fuentes et al, 1999; Gouzoulis-Mayfrank et al, 2005a). Finally, subject-related issues such as the biological heterogeneity of the schizophrenic disorder, different medications and aspects of the age of onset, and long-term course of the disorder may also account for some discrepancies across the literature.
In respect to these latter subject-related methodological issues, human experimental studies with hallucinogenic drugs may be a valuable, complementary research strategy to studies with patient populations. Hallucinogenic drug states resemble clinical manifestations of schizophrenia. Therefore, pharmacological challenges with hallucinogens have often been used as models for psychosis, although there is some controversy as to the closeness of these models to schizophrenia (eg Snyder, 1988; Gouzoulis-Mayfrank et al, 1998a, 1999a, 1999b; D'Souza et al, 1999; Carpenter, 1999). Intraindividual comparisons of the off- and on-drug state help to minimize the variability of data and offer a unique opportunity to study fundamental neurobiological mechanisms of psychoses. Interestingly, the two major classes of hallucinogens (PCP-type: glutamate NMDA receptor antagonists, and LSD-type: serotonin 5-HT2A receptor agonists or partial agonists) have somewhat different psychotropic profiles, and therefore, they may model different aspects or types of schizophrenia. The NMDA antagonist state (PCP, ketamine) is thought to be an appropriate model for undifferentiated or disorganized psychoses with both positive and negative symptoms, while the 5-HT2A agonist state (LSD, dimethyltryptamine (DMT), psilocybin) may be an appropriate model for the paranoid subtype of schizophrenia (Javitt and Zukin, 1991; Krystal et al, 1994; Abi-Saab et al, 1998; Gouzoulis-Mayfrank et al, 2005b).
In a previous study, we found some indication for deficits in both disengagement of attention and IOR in the psilocybin 5-HT2A model of psychosis (Gouzoulis-Mayfrank et al, 2002). However, the use of a ‘mixed’ paradigm with exogenous, but predictive cues made it difficult to interprete those findings. The aim of the present experiment was to study orienting of attention in human hallucinogen ‘model psychoses’ in a more sophisticated design using two different versions of the COVAT and two doses of the 5-HT2A agonist DMT and the NMDA antagonist S-ketamine. Both drugs can be given intravenously and have similar pharmacokinetics with rapid onset and rapid fading of action after the end of the infusion, thus making it possible to study the effects of the two drug states in a randomized, double-blind design. Based on the literature with patients with schizophrenia (Strauss et al, 1992; Carter et al, 1994; Maruff et al, 1995; Wigal et al, 1997), we expected to find a deficit in disengaging attention after both hallucinogens and an IOR deficit after DMT, but not necessarily after S-ketamine.
MATERIALS AND METHODS
Subjects
In total, 15 healthy volunteers (nine men, six women; mean age 38.0 years, range: 28–53) with no current physical and no current or previous history of neurological or psychiatric disorder (Axis I according to DSM-IV criteria, APA, 1994) were included in the study. Subjects with a positive family history of psychotic or major affective psychiatric disorder in first-degree relatives, a personal history of current or previous alcohol or drug related disorder, or under regular medication were excluded. All subjects were screened with a medical history, a standardized psychiatric interview (SCID) and a physical examination, ECG, and a routine laboratory testing. No subject had been under medication or subject to excessive caffeine intake and/or stressful life events in the 4 weeks prior to the study. All subjects were either physicians or psychologists or psychiatric nursing staff, but they were no direct employees of the experimenters. They had a scientific or clinical interest in the study and did not receive any payment for their participation.
The study was carried out in accordance with the Declaration of Helsinki and was approved by the ethics committee at the Medical Faculty of the University of Technology Aachen and the Federal Health Administration (Bundesinstitut für Arzneimittel und Medizinprodukte, Bundesopiumstelle Berlin). Written informed consent was obtained from all subjects following detailed description of the experimental procedures and assurance that they could withdraw from the study at any time, if they wish so, without having to explain the reasons.
Drugs
Dimethyltryptamine fumarate (DMT) was synthesized in the Pharmaceutical Institute, University of Tübingen (Germany) and prepared as solution for intravenous use by Wülfing Pharma (Gronau, Germany). The S-ketamine solution (Ketanest® S, Parke-Davis, Karlsruhe, Germany) was purchased from the hospital pharmacy. The S-isomer of ketamine has 2–4 times greater affinity for the NMDA receptor and stronger hallucinogenic potency than the R-isomer (Øye et al, 1991, 1992; Vollenweider et al, 1997). The appropriate dosages for both DMT and S-ketamine were determined in a previous open study with six subjects (unpublished results). The low dose range was determined so as to evoke relatively subtle psychopathological alterations, below the threshold of psychotic symptoms (a so called ‘prepsychotic’ state), and the high dose range so as to evoke more profound alterations including true psychotic symptoms such as hallucinations and transient delusional misinterpretations of the experimental situation. The individual dosages were titrated during every experiment within the defined ranges so as to obtain similar intensities of psychopathological effects within the low- and high-dose regimens. Hence, the first dose was always on the maximum of the dose range of the low dose that equalled the minimum of the dose range of the high dose. The second dose was higher or lower than the first one depending on the intensity of effects during the first infusion period. This procedure enabled us to obtain psychological effects of comparable intensity within each dose regimen despite the interindividual differences in responsiveness to these drugs.
The four dose regimens were: (1) low DMT: a bolus injection of 0.15 or 0.2 mg/kg over 5 min followed by a break of 1 min, followed by continuous infusion with 0.01125 or 0.015 mg/kg min over 84 min, (2) high DMT: bolus injection of 0.2 or 0.3 mg/kg, break of 1 min and continuous infusion with 0.015 or 0.02 mg/kg min, (3) low S-ketamine: bolus injection of 0.1 or 0.15 mg/kg over 5 min, followed by a break of 1 min, followed by continuous infusion with 0.0066 or 0.01 mg/kg min over 54 min, followed by continuous infusion at a rate of 75% of the previous dose over 30 min, and (4) high S-ketamine: bolus injection of 0.15 or 0.2 mg/kg, break of 1 min, continuous infusion with 0.01 or 0.015 mg/kg min over 54 min, followed by continuous infusion at a rate of 75% of the previous dose over 30 min. The adjustment of the infusion rate of S-ketamine after 60 min was required in order to avoid a cumulation of plasma levels and gradual intensification of clinical effects. Owing to the faster elimination rate of DMT, a reduction of the DMT infusion rate over the 90 min administration period was not required. With these doses, the psychological effects of both drugs developed fully within about 15 min from the start of the injection and were then kept relatively constant over the remaining 75 min of the infusion.
Study Design and Experimental Procedures
Subjects were tested for baseline performance of orienting of attention two to seven days prior to the first experiment. Each subject participated in one experiment with DMT and one experiment with S-ketamine in a double-blind, crossover design and pseudorandomized order. The two experiments were 2–4 weeks apart. They were performed in a quiet laboratory room in the Department of Psychiatry at the University of Aachen. The subjects were instructed to take a light breakfast in the morning of the experiment and to come to the hospital between 0800 and 0900 hours. As soon as they arrived, intravenous catheters were placed in the forearm veins of both arms. During the experiment, subjects were lying comfortably in a bed with their head and upper trunk elevated. They were at all times in the company of an experienced psychiatrist and a medical student, who were both blind as to the substance used (DMT or S-ketamine). On each experiment, the low and high dose of one of the two substances (DMT or S-ketamine) were administered with a 2 h break between the two doses in a single-blind order design (see above). The drugs were administered by a second physician, who was a member of the research team and was not blind as to the substance. Therefore, she had no other role in these experiments and did not communicate with the subjects and the other members of the research team.
Drugs were administered intravenously by an automatic infusion pump (Perfusor®, B. Braun, Melsungen, Germany) between 1000 and 1130 hours and again between 1330 and 1500 hours. Cardiovascular parameters (systolic and diastolic blood pressure, heart rate) were monitored automatically (Dinamap®, Critikon Tampa, FL, USA) throughout the experiment. Between 1030 and 1130 hours and again between 1400 and 1500 hours we studied orienting of attention and the modulation of the startle reflex. Psychiatric interviews were performed in the first 30 min of each infusion, in the breaks between the assessments of orienting of attention and the modulation of the startle reflex and after termination of both infusion periods. The psychometric ratings were completed after termination of the infusion periods relating to the period during which significant psychological effects from the drugs were experienced. The SANS and SAPS data (Scale for the Assessment of Negative Symptoms and Scale for the Assessment of Positive Symptoms, Andreasen, 1984a, 1984b) are presented in this paper. A more detailed description of the psychopathological effects of DMT and S-ketamine and the startle data will be reported upon separately (Gouzoulis-Mayfrank et al, 2005b). Within 10–30 min of stopping the drug infusion, the psychological effects vanished. Blood samples for plasma levels of DMT and S-ketamine were drawn at −10, +15, +60, +90, and +150 min from the beginning of each infusion and were analyzed in the Institute of Pharmacy of the University of Tuebingen. At 1230 hours, that is, during the break between the two drug doses, subjects were served a light standardized meal. Throughout the experiment they were allowed to drink water at will. Subjects remained in the hospital under medical supervision during the break between the two doses and for at least 2 h after termination of the second dose. During that time we completed the interviews on the drug effects, and both subject and researcher completed the psychometric ratings relating to the period during which significant effects from the drugs were experienced. At discharge, subjects were instructed to contact the researcher whenever problems such as anxiety, flash back, etc. should occur during the following days. On the day after the experiment all subjects were interviewed on possible delayed effects. In addition, 7 days and 10–12 months after the experiments, we carried out semistructured interviews with all subjects on possible delayed effects, psychological well-being, and substance use.
Stimulus Materials and Procedures
Subjects were tested with the same two versions of the COVAT (one version with endogenous and one version with exogenous cues) on the baseline and on the two experimental days. Stimuli were presented on a Toshiba 740CDT laptop. Stimulus presentation and data collection were controlled by the program ERTS (Experimental Run Time System, BeriSoft Cooperation Frankfurt). During performance of the task, subjects were seated about 60 cm in front of the computer monitor and were instructed to maintain fixation on a centrally presented cross. The task was to respond as rapidly as possible to the target by pressing a single key with the index finger of the dominant hand, which was allowed to rest on the key in anticipation of making a response. The target was a star, which appeared on each trial within one of the two peripheral square boxes at about 5° right or left from the central fixation cross, and remained present for 300 ms. Recordings of the electrooculogram (EOG) were used in order to control for eye movements. The two electrodes for the vertical channel were placed above and below the left eye and the two for the horizontal channel were placed on the outer canthi of the left and right eye. The EOG data were recorded digitally using a 50 Hz low-pass and a 0.3 Hz high-pass filter (Synamps, Neuroscan). The EOG data were marked by trigger signals from the COVAT task. This enabled us to reject single trials with eye movement artefacts and exclude them from further analyses. A practice experiment consisting of 24 trials was performed prior to each session with no RTs recorded.
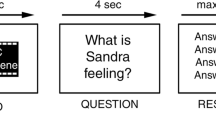
COVAT with exogenous cues (schematic presentation in Figure 1)
In this task, three identical boxes were presented on the screen throughout the experiment: one box in the center of the screen with the fixation point in it, and the two peripheral boxes. The experiment consisted of 192 trials. Out of these trials, 32 were uncued: In these no-cue trials, the target occurred in the center of the left or the right box with equal probability following an interval of 1100 ms after the previous key press. In another 32 trials, only the central box was brightened (spatially neutral cue), and the target followed either in the right or in the left box either 100 or 800 ms after cue onset with equal probability (stimulus onset asynchrony: SOA 100 or 800 ms). In the remaining 128 trials, either the right or the left box was brightened with equal probability, and the target followed either 100 or 800 ms after cue onset either in the brightened box or opposite to the brightened box (valid or invalid cue) with equal probability. In cued trials, the cue appeared following an interval of 1000 ms after the previous key press (intertrial interval) and remained present for the duration of 100 ms. If the subject missed to response to a target, the next trial started automatically 2000 ms after offset of the target from the previous trial.
COVAT with endogenous cues (schematic presentation in Figure 2)
In this task, only the two peripheral boxes were presented on the screen. Instead of the central box, two arrows right and left from and very close to the central fixation point were presented, the right arrow indicating towards the right and the left arrow towards the left peripheral box. Again, the experiment consisted of 192 trials and 32 trials were uncued. In the 32 trials with a spatially neutral cue, both arrows were brightened and the target followed either in the right or in the left box either 200 ms or 800 ms after cue onset with equal probability (stimulus onset asynchrony: SOA 200 ms or 800 ms). In the remaining 128 trials, either the right or the left arrow was brightened with equal probability, and the target followed either 200 or 800 ms after cue onset with equal probability, either in the indicated box or opposite to the indicated box (valid or invalid cue) with a probability of 78.125–21.875% (25 valid: 7 invalid).
Data Analysis
Trials with RTs less than 100 ms or exceeding 1000 ms were excluded, because they were considered either anticipatory or most likely to be due to brief periods of general inattention to the task. Trials with eye movements registered in the EOG were also excluded. Median RT values of the remaining trials were calculated for each subject, drug condition, and type of trial. Group performances were calculated as mean values of these data. In order to obtain a measure for the global response readiness, we initially analyzed RTs in the no-cue trials separately by means of repeated measures ANOVAs with the factor drug (baseline, DMT low, DMT high, S-ketamine (KET) low, KET high) and visual field in which the target appeared (visual field (VF)). Thereafter, we analyzed the RTs in cued trials by means of repeated measures ANOVAs with the factors drug, cue (double, invalid, valid), stimulus onset asynchrony (SOA), and VF.
Subsequently, we calculated validity effects by subtracting the median RT of the valid from the median RT of the invalid trials for every subject and type of trial (validity effect in ms: RTinvalid−RTvalid). Similarly, we calculated alertness effects by subtracting the median RT of trials with a neutral cue from the median RT of no-cue trials (alertness effect in ms: RTno-cue−RTdouble cue, reflects the generally higher response readiness after cues, irrespective of their spatial information). Alertness and validity effects were analyzed by means of repeated measures ANOVAs with the factors drug, SOA, and VF. Validity effects for the COVAT with exogenous cues were analyzed separately for the short and long SOA using only the factors drug and VF, because these validity effects reflect different mechanisms (reorienting with the short SOA vs IOR with the long SOA).
Pearson's correlation coefficients were employed to explore the relationship between alertness and validity effects and psychopathological symptoms (total and subscale scores of the SANS and the SAPS; Andreasen, 1984a, 1984b). All statistical procedures were performed using SPSS software (version 11.0). P-values ⩽0.05 were considered significant, except for the correlation analyses, where the significance level was adjusted following Bonferroni correction in order to avoid accumulation of type-I error due to multiple correlations.
RESULTS
From the 15 subjects who entered the study, 12 subjects completed the experiment with both doses of DMT and 10 subjects completed the experiment with both doses of S-ketamine. Dropouts were due to unpleasant psychological effects (two subjects under S-ketamine, one subject under DMT), nausea (one subject under DMT), hypotonia (one subject under DMT), and headache and mild orthostatic complaints (one subject on the day following an experiment with DMT). In all dropout cases, undesirable effects were self-limited and required no additional medication. The interviews conducted 7 days and 10–12 months after the experiments revealed no aspects of psychopathology or substance abuse that might be related to participation in our study. Both drugs dose-dependently induced psychotic symptoms similar to schizophrenic manifestations.
The global and subscale scores of the Scale for the Assessment of Negative Symptoms SANS and the Scale for the Assessment of Positive Symptoms SAPS (Andreasen, 1984a, 1984b) are presented in Table 1. Phenomena resembling positive symptoms of schizophrenia, particularly positive formal thought disorder and inappropriate affect, were stronger after DMT. Phenomena resembling negative symptoms of schizophrenia and attentional deficits were stronger after S-ketamine. Plasma levels for both substances showed little variation between +60 and +90 min after start of infusion and a fast decline after termination of the infusion. Details on psychopathological effects, after-effects, and plasma levels are presented in Gouzoulis-Mayfrank et al (2005b).
Nine subjects completed both experiments with both doses of DMT and S-ketamine. Data are reported for these nine subjects. The order of dosages was first low, then high in eight and first high, then low in 10 out of the 18 experiments. For the task with exogenous cues, the mean percentage of excluded trials for baseline was 0.64% for too fast (<100 ms) and/or too slow (>1000 ms) or missing responses and 5.93% for eye movements recorded by EOG. For DMT low, these percentages were 0.81 and 13.43%, for DMT high 1.27 and 18.58%, for S-ketamine (KET) low 0.64 and 6.66%, and for KET high 0.52 and 3.30%, respectively. For the task with endogenous cues, the mean percentage of excluded trials for baseline was 0.58% for too fast and/or too slow or missing responses and 6.12% for eye movements. These percentages were 0.87 and 14.35% for DMT low, 2.72 and 16.73% for DMT high, 1.33 and 6.67% for KET low, and 1.39 and 2.03%, respectively, for KET high.
COVAT with Exogenous Cues
RTs are presented in Figure 3. No-cue trials: In the repeated measures ANOVA for the RTs in the no-cue trials, we found a significant main effect of the drug (F=7.989, p<0.05), but no effect of VF and no interaction. The post hoc tests revealed significant differences between baseline and both DMT doses as well as the KET high dose. In addition, DMT low was significantly different from KET low, and DMT high was different from both KET low and KET high. Hence, both drugs dose-dependently prolonged global RTs, this effect being more pronounced after DMT, while the low KET dose was not significantly different from baseline. Cued trials: In the repeated measures ANOVA for the RTs in the cued trials, we found significant main effects of drug (F=17.733, p<0.01) and SOA (F=33.334, p<0.0001). Again, we found no significant effect of VF, and also the effect of cue failed significance (p=0.12). However, we found a significant interaction SOA × cue (F=23.625, p<0.001), and a marginal interaction drug × SOA × cue (F=223.659, p=0.052). All other interactions and higher order interactions were insignificant. The post hoc tests revealed significant differences between baseline and both DMT doses as well as the KET high dose. In addition, DMT low was significantly different from KET low, DMT high was different from KET low, and KET high was different from KET low. Inspection of the descriptive data suggests a smaller amount of IOR after both drugs and, in addition, reversed validity effects for right VF targets with the short SOA of 100 ms after the low KET and the high DMT dose.
Reaction times (RTs) in ms in the covert orienting of attention task (COVAT) with exogenous cues (n=9, group means). SOA, stimulus onset asynchrony=time from onset of cue to onset of target; filled symbols, target in right visual field; open symbols, target in left visual field; No, no-cue trial, N, neutral cue trial; V, valid trial; I, invalid trial.
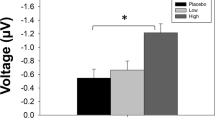
To further analyze these effects, we performed analyses of validity and alertness effects. Validity effects (Figure 4): In the repeated measures ANOVA of the validity effects for the short SOA (reorienting), we found a significant main effect of drug (F=5.595, p<0.05), but no effect of VF and no interaction. Post hoc tests revealed significant differences between DMT high and the other three drug conditions (DMT low, KET high, and KET low). However, the difference between DMT high and baseline failed significance (p=0.062), and, otherwise, baseline was not different from the other drug conditions (p-values >0.2). These results indicate high variance in the data, but they clearly do not support a deficit in disengagement of attention from previously cued locations. If any, there is rather tentative support for an inverse validity effect after DMT, reflecting abnormal facilitation of reorienting in favor of targets in the right VF. In the repeated measures ANOVA of the validity effects for the long SOA, which reflect IOR, we also found a significant main effect of drug (F=10.848, p<0.05), no effect of VF, and no interaction. Post hoc tests revealed significant differences between baseline and both DMT dosages as well as baseline and KET low. The difference between baseline and KET high failed significance (p=0.14). There was no significant difference between DMT and KET in either dose (p-values >0.5). These results support a deficit of IOR with both hallucinogens, but more clearly so with DMT. Alertness effects: In the repeated measures ANOVA of the alertness effects, we found only a significant main effect of SOA (F=61.915, p<0.001), reflecting a response facilitation with the long SOA. Otherwise, no main effects or interactions reached statistical significance. Hence, the general alerting effect of spatially uninformative exogenous cues was similar for baseline and the hallucinogenic drug conditions. Interestingly, we found no facilitating effect of neutral cues with the short SOA. In the contrary, RTs in trials with spatially neutral cues were tentatively longer than RTs in no-cue trials. A possible explanation for this unexpected finding might be that the centrally located cue, which was supposed to be spatially neutral, still summoned attention automatically to the central area of the screen, thus acting as an invalid cue.
COVAT with Endogenous Cues
RTs are presented in Figure 5. No-cue trials: In the repeated measures ANOVA for the RTs in the no-cue trials, we found no significant main effects and no interactions. Hence, in this version of the COVAT, the two hallucinogens did not prolong global RTs. Cued trials: In the repeated measures ANOVA for the RTs in the cued trials, we found significant main effects of SOA (F=20.111, p<0.01) and cue (F=27.949, p<0.0001), but not of the VF. The effect of drug failed significance (F=4.622, p=0.062). Also, we found a marginal interaction drug × SOA (F=4.302, p=0.071). The post hoc tests revealed significant differences between baseline and both DMT dosages, but not between baseline and KET. In addition, DMT low was significantly different from both KET doses, DMT high was different from KET low, and KET high was different from KET low. Additional post hoc tests revealed significant differences between all three cue conditions. Again, in order to further analyze the general alerting and the spatially orienting effects of cues, we performed analyses of alertness and validity effects. Validity effects: In the repeated measures ANOVA of the validity effects, we found no significant main effects and no significant interactions. Alertness effects (Figure 6): We found significant main effects of drug (F=81.962, p<0.0001) and SOA (F=21.760, p<0.01), but no effect of VF and no significant interactions. The post hoc tests revealed significant differences between DMT high and baseline as well as all other drug conditions. Hence, the general alerting effect of spatially neutral cues was diminished after the high dose of DMT.
Reaction times (RTs) in ms in the covert orienting of attention task (COVAT) with endogenous cues (n=9, group means). SOA, stimulus onset asynchrony=time from onset of cue to onset of target; filled symbols, target in right visual field; open symbols, target in left visual field; No, no-cue trial; N, neutral cue trial; V, valid trial; I, invalid trial.
Correlations with Psychopathological Symptoms
Pearson's correlation coefficients were employed to explore the relationship between psychopathological symptoms (global and subscale scores of the SANS and SAPS, Andreasen, 1984a, 1984b) and blunted IOR (validity effects at the long SOA in the COVAT with peripheral cues) after both drugs and doses as well as alertness effects after the high dose of DMT. Only one correlation passed a conservative Bonferroni corrected significance level indicating a larger validity effect (ie higher deficit of IOR) for targets in the left visual field with more hallucinations (SAPS subscale score) with the low DMT dose (r=0.952; p<0.0001).
DISCUSSION
The aim of the present investigation was to study spatial orienting of attention in two different pharmacological models of psychosis in humans. We administered two doses of the serotonergic hallucinogen DMT and the antiglutamatergic hallucinogen S-ketamine to healthy volunteers in a randomized, double-blind, crossover experimental design. Overall, most subjects tolerated the procedures and we observed no serious delayed adverse effects after the experiments. In those cases where we stopped drug administration and terminated the experiment because of intense, unpleasant psychological or adverse physical effects, all undesirable phenomena faded rapidly and were never followed by lasting sequelae. Hence, although the participation in this study has been stressful, the level of distress for the subjects has been acceptable.
The administration of both hallucinogens was followed by dose-dependent, powerful alterations of perception, affect and cognition, which were similar to many typical symptoms of patients with schizophrenia. The overall intensity of the hallucinogenic effects of both drugs was similar, however, phenomena that resemble positive symptoms of schizophrenia were more pronounced after DMT and phenomena that resemble negative and motor (catatonic) symptoms of schizophrenia were clearly more pronounced after S-ketamine. Similarly, cognitive problems such as difficulties with concentration and short-term memory appeared to be more pronounced after S-ketamine (for a more detailed description of psychopathological effects, see Gouzoulis-Mayfrank et al, 2005b). Taken together, the data from the present study are in line with the view that the NMDA antagonist state (ketamine) is a model for undifferentiated or disorganized psychoses with both positive and negative symptoms, while the 5-HT2A agonist state (DMT) is an appropriate model for psychoses with prominent positive symptoms (Javitt and Zukin, 1991; Krystal et al, 1994; Abi-Saab et al, 1998).
The baseline performance data reflect the usual response facilitation in trials with spatially neutral cues over uncued trials (alerting effect), the general response facilitation with longer SOAs (also a consequence of increased preparedness to respond to the target), the disadvantage of invalid over valid trials with endogenous cues and with exogenous cues and short SOAs (reorienting), and, finally, the disadvantage of valid over invalid trials with exogenous cues and long SOAs (Inhibition of Return=IOR). Both hallucinogens dose-dependently slowed down RTs, however, this unspecific effect on general response readiness was more pronounced after DMT and passed the significance level only with the high dose of S-ketamine. In addition, the facilitatory effect of spatially neutral cues was diminished after the high dose of DMT, but not after S-ketamine. Hence, although subjects under S-ketamine displayed more pronounced psychomotor poverty, general retardation and passive behavior gave the impression of being more cognitively disturbed in terms of their ability to concentrate (Gouzoulis-Mayfrank et al, 2005b), their general response readiness in a psychomotor task, and their ability to utilize spatially neutral, alerting cues seemed to be relatively intact compared to the state elicited by DMT.
In respect to spatial orienting, we found no evidence for a deficit in disengaging attention from previously cued locations after both hallucinogens and with both versions of the COVAT. The variance in the reorienting data has been particularly large. However, in any, the findings provide limited support for an abnormal facilitation, rather than a deficit in reorienting after the high dose of DMT and exogenous cueing. This finding is reminiscent of a similar effect showed by Nestor et al (1992) and Oie et al (1998) in patients with schizophrenia. However, the difference between DMT and baseline failed significance. Therefore, we abstain from further interpretations of these data.
The clearest finding in our study was a blunting of IOR after exogenous cueing and a long cue target interval of 800 ms after both doses of DMT and the low dose of S-ketamine. The difference between the high S-ketamine dose and baseline failed significance, although the amount of IOR tended to be smaller also with the high S-ketamine dose. Given the normal alerting effects of exogenous neutral cues with the long cue target interval after both drugs, the finding of deficient IOR cannot be explained by some general deficit in the processing or memory trace of cues. Hence, the most plausible interpretation of our data is a specific abnormality of the automatic, reflexive mechanisms of orienting underlying IOR. This abnormality seems to be more pronounced or more robust in the serotonin (DMT) model, which is a model for psychoses with prominent positive symptoms. In addition, results from the correlation analyses support an association of blunted IOR with positive symptoms, specifically hallucinations, in the DMT model.
Our study is the first direct comparison of a serotonergic and an antiglutamatergic hallucinogen in a double-blind, within-subject experimental design. However, this study has methodological limitations that have to be acknowledged: Most importantly, the sample size was small for completers. Hence, lack of significant differences between the different drug conditions might be due to lack of statistical power. Moreover, the use of psychiatric staff (mostly academics) as experimental subjects may well bear the risk of significant biases in the data. On the other hand, it is difficult to plan and obtain permissions for human experimental studies with hallucinogens, and the recruitment of suitable experimental subjects is a sensitive issue. Therefore, it would be rather unrealistic to plan studies with larger samples, and also, different samples of volunteers who are not professionals in the psychiatric field would be likely to have their own biases (are people who volunteer to participate in such studies representative, ‘average’ subjects?). Furthermore, the absence of a placebo condition is a further limitation that we decided to accept due to practical considerations: The fact that we would have needed a third experimental day for the placebo condition would have been critical for the recruitment of volunteers for our study. This problem is very significant because our subjects were full time professionals who had to take time from work to take part in our experiments without payment. Nevertheless, placebo-controlled hallucinogen experiments have their own methodological problems, because the effects of hallucinogens are so prominent that blinding is not really possible (Gouzoulis-Mayfrank et al, 1998b). Therefore, we decided that, on balance, it was reasonable and acceptable to omit the placebo condition and use baseline data instead.
Our data are in line with the findings from previous studies reporting delayed or blunted IOR in patients with schizophrenia (Huey and Wexler, 1994; Carter et al, 1994; Sapir et al, 2001; Larrison-Faucher et al, 2002; Gouzoulis-Mayfrank et al, 2004, 2005a). Interestingly, one of these studies demonstrated blunted IOR only in patients with paranoid, but not in patients with the undifferentiated subtype of schizophrenia (Carter et al, 1994). Again, this finding is in line with our data, which suggest a more robust IOR deficit with the serotonin, rather than the NMDA antagonist model of psychosis. Nevertheless, four studies using appropriate tasks with exogenous, nonpredictive cues reported normal IOR in patients with schizophrenia (Carter et al, 1992; Maruff et al, 1998; Fuentes and Santiago, 1999; Fuentes et al, 1999). However, again, two out of these four negative studies used a ‘cue-back’ manipulation (Fuentes and Santiago, 1999; Fuentes et al, 1999), where a second cue draws attention back to the central fixation point shortly after the first cue and prior to the appearance of the target. This ‘cue-back’ manipulation is known to enhance or speed up the course of IOR and may have acted to reinstate a subtle IOR deficit in this patient population. This interpretation is in line with a study by Sapir et al (2001) who used both a single cue and a cue-back paradigm in the same patient sample and reported absence of IOR in the single cue, but normal IOR in the cue-back paradigm.
In conclusion, IOR seems to be deficient in naturally occurring and in experimental psychoses. Accordingly, deficient IOR might reflect a fundamental cognitive mechanism in psychotic disturbances. However, the IOR deficit seems to be more pronounced in psychoses with prominent positive symptoms. This finding leads to a question about the physiological significance of IOR and the significance of the IOR deficit in psychosis. The physiological significance of the advantage of valid over invalid trials with peripheral cues and short cue target intervals is intuitively clear as being due to an automatic shift of attention towards the direction of stimulation by the cue. In contrast, and despite extensive research, the phenomenon of IOR, that is, the RT disadvantage for trials with valid, peripheral cues and long SOAs, is not entirely understood. Posner and co-workers (Posner and Cohen, 1984; Posner et al, 1985) favored an inhibitory, attentional mechanism that protects the organism from redirecting attention to previously scanned, insignificant locations, thus preventing perseveration and making searching operations more effective. However, alternative interpretations of IOR include a sensory mechanism related to sensory masking or habituation and a motor bias against making responses to targets that appear in a previously cued location (Taylor and Klein, 1998). The prevailing theory has been the one of an automatic, that is, reflexive, inhibitory attentional mechanism (reviewed in Klein, 2000), although recent studies support a combined attentional and motor basis of IOR (Klein and Dick, 2002; Lepsien and Pollmann, 2002).
With regard to the attentional interpretation of IOR, its deficit in patients with schizophrenia might result in overprocessing of redundant stimuli and a bias towards preservation errors. Furthermore, one might expect that patients could be more easily distracted by irrelevant stimuli from the environment. This, in turn, might result in overstimulation and difficulties to sustain internally driven directed attention. Finally, these abnormalities in information processing might contribute to what has been termed ‘cognitive fragmentation’ (Braff et al, 1992) and the formation of positive psychotic symptoms. Clearly, this interpretation is speculative. However, it appeals intuitively, and it receives some support by a report of associations between low IOR and high distractibility in patients with schizophrenia (Karper et al, 1996). In addition, this interpretation is in line with our experimental data of the IOR being blunted already with the low doses of both DMT and S-ketamine, which elicited mostly ‘prepsychotic’ symptoms and being associated with a higher amount of positive symptoms such as hallucinations.
Clearly, IOR is closely linked to oculomotor programming, and evidence from animal and human lesion studies suggests that the superior colliculus (SC) is crucial for the generation of IOR (Sapir et al, 1999; Klein, 2000; Fecteau et al, 2004). However, recent functional neuroimaging studies demonstrate an involvement of frontal premotor (oculomotor) and parietal areas, the cerebellum, and the ventrolateral nucleus of the thalamus in IOR (Rosen et al, 1999; Lepsien and Pollmann, 2002; Mayer et al, 2004a, 2004b). Undoubtedly, both oculomotor abnormalities and frontal cortex dysfunction belong to the most robust findings of biological schizophrenia research (Holzman, 1985; Sereno and Holzman, 1995; Arolt et al, 1998; Weinberger et al, 1986, 2001). More recently, abnormalities of thalamic and cerebellar function and abnormalities in the functional interplay between different areas such as the prefrontal and temporolimbic cortex, the thalamus, basal ganglia, and the cerebellum (‘disconnectivity’) have also been suggested as indicative of the schizophrenic disorder (Andreasen et al, 1998; Meyer-Lindenberg et al, 2001; Schlosser et al, 2003; Ragland et al, 2004; Hulshoff Pol et al, 2004). Hence, disturbed function in both cortical and subcortical areas and their interconnections may be associated with deficits of IOR in patients with schizophrenia.
In conclusion, the main finding of our study is a deficit of IOR both in the serotonin (LSD-type) and the NMDA antagonist (PCP type) model of psychosis, with the effect being clearer in the serotonin model. This finding is in line with reports on deficient IOR in patients with schizophrenia and specifically with one report on blunted IOR in paranoid, but not in undifferentiated patients (Carter et al, 1994). Deficient IOR might be viewed as a state marker, or, alternatively, as a vulnerability factor for psychoses with prominent positive symptoms. Future studies with schizotypal, prodromal, or genetic high-risk subjects should help to clarify the questions on the significance of blunted IOR in schizophrenia and spectrum disorders.
References
Abi-Saab WM, D'Souza DC, Moghaddam B, Krystal JH (1998). The NMDA antagonist model for schizophrenia: promise and pitfalls. Pharmacopsychiatry 31S: 104–109.
Addington J, Addington D (1998). Visual attention and symptoms in schizophrenia: a 1-year follow-up. Schizophrenia Res 34: 95–99.
American Psychiatric Association (APA) (1994). DSM-IV: Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Press, Inc.: Washington, DC.
Andreasen NC (1984a). The scale for the assessment of negative symptoms (SANS). Department of Psychiatry, University of Iowa, Iowa City, Copyright by Andreasen NC, 1984.
Andreasen NC (1984b). The scale for the assessment of positive symptoms (SAPS). Department of Psychiatry, University of Iowa, Iowa City, Copyright by Andreasen NC, 1984.
Andreasen NC, Paradiso S, O'Leary DS (1998). ‘Cognitive dysmetria’ as an integrative theory of schizophrenia: a dysfunction in cortical–subcortical–cerebellar circuitry? Schizophrenia Bull 24: 203–218.
Arolt V, Teichert HM, Steege D, Lencer R, Heide W (1998). Distinguishing schizophrenic patients from healthy controls by quantitative measurement of eye movement parameters. Biol Psychiatry 44: 448–458.
Braff DL, Grillon C, Geyer MA (1992). Gating and habituation of the startle reflex in schizophrenic patients. Arch Gen Psychiatry 49: 206–215.
Carpenter WT (1999). The schizophrenia ketamine challenge study debate. Biol Psychiatry 46: 1081–1091.
Carter CS, Robertson LC, Chaderjian MR, Celaya LJ, Nordahl TE (1992). Attentional asymmetry in schizophrenia: controlled and automatic processes. Biol Psychiatry 31: 909–918.
Carter CS, Robertson LC, Chaderjian MR, O'Shora-Celaya L, Nordahl TE (1994). Attentional asymmetry in schizophrenia: the role of illness subtype and symptomatology. Progr Neuropsychopharmacol Biol Psychiatry 18: 661–683.
D'Souza DC, Berman RM, Krystal JH, Charney DS (1999). Symptom provocation studies in psychiatric disorders: scientific value, risks, and future. Biol Psychiatry 46: 1060–1080.
Fecteau JH, Bell AH, Munoz DP (2004). Neural correlates of the automatic and goal-driven biases in orienting spatial attention. J Neurophysiology 92: 1728–1737.
Fuentes LJ, Boucart M, Alvarez R, Vivas AB, Zimmerman MA (1999). Inhibitory processing in visuospatial attention in healthy adults and schizophrenic patients. Schizophrenia Res 40: 75–80.
Fuentes LJ, Santiago E (1999). Spatial and semantic inhibitory processing in schizophrenia. Neuropsychology 13: 259–270.
Gold JM, Randolph C, Coppola R, Carpenter CJ, Goldberg TE, Weinberger DR (1992). Visual orienting in schizophrenia. Schizophrenia Res 7: 203–209.
Gouzoulis-Mayfrank E, Arnold S, Heekeren K (2005a). Deficient inhibition of return in schizophrenia—further evidence from an independent sample. Prog Neuropsychopharmacol Biol Psychiatry, in press, corrected proof, available online 12 July 2005.
Gouzoulis-Mayfrank E, Heekeren K, Timmerbeil A, Stoll M, Stock C, Obradovic M et al (2005b). Psychological effects of S-ketamine and N,N-dimethyltryptamine (DMT): a double-blind, cross-over study in healthy volunteers. Pharmacopsychiatry, in press.
Gouzoulis-Mayfrank E, Heekeren K, Voss T, Moerth D, Thelen B, Meincke U (2004). Blunted inhibion of return (IOR)—a trait marker of schizophrenia? Prog Neuro-Psychopharmacol Biol Psychiatry 28: 389–396.
Gouzoulis-Mayfrank E, Hermle L, Thelen B, Sass H (1998a). History, rationale and potential of experimental hallucinogenic drug research in psychiatry. Pharmacopsychiatry 31(S2): 63–68.
Gouzoulis-Mayfrank E, Schneider F, Spitzer M, Thelen B, Sass H (1998b). Methodological issues of human experimental research with hallucinogens. Pharmacopsychiatry 31(S2): 114–118.
Gouzoulis-Mayfrank E, Schreckenberger M, Sabri O, Arning C, Thelen B, Spitzer M et al (1999a). Neurometabolic effects of psilocybin, 3,4-methylenedioxyethylamphetamine (MDE) and d-methamphetamine in healthy volunteers. A double-blind, placebo-controlled PET study with [18F]FDG. Neuropsychopharmacology 20: 565–581.
Gouzoulis-Mayfrank E, Thelen B, Habermeyer E, Kunert HJ, Kovar KA, Hermle L et al (1999b). Psychopathological, neuroendocrine and autonomic effects of 3,4-methylenedioxyethylamphetamine (MDE), psilocybin and d-methamphetamine in healthy volunteers. Results of an experimental double-blind placebo-controlled study. Psychopharmacology 142: 41–50.
Gouzoulis-Mayfrank E, Thelen B, Maier S, Habermeyer E, Kovar K-A, Sass H et al (2002). Effects of the hallucinogen psilocybin on covert orienting of visual attention in humans. Neuropsychobiology 45: 205–212.
Holzman PS (1985). Eye movement dysfunctions and psychosis. Int Rev Neurobiol 27: 179–205.
Huey ED, Wexler BE (1994). Abnormalities in rapid, automatic aspects of attention in schizophrenia: blunted inhibition of return. Schizophrenia Res 14: 57–63.
Hulshoff Pol HE, Schnack HG, Mandl RC, Cahn W, Collins DL, Evans AC et al (2004). Focal white matter density changes in schizophrenia: reduced inter-hemispheric connectivity. Neuroimage 21: 27–35.
Javitt DC, Zukin SR (1991). Recent advances in the phencyclidine model of schizophrenia. Am J Psychiatry 148: 1301–1308.
Karper LP, Freeman G, Grillon C, Morgan III CA, Charney DS, Krystal JH (1996). Preliminary evidence of an association between sensorimotor gating and distractibility in psychosis. J Neuropsych Clin Neurosci 8: 60–66.
Klein RM (2000). Inhibition of return. Trends Cogn Sci 4: 138–147.
Klein RM, Dick B (2002). Temporal dynamics of reflexive attention shifts: a dual-stream rapid serial visual presentation exploration. Psychol Sci 13: 176–179.
Krystal JH, Karper LP, Seibyl JP, Freeman GK, Delaney R, Bremner JD et al (1994). Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry 51: 199–214.
Larrison-Faucher A, Briand KA, Sereno AB (2002). Delayed onset of inhibition of return in schizophrenia. Progr Neuropsychopharmacol Biol Psychiatry 26: 505–512.
Lepsien J, Pollmann S (2002). Covert reorienting and inhibition of return: an event-related fMRI study. J Cogn Neurosci 14: 127–144.
Liotti M, Dazzi S, Umilta C (1993). Deficits of the automatic orienting of attention in schizophrenic patients. J Psychiatr Res 27: 119–130.
Maruff P, Danckert J, Pantelis C, Currie J (1998). Saccadic and attentional abnormalities in patients with schizophrenia. Psychol Med 28: 1091–1100.
Maruff P, Hay D, Malone V, Currie J (1995). Asymmetries in the covert orienting of visual spatial attention in schizophrenia. Neuropsychologia 33: 1205–1223.
Mayer AR, Dorflinger JM, Rao SM, Seidenberg M (2004a). Neural networks underlying endogenous and exogenous visual-spatial orienting. Neuroimage 23: 534–541.
Mayer AR, Seidenberg M, Dorflinger JM, Rao SM (2004b). An event-related fMRI study of exogenous orienting: supporting evidence for the cortical basis of inhibition of return? J Cogn Neurosci 16: 1262–1271.
Meyer-Lindenberg A, Poline JB, Kohn PD, Holt JL, Egan MF, Weinberger DR et al (2001). Evidence for abnormal cortical functional connectivity during working memory in schizophrenia. Am J Psychiatry 158: 1809–1817.
Nestor PG, Faux SF, McCarley RW, Penhune V, Shenton ME, Pollak S et al (1992). Attentional cues in chronic schizophrenia: abnormal disengagement of attention. J Abnormal Psychol 101: 682–689.
Oie M, Rund BR, Sundet K (1998). Covert visual attention in patients with early-onset schizophrenia. Schizophrenia Res 34: 195–205.
Øye N, Hustveit O, Moberg ER, Pausen O, Skoglund LA (1991). The chiral forms of ketamine as probes for NMDA receptor function in humans. In: Kameyama T, Nabeshima T, Domino ES (eds). NMDA Receptor Related Agents: Biochemistry, Pharmacology and Behavior. NPP Books: Ann Arbor. pp 381–389.
Øye N, Paulsen O, Maurset A (1992). Effects of ketamine on sensory perception: evidence for a roel of N-methyl-D-aspartate receptors. J Pharmacol Exp Therap 260: 1209–1213.
Posner MI, Cohen Y (1984). Components of visual orienting. In: Bouma H, Bouwhuis DG (eds). Attention and Performance. Control of Language Processing. Lawrence Erlbaum Associates Publishers: London. pp 531–556.
Posner MI, Early TS, Reiman E, Pardo PJ, Dhawan M (1988). Asymmetries in hemispheric control of attention in schizophrenia. Arch Gen Psychiatry 45: 814–821.
Posner MI, Rafal R, Choate LS, Vaughan J (1985). Inhibition of Return: neural basis and function. Cogn Neuropsychology 2: 211–228.
Potkin SG, Swanson JM, Urbaneck M, Carreon D, Bravo G (1989). Lateralized deficits in covert shifts of visual attention in chronic and never-medicated schizophrenics compared to normal controls. Schizophrenia Res 2: 95.
Ragland JD, Gur RC, Valdez J, Turetsky BI, Elliott M, Kohler C et al (2004). Event-related fMRI of frontotemporal activity during word encoding and recognition in schizophrenia. Am J Psychiatry 161: 1004–1015.
Rosen AC, Rao SM, Caffarra P, Scaglioni A, Bobholz JA, Woodley SJ et al (1999). Neural basis of endogenous and exogenous spatial orienting. A functional MRI study. J Cogn Neurosci 11: 135–152.
Sapir A, Henik A, Dobrusin M, Hochman EY (2001). Attentional asymmetry in schizophrenia: disengagement and inhibition of return deficits. Neuropsychology 15: 361–370.
Sapir A, Soroker N, Berger A, Henik A (1999). Inhibition of return in spatial attention: direct evidence for collicular generation. Nat Neurosci 2: 1053–1054.
Schlosser R, Gesierich T, Kaufmann B, Vucurevic G, Hunsche S, Gawehn J et al (2003). Altered effective connectivity during working memory performance in schizophrenia: a study with fMRI and structural equation modeling. Neuroimage 19: 751–763.
Sereno AB, Holzman PS (1995). Antisaccades and smooth pursuit eye movements in schizophrenia. Biol Psychiatry 37: 394–401.
Snyder SH (1988). Psychotogenic drugs as models for schizophrenia. Neuropsychopharmacology 1: 197–199.
Strauss ME, Alphs L, Boekamp J (1992). Disengagement of attention in chronic schizophrenia. Psychiatry Res 43: 87–92.
Strauss ME, Novakovic T, Tien AY, Bylsma F, Pearlson GD (1991). Disengagement of attention in schizophrenia. Schizophrenia Res 37: 139–146.
Taylor TL, Klein RM (1998). On the causes and effects of inhibition of return. Psychon Bull Rev 5: 625–643.
Vollenweider FX, Antonini A, Leenders KL, Oye I, Hell D, Angst J (1997). Differential psychopathology and patterns of cerebral glucose utilisation produced by (S)- and (R)-ketamine in healthy volunteers using positron emission tomography (PET). Eur Neuropsychopharmacol 7: 25–38.
Weinberger DR, Berman KF, Zec RF (1986). Physiologic dysfunction of dorsolateral prefrontal cortex in schizophrenia. I. Regional cerebral blood flow evidence. Arch Gen Psychiatry 43: 114–124.
Weinberger DR, Egan MF, Bertolino A, Callicott JH, Mattay VS, Lipska BK et al (2001). Prefrontal neurons and the genetics of schizophrenia. Biol Psychiatry 50: 825–844.
Wigal SB, Swanson JM, Potkin SG (1997). Lateralized attentional deficits in drug-free and medicated schizophrenic patients. Neuropsychologia 35: 1519–1525.
Acknowledgements
This work was supported by a grant to the first author from the German Research Foundation (Deutsche Forschungsgemeinschaft DFG, Project No. 6 of a DFG clinical researcher group KFO 112/1/-1, Go 717/5-1). The paper includes parts of the doctoral thesis of the third author (AN) at the University Hospital Aachen.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gouzoulis-Mayfrank, E., Heekeren, K., Neukirch, A. et al. Inhibition of Return in the Human 5HT2A Agonist and NMDA Antagonist Model of Psychosis. Neuropsychopharmacol 31, 431–441 (2006). https://doi.org/10.1038/sj.npp.1300882
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300882
Keywords
This article is cited by
-
Impaired inhibition of return during free-viewing behaviour in patients with schizophrenia
Scientific Reports (2021)
-
Double-blind comparison of the two hallucinogens psilocybin and dextromethorphan: effects on cognition
Psychopharmacology (2018)
-
Persistent effects of chronic clozapine on the cellular and behavioral responses to LSD in mice
Psychopharmacology (2013)
-
Acute effects of ayahuasca on neuropsychological performance: differences in executive function between experienced and occasional users
Psychopharmacology (2013)
-
Psilocybin-Induced Deficits in Automatic and Controlled Inhibition are Attenuated by Ketanserin in Healthy Human Volunteers
Neuropsychopharmacology (2012)