Abstract
Tumor hypoxia negatively regulates cell growth and causes a more malignant phenotype by increasing the expression of genes encoding angiogenic, metabolic and metastatic factors. Of clinical importance, insufficient tumor oxygenation affects the efficiency of chemotherapy and radiotherapy by poorly understood mechanisms. The hypoxia-inducible factor (HIF)-1 is a master transcriptional activator of oxygen-regulated genes and HIF-1 is constitutively upregulated in several tumor types. HIF-1 might thus be implicated in tumor therapy resistance. We found that transformed mouse embryonic fibroblasts deficient for HIF-1α are more susceptible to the treatment with carboplatin, etoposide and ionizing radiation than wild-type cells. Increased cell death in HIF-1α-deficient cells was because of apoptosis and did not involve p53 induction. Tumor chemotherapy of experimental fibrosarcoma in immunocompromised mice with carboplatin and etoposide confirmed the enhanced susceptibility of HIF-1α-deficient cells. Agents that did not cause DNA double-strand breaks, such as DNA-synthesis inhibitors or a DNA single-strand break-causing agent equally impaired cell growth, independent of the HIF-1α genotype. Functional repair of a fragmented reporter gene was decreased in HIF-1α-deficient cells. Thus, hypoxia-independent basal HIF-1α expression in tumor cells, as known from untransformed embryonic stem cells, is sufficient to induce target gene expression, probably including DNA double-strand break repair enzymes.
Similar content being viewed by others
Introduction
Hypoxic microenvironments are frequently found in solid tumors as a result of morphologically and functionally inappropriate vascularization, irregular blood flow, anemia and high oxygen consumption of rapidly proliferating malignant cells. Tumor hypoxia is associated with malignant progression; resistance to chemotherapy, photodynamic therapy and radiotherapy; increased metastasis and poor prognosis (Brown and Giaccia, 1998; Höckel et al., 1999; Brown, 2000; Höckel and Vaupel, 2001; Vaupel et al., 2001). Many of these effects in hypoxic tumor cells are mediated by oxygen-regulated transcriptional activation of a specific set of genes whose relation to therapy resistance is only poorly understood.
The hypoxia-inducible factor-1 (HIF-1) activates a number of oxygen-regulated genes critically involved in adaptation to hypoxia (Semenza, 2000; Wenger, 2002). HIF-1 is constitutively upregulated in many cancer types and plays a major role in tumor progression (Harris, 2002; Semenza, 2002). HIF-1 elevates vascular endothelial growth factor-dependent tumor angiogenesis and mediates the increased glycolytic capacity of tumor cells, known as the Warburg effect (Seagroves et al., 2001; Minchenko et al., 2002). HIF-1 is an α1β1 heterodimer specifically recognizing hypoxia-response elements of oxygen-regulated genes (Wang et al., 1995). Under normoxic conditions, the von Hippel–Lindau tumor suppressor protein (pVHL) targets the HIF-1α subunit for rapid ubiquitination and proteasomal degradation (Maxwell et al., 1999). pVHL binding requires oxygen-dependent prolyl hydroxylation of HIF-1α, representing the actual oxygen-sensing mechanism (Epstein et al., 2001; Ivan et al., 2001; Jaakkola et al., 2001).
The loss of tumor suppressors such as pVHL (Krieg et al., 2000), PTEN (Zundel et al., 2000) or p53 (Ravi et al., 2000), and oncogenes such as v-src (Jiang et al., 1997) have been shown to stabilize HIF-1α, which is overexpressed in the majority of human cancers (Zhong et al., 1999) with expression levels correlating with malignancy and negative survival prognosis (Birner et al., 2000; Aebersold et al., 2001). Thus, as shown by most published experimental tumor models, HIF-1β (Jiang et al., 1997; Maxwell et al., 1997; Griffiths et al., 2002; Höpfl et al., 2002) as well as HIF-1α (Ryan et al., 1998,2000; Kung et al., 2000; Höpfl et al., 2002; Williams et al., 2002) are positive factors for solid tumor growth. However, in one embryonic stem cell tumor model, HIF-1α-deficient (HIF-1α−/−) tumors have been shown to grow faster when compared with HIF-1α wild-type (HIF-1α+/+) tumors, apparently because of an increased rate of p53-dependent apoptosis in the HIF-1α+/+ cells (Carmeliet et al., 1998). The tumor suppressor protein p53 has been suggested to be induced by severe hypoxia (0.02% O2) and to cause apoptosis, resulting in a selective pressure against cells expressing wild-type p53 (Graeber et al., 1996). Unlike reported by others (An et al., 1998), we could not detect HIF-1α-dependent p53 stabilization under relatively mild hypoxic (1% O2) conditions (Wenger et al., 1998). Indeed, several HIF-1-independent pathways have been shown to induce p53 under severely hypoxic conditions (Alarcón et al., 1999; Hammond et al., 2002).
Resistance to radiotherapy and chemotherapy in hypoxic tumor cells has been attributed to a multitude of mechanisms. These include direct effects through lowered generation of oxygen-dependent radical formation or decreased drug accessibility of the more distant hypoxic cells. Indirect effects include clonal selection for hypoxically adapted cells with altered transcriptome or proteome patterns (Brown, 2000; Vaupel et al., 2001). However, the precise molecular mechanisms underlying the therapy resistance of hypoxic cells are not fully understood. High HIF-1α expression levels in human squamous cell head-and-neck cancers are associated with incomplete response to radiation and chemotherapy (Aebersold et al., 2001; Koukourakis et al., 2002). We thus reasoned that intrinsic mechanisms, such as constitutive variations in the HIF-1α expression levels, might contribute to therapy resistance and analysed whether HIF-1α mediates susceptibility to radiotherapy and chemotherapy.
Results
Increased susceptibility of HIF-1a-deficient cells to chemotherapeutic agents
Considerable evidence has been provided that HIF-1α is a positive factor for solid tumor growth. To analyse whether HIF-1α is also involved in chemotherapy resistance, we exposed wild-type mouse embryonic fibroblast (MEF)-HIF-1α+/+ and HIF-1α-deficient MEF-HIF-1α−/− cells for 48 h to increasing concentrations of two clinically relevant chemotherapeutic agents, carboplatin and etoposide. To assess the effects on cell growth and viability, the MTT 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide assay was employed which is based on the functional activity of mitochondrial dehydrogenases in living cells, converting MTT to the colored formazan salt (Mosmann, 1983; Hansen et al., 1989). Interestingly, dose–response curves were shifted to the left in MEF-HIF-1α−/− cells when compared to MEF-HIF-1α+/+cells (Figure 1a). The 50% inhibitory concentrations (IC50) of both agents were significantly (P<0.05) lower in HIF-1α-deficient cells, irrespective of whether the gas phase contained 20 or 1% oxygen (Figure 1b). The same elevated susceptibility could be observed with two subclones of the HIF-1α-deficient cell line, providing evidence that this was not because of clonal effects (data not shown).
Differential susceptibility of wild-type MEF-HIF-1α+/+ and HIF-1α-deficient MEF-HIF-1α−/− cells to treatment with the chemotherapeutic agents carboplatin and etoposide. (a) The cells were treated with the indicated concentrations of carboplatin and etoposide for 48 h under normoxic or hypoxic conditions. Chemosensitivity was quantified using the MTT assay. Maximal MTT conversion corresponded to 0% decrease in MTT conversion activity and was determined in solvent-treated cells (0 μ M not shown in the logarithmic scale). (b) Comparison of IC50 values between MEF-HIF-1α+/+ and MEF-HIF-1α−/− cells. Asterisks indicate statistically significant differences (P<0.05, nonparametric Wilcoxon matched pairs test). (a and b) Mean values±s.e.m. of n=6 independent experiments, each performed in triplicates, are shown
p53-independent induction of apoptosis in HIF-1a-deficient cells after treatment with chemotherapeutic agents
To assess the mode of increased cell death in HIF-1α-deficient MEF-HIF-1α−/− cells after treatment with the chemotherapeutic agents, DNA fragmentation was analysed by agarose gel electrophoresis. Following treatment for 48 h with 9 μ M carboplatin or 0.4 μ M etoposide, MEF-HIF-1α−/− cells showed the characteristic DNA laddering indicative for apoptotic DNA fragmentation (Figure 2a). In MEF-HIF-1α+/+ cells, DNA laddering was barely visible at these relatively low concentrations of the drugs. Thus, the increased chemosensitivity of HIF-1α-deficient cells, as estimated by the MTT assay, might be owing to the increased apoptosis rather than growth arrest or necrosis.
Increased carboplatin and etoposide chemosensitivity of HIF-1α-deficient cells is because of increased rate of apoptosis and does not involve p53 induction. (a) Apoptotic DNA fragmentation in MEF-HIF-1α−/− but not in MEF-HIF-1α+/+ cells. After treatment of the cells for 48 h with the indicated concentrations of carboplatin and etoposide, total cellular DNA was isolated and analysed by agarose gel electrophoresis and ethidium bromide staining. (b) Constitutive expression of p53 in the SV40 large T antigen-transformed MEF-HIF-1α+/+ and MEF-HIF-1α−/− cells. Immunoblot analysis of 75 μg protein extract derived from MEFs treated for 6 h with 200 μ M deferoxamine (DFX), 134 μ M carboplatin (C-Pt) or solvent (Ctrl)
One putative HIF-1α target responsible for the differential effects of the DNA-damaging agents in HIF-lα-deficient and wild-type cells could be the tumor suppressor protein p53 that might be stabilized by a mechanism involving HIF-1α (An et al., 1998; Ravi et al., 2000). As shown by immunoblotting, relatively high p53 protein levels are constitutively expressed in both cell lines independent of their HIF-1α genotype (Figure 2b). Expression of the SV40 large T antigen, known to stabilize and inactivate p53 (Ali and DeCaprio, 2001), explains these relatively high levels of (nonfunctional) p53 in both cell lines. Although we cannot formally exclude that these cells still contain some functionally active p53, a contribution to the HIF-1α-dependent resistance to chemotherapy is unlikely since HIF-1α reportedly is involved in the stabilization rather than activation of p53 and because the p53 protein concentrations remained unaffected by HIF-1α deficiency.
HIF-1a deficiency does not affect cellular susceptibility to iron chelators and a topoisomerase I inhibitor
Carboplatin forms platinum–DNA adducts and etoposide is a topoisomerase II inhibitor, both of which results in DNA damage. We thus examined whether other toxic substances, which function through independent mechanisms, elicit the same differential HIF-1α-dependent responses. Therefore, the cells were treated with two iron chelators, deferoxamine and ciclopirox olamine, known to induce HIF-1α protein stability at low concentrations (Wanner et al., 2000). At higher concentrations, these iron chelators interfere with the cell cycle S phase, probably because of the inhibition of ribonucleotide reductase that produces deoxyribonucleoside triphosphates required for DNA synthesis. Iron chelators hence display antiproliferative properties in tumor cells both in vitro and in clinical trials (Lederman et al., 1984; Farinelli and Greene, 1996; Gao and Richardson, 2001). Interestingly, the toxicity of the iron chelators under normoxic conditions was indistinguishable between the two cell lines, suggesting that the differential carboplatin and etoposide toxicity is because of specific mechanisms rather than because of a general vulnerability of the HIF-1α-deficient cells (Figure 3a). Of note, the iron chelators were less toxic in HIF-1α-deficient cells under hypoxic conditions. This stands in sharp contrast to the carboplatin and etoposide treatments that were more toxic in HIF-1α-deficient cells. Although the reason for this effect is currently unclear, it confirms the specificity of the carboplatin and etoposide effects and rules out gross variations in the general properties of the two cell lines.
Similar susceptibility of wild-type MEF-HIF-1α+/+ and HIF-1α-deficient MEF-HIF-1α−/− cells to treatment with the iron chelators deferoxamine and ciclopirox olamine (a) and the topoisomerase I inhibitor SN38 (b). Chemosensitivity was estimated as described for Figure 1a (shown as mean values±s.e.m., n=3 independent experiments, each performed in triplicates)
Finally, the cells were treated for 48 h with a topoisomerase I inhibitor, the camptothecin-derivative SN38. As shown in Figure 3b, the toxicity of SN38 was comparable in wild-type MEF-HIF-1α+/+ and HIF-1α-deficient MEF-HIF-1α−/− cells under both normoxic and hypoxic conditions.
Increased susceptibility of HIF-1a-deficient cells to ionizing radiation
Besides chemotherapy, radiotherapy is another tumor treatment modality known to be negatively affected by tumor hypoxia. We therefore treated the wild-type MEF-HIF-1α+/+ and HIF-1α-deficient MEF-HIF-1α−/− cells with ionizing radiation doses from 2 to 10 Gy and examined cellular viability 48 h later. As shown in Figure 4, HIF-1α-deficient MEF-HIF-1α−/− cells were significantly (P<0.01) more susceptible to irradiation when compared to wild-type cells, consistent with the inverse correlation between HIF-1α tumor expression and prognosis for the outcome of radiotherapy (Aebersold et al., 2001; Koukourakis et al., 2002).
Differential susceptibility of wild-type MEF-HIF-1α+/+ and HIF-1α -deficient MEF-HIF-1α−/− cells to irradiation (P<0.01, paired t-test). Radiosensitivity was estimated as described for Figure 1a (shown as mean values±s.e.m., n=3 independent experiments, each performed in 12 dishes simultaneously)
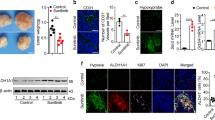
Increased susceptibility of HIF-1a-deficient tumors to chemotherapy
Immortalization and transformation of the wild-type MEF-HIF-1α+/+ and HIF-1α-deficient MEF-HIF-1α−/− cells with the SV40 large T antigen and the H-ras oncogene provided a suitable cellular model for solid tumor formation (Ryan et al., 1998). Fibrosarcomas were generated by subcutaneous injection of these cells into immunocompromised athymic nu/nu mice. As observed before (Ryan et al., 2000), the HIF-1α-deficient MEF-HIF-1α−/− tumors initially grew slower than the wild-type tumors, confirming that HIF-1α is a positive factor for solid tumor growth (data not shown). Chemotherapy of the tumors was started when an equal tumor size (100 mm3) was reached. Figure 5 shows the development of the tumor size of carboplatin- or etoposide-treated mice in relation to the saline controls. Following treatment, the tumor size of both cell lines became smaller than the corresponding controls. The MEF-HIF-1α−/− tumors were significantly (P<0.05 and <0.0001, respectively) more sensitive to chemotherapy than the wild-type cells, confirming that HIF-1α expression negatively affects therapy efficiency.
Differential efficacy of tumor chemotherapy of fibrosarcomas generated by s.c. injection of 107 wild-type MEF-HIF-1α+/+ and HIF-1α-deficient MEF-HIF-1α−/− cells into nude mice. The tumor size is shown as relative volumes between chemotherapy and saline control-treatments (mean values±s.e.m.). MEF-HIF-1α−/− cells were significantly more sensitive than MEF-HIF-1α+/+ cells: carboplatin, P<0.05, n=6 for both cell lines; etoposide, P<0.0001, n=8 for both cell lines (paired t-test)
HIF-1a-dependent repair of a DNA double-strand break
Since the common mode of action of carboplatin, etoposide and ionizing radiation might be the formation of DNA double-strand breaks, we investigated the role of HIF-1α in the repair of a fragmented reporter gene. As shown in Figure 6, a linearized and thereby functionally inactivated firefly luciferase reporter gene produced higher levels of bioluminescence following transient transfection into HIF-1α wild-type than into HIF-1α-deficient MEFs. In contrast, the cotransfected circular renilla luciferase reporter gene resulted in equal activities. Normalization of the firefly luciferase activities to the renilla luciferase activities revealed an approx 50-fold higher repair efficiency of the reporter gene in the HIF-1α wild-type than in the HIF-1α mutant cells.
Increased repair of a functionally inactivated reporter gene in HIF-1α wild-type MEFs. A linearized firefly luciferase expression plasmid was cotransfected together with a circular renilla luciferase expression plasmid into HIF-1α wild-type MEF-HIF-1α+/+ and HIF-1α-deficient MEF-HIF-1α−/− cells and luciferase activities were determined 72 h after transfection. The double-strand break repair efficiency was obtained by normalization of the firefly to the renilla luciferase activities. Mean values±s.e.m. of n=5 independent experiments, each performed in triplicates, are shown. The asterisk indicates statistically significant difference (P<0.01, nonparametric Mann–Whitney test)
Discussion
The molecular mechanisms underlying the therapy resistance of hypoxic tumor regions have not yet been completely elucidated. Here, we demonstrated that MEF-HIF-1α−/− cells are more susceptible to the treatment with carboplatin and etoposide than MEF-HIF-1α+/+ cells in vitro as well as in vivo. We provide evidence that this effect is specific and not because of clonal differences since HIF-1α-positive and -negative cells were equally sensitive to other cytotoxic drugs. What could be the nature of the HIF-1 target gene(s) responsible for this differential susceptibility? A recent report demonstrated that the multidrug-resistance gene MDR1 is a HIF-1 target gene (Comerford et al., 2002). While increased MDR1 gene expression would explain resistance of the MEF-HIF-1α−/− cells to carboplatin and etoposide, it cannot explain the increased sensitivity to ionizing radiation of MEF-HIF-1α−/− cells. This finding provides evidence against MDR1 being the only HIF-1 target gene involved in susceptibility to tumor therapy. This conclusion was further confirmed by the finding that a topoisomerase I inhibitor, in contrast to the topoisomerase II inhibitor, does not affect cell growth/viability. Thus, is there a common mode of action between carboplatin, etoposide and ionizing radiation? Carboplatin forms platinum–DNA adducts, resulting in DNA inter- and intrastrand crosslinks, and etoposide is a topoisomerase II inhibitor. Both treatments result in DNA damage, mainly by double-strand breaks. Also ionizing radiation leads to DNA double-strand breaks. On the contrary, the equally effective SN38 is a topoisomerase I inhibitor and prevents the religation of transient DNA single-strand breaks caused by topoisomerase I. Therefore, DNA repair pathways involved in DNA double-strand break repair likely include potential HIF-1 targets. The finding that a fragmented reporter gene construct resulted in higher luciferase activities in HIF-1α wild-type cells than in HIF-1α-deficient cells provides a first confirmation of this hypothesis.
In our experiments, differential susceptibility towards chemotherapeutic agents was found under both normoxic (20% O2) and hypoxic (1% O2) conditions. These hypoxic conditions are sufficient to strongly induce HIF-1α protein stabilization (Jiang et al., 1996; Jewell et al., 2001), but the severity and/or duration is apparently not sufficient to confer resistance to the chemotherapeutic agents. Differential toxic effects in the two cell lines could be observed already under normoxic conditions, despite the high instability of HIF-1α protein in the wild-type cells. However, this is consistent with the finding that HIF-1α-deficient embryonic stem cells (Iyer et al., 1998; Ryan et al., 1998) and HIF-1β-deficient hepatoma cells (Gassmann et al., 1997) repeatedly displayed a decreased expression of HIF-1 target genes already under normoxic conditions, suggesting that normoxic basal levels of HIF-1α (normally not detectable by immunoblotting) are sufficient to confer increased target gene expression as well as increased resistance to chemotherapy.
In summary, our experiments suggest that oxygen availability affects tumor therapy efficacy not only by the direct effects of severe hypoxia (anoxia), but also by genetic components involving altered HIF-1 and HIF-1 target gene expression in malignant cells. Clearly, an anti-HIF-1 strategy is required. The identification of small molecule inhibitors of HIF-1 (Rapisarda et al., 2002) and the finding that Hsp90 inhibitors of the ansamycin family strongly inhibit HIF-1 function (Isaacs et al., 2002; Katschinski et al., 2002; Mabjeesh et al., 2002) provide a first step towards a pharmacological anti-HIF-1 tumor therapy. In addition to the inhibition of tumor angiogenesis and tumor glycolysis, such a strategy, based on our study, should also improve the efficiency of classical tumor therapies.
Materials and methods
Chemicals
MTT, cis-diammine(1,1-cyclobutanedicarbo-xylato) platinum (carboplatin), 4′-desmethylepipodophyllotoxin 9-(4,6-O-ethylidene-β-D-glucopyranoside) (etoposide), deferoxamine mesylate (DFX) and ciclopirox olamine were purchased from Sigma (Taufkirchen, Germany). 7-ethyl-10-hydroxycamptothecin (SN38) was obtained from Pharmacia-Upjohn (Freiburg, Germany). For tumor chemotherapy, carboplatin (Carboplat®) and etoposide (Etopophos®) were purchased from Bristol (München, Germany).
Cell culture
MEFs were derived from mouse day 9.5 embryos, either wild-type (MEF-HIF-1α+/+) or deficient (MEF-HIF-1α−/−) for HIF-1α, immortalized with SV40 large T antigen and transformed with H-ras (Ryan et al., 2000; Seagroves et al., 2001). All cell lines were cultured in Dulbecco's modified Eagle's medium (high glucose) as described previously (Katschinski et al., 2002). Oxygen partial pressures in the hypoxic workstation (InVivO2-400, Ruskinn Technology, Leeds, UK) or in the incubator (Model 3319, Forma Scientific, Thermo Life Sciences, Egelsbach, Germany) were either 140 mmHg (20% O2 vol/vol, normoxia) or 7 mmHg (1% O2 vol/vol, hypoxia).
Cell proliferation/viability assays
Cells were cultured in 96-well plates in triplicates and allowed to attach for 6–12 h before the drugs were added for 48 h. Irradiation was performed with 10 MeV photons generated by a linear accelerator (Mevatron, Siemens Corp., Germany) at a dose rate of 3 Gy/min. Cell proliferation/viability was assessed by the MTT assay as described (Mosmann, 1983; Hansen et al., 1989). Briefly, following treatment of the cells, the medium was replaced with fresh medium containing 1 mg/ml MTT and incubated for 2 h at 37°C. One volume of 20% SDS, 50% N,N-dimethylformamide was added and incubated overnight at 37°C. Absorbances at 570 nm were determined in a 96-well photometer and means of the triplicates were calculated. Following noncellular background subtraction, all data were normalized to the MTT conversion activity of solvent-treated control cells. This value corresponds to 0% decrease in MTT conversion activity. The range of drug concentrations chosen included high doses resulting in values similar to the background, which corresponds to 100% decrease in MTT conversion activity, allowing the estimation of drug concentrations causing 50% reduction of maximal MTT conversion (IC50) for each set of experiments.
For DNA laddering, nonconfluent cells from one 150 cm2 Petri dish were collected and the DNA was isolated and analysed as described previously (Katschinski et al., 1999). Immunoblot analysis of p53 expression was performed as reported before (Wenger et al., 1998).
Experimental tumor chemotherapy
Animal experiments were performed in strict accordance with the NIH Guide for the Care and Use of Laboratory Animals and were approved by the local Governmental Commission for the Care of Animals, Kiel, Germany (V252-72241.122-2). NMRI athymic male nude mice (nu/nu) were obtained from Mollegaard and Bomholtgard Breeding and Research Centre (Ry, Denmark). Nonconfluent cells were treated with 0.2% trypsin in PBS for 10 min at 37°C and collected using a cell scraper. Cells (1 0 7) in 250 μl PBS were injected s.c. into the hind leg of ether-anesthetized mice. Tumor size was measured with a caliper every second day and the volume was estimated according to the formula: volume=length × width2 × π/6. When the tumor volume reached 100 mm3, 200 μl 0.9% NaCl containing or not containing carboplatin (30 mg/kg body weight) or etoposide (10 mg/kg body weight) was injected into the tail vein of ether-anesthetized mice. The mice were euthanized when the tumors reached a volume of >1 cm3.
DNA double-strand break repair assay
A SV40 promoter-driven firefly luciferase expression vector (pGL3Promoter, Promega) was functionally inactivated by digestion with HindIII. A 3 μg weight of this linearized plasmid was mixed with 0.1 ng of a circular plasmid containing SV40 promoter-driven renilla luciferase (pRL-SV40, Promega) which served as a control. This mixture was transiently transfected into MEFs by lipofection as described in the instructions provided by the manufacturer (Fugene 6, Roche Diagnostics, Basel, Switzerland). After 72 h of incubation at 37°C, the cells were lysed in passive lysis buffer (Promega) and the luciferase activities were determined according to the manufacturer's instructions (Dual Luciferase, Promega).
Statistical analysis
Since IC50 values are more reliable for statistical evaluation than single-dose values, IC50 values were determined from sigmoidal dose–response curve fittings of each experiment using GraphPad Prism 3.0 software (GraphPad Software, San Diego, CA, USA). Statistical analysis of IC50 values was performed using the nonparametric two-tailed Wilcoxon matched pairs test. Statistical analysis of irradiated cells and tumor volume regression was performed using the two-tailed paired t-tests. P-values <0.05 were considered statistically significant.
Abbreviations
- DFX:
-
deferoxamine mesylate
- HIF-1:
-
hypoxia-inducible factor-1
- IC50:
-
50% inhibitory concentration
- MEF:
-
mouse embryonic fibroblast
- pVHL:
-
von Hippel–Lindau tumor suppressor protein
References
Aebersold DM, Burri P, Beer KT, Laissue J, Djonov V, Greiner RH and Semenza GL . (2001). Cancer Res., 61, 2911–2916.
Alarcón R, Koumenis C, Geyer RK, Maki CG and Giaccia AJ . (1999). Cancer Res., 59, 6046–6051.
Ali SH and DeCaprio JA . (2001). Semin. Cancer Biol., 11, 15–23.
An WG, Kanekal M, Simon MC, Maltepe E, Blagosklonny MV and Neckers LM . (1998). Nature, 392, 405–408.
Birner P, Schindl M, Obermair A, Plank C, Breitenecker G and Oberhuber G . (2000). Cancer Res., 60, 4693–4696.
Brown JM . (2000). Mol. Med. Today, 6, 157–162.
Brown JM and Giaccia AJ . (1998). Cancer Res., 58, 1408–1416.
Carmeliet P, Dor Y, Herbert JM, Fukumura D, Brusselmans K, Dewerchin M, Neeman M, Bono F, Abramovitch R, Maxwell P, Koch CJ, Ratcliffe P, Moons L, Jain RK, Collen D and Keshet E . (1998). Nature, 394, 485–490.
Comerford KM, Wallace TJ, Karhausen J, Louis NA, Montalto MC and Colgan SP . (2002). Cancer Res., 62, 3387–3394.
Epstein AC, Gleadle JM, McNeill LA, Hewitson KS, O'Rourke J, Mole DR, Mukherji M, Metzen E, Wilson MI, Dhanda A, Tian YM, Masson N, Hamilton DL, Jaakkola P, Barstead R, Hodgkin J, Maxwell PH, Pugh CW, Schofield CJ and Ratcliffe PJ . (2001). Cell, 107, 43–54.
Farinelli SE and Greene LA . (1996). J. Neurosci., 16, 1150–1162.
Gao J and Richardson DR . (2001). Blood, 98, 842–850.
Gassmann M, Kvietikova I, Rolfs A and Wenger RH . (1997). Kidney Int., 51, 567–574.
Graeber TG, Osmanian C, Jacks T, Housman DE, Koch CJ, Lowe SW and Giaccia AJ . (1996). Nature, 379, 88–91.
Griffiths JR, McSheehy PM, Robinson SP, Troy H, Chung YL, Leek RD, Williams KJ, Stratford IJ, Harris AL and Stubbs M . (2002). Cancer Res., 62, 688–695.
Hammond EM, Denko NC, Dorie MJ, Abraham RT and Giaccia AJ . (2002). Mol. Cell. Biol., 22, 1834–1843.
Hansen MB, Nielsen SE and Berg K . (1989). J. Immunol. Methods, 119, 203–210.
Harris AL . (2002). Nat. Rev. Cancer, 2, 38–47.
Höckel M, Schlenger K, Höckel S and Vaupel P . (1999). Cancer Res., 59, 4525–4528.
Höckel M and Vaupel P . (2001). J. Natl. Cancer Inst., 93, 266–276.
Höpfl G, Wenger RH, Ziegler U, Stallmach T, Gardelle O, Achermann R, Wergin M, Kaser-Hotz B, Saunders HM, Williams KJ, Stratford IJ, Gassmann M and Desbaillets I . (2002). Cancer Res., 62, 2962–2970.
Isaacs JS, Jung YJ, Mimnaugh EG, Martinez A, Cuttitta F and Neckers LM . (2002). J. Biol. Chem., 277, 29936–29944.
Ivan M, Kondo K, Yang H, Kim W, Valiando J, Ohh M, Salic A, Asara JM, Lane WS and Kaelin Jr WG . (2001). Science, 292, 464–468.
Iyer NV, Kotch LE, Agani F, Leung SW, Laughner E, Wenger RH, Gassmann M, Gearhart JD, Lawler AM, Yu AY and Semenza GL . (1998). Genes Dev., 12, 149–162.
Jaakkola P, Mole DR, Tian YM, Wilson MI, Gielbert J, Gaskell SJ, von Kriegsheim A, Hebestreit HF, Mukherji M, Schofield CJ, Maxwell PH, Pugh CW and Ratcliffe PJ . (2001). Science, 292, 468–472.
Jewell UR, Kvietikova I, Scheid A, Bauer C, Wenger RH and Gassmann M . (2001). FASEB J., 15, 1312–1314.
Jiang BH, Agani F, Passaniti A and Semenza GL . (1997). Cancer Res., 57, 5328–5335.
Jiang BH, Semenza GL, Bauer C and Marti HH . (1996). Am. J. Physiol., 271, C1172–1180.
Katschinski DM, Le L, Heinrich D, Wagner KF, Hofer T, Schindler SG and Wenger RH . (2002). J. Biol. Chem., 277, 9262–9267.
Katschinski DM, Robins HI, Schad M, Frede S and Fandrey J . (1999). Cancer Res., 59, 3404–3410.
Koukourakis MI, Giatromanolaki A, Sivridis E, Simopoulos C, Turtey H, Talks K, Gatter KC and Harris AL . (2002). Int. J. Radiat. Oncol. Biol. Phys., 53, 1192–1202.
Krieg M, Haas R, Brauch H, Acker T, Flamme I and Plate KH . (2000). Oncogene, 19, 5435–5443.
Kung AL, Wang S, Klco JM, Kaelin WG and Livingston DM . (2000). Nat. Med., 6, 1335–1340.
Lederman HM, Cohen A, Lee JW, Freedman MH and Gelfand EW . (1984). Blood, 64, 748–753.
Mabjeesh NJ, Post DE, Willard MT, Kaur B, Van Meir EG, Simons JW and Zhong H . (2002). Cancer Res., 62, 2478–2482.
Maxwell PH, Dachs GU, Gleadle JM, Nicholls LG, Harris AL, Stratford IJ, Hankinson O, Pugh CW and Ratcliffe PJ . (1997). Proc. Natl. Acad. Sci. USA, 94, 8104–8109.
Maxwell PH, Wiesener MS, Chang GW, Clifford SC, Vaux EC, Cockman ME, Wykoff CC, Pugh CW, Maher ER and Ratcliffe PJ . (1999). Nature, 399, 271–275.
Minchenko A, Leshchinsky I, Opentanova I, Sang N, Srinivas V, Armstead V and Caro J . (2002). J. Biol. Chem., 277, 6183–6187.
Mosmann T . (1983). J. Immunol. Methods, 65, 55–63.
Rapisarda A, Uranchimeg B, Scudiero DA, Selby M, Sausville EA, Shoemaker RH and Melillo G . (2002). Cancer Res., 62, 4316–4324.
Ravi R, Mookerjee B, Bhujwalla ZM, Sutter CH, Artemov D, Zeng Q, Dillehay LE, Madan A, Semenza GL and Bedi A . (2000). Genes Dev., 14, 34–44.
Ryan HE, Lo J and Johnson RS . (1998). EMBO J., 17, 3005–3015.
Ryan HE, Poloni M, McNulty W, Elson D, Gassmann M, Arbeit JM and Johnson RS . (2000). Cancer Res., 60, 4010–4015.
Seagroves TN, Ryan HE, Lu H, Wouters BG, Knapp M, Thibault P, Laderoute K and Johnson RS . (2001). Mol. Cell. Biol., 21, 3436–3444.
Semenza GL . (2000). Crit. Rev. Biochem. Mol. Biol., 35, 71–103.
Semenza GL . (2002). Trends Mol. Med., 8, S62–S67.
Vaupel P, Thews O and Höckel M . (2001). Med. Oncol., 18, 243–259.
Wang GL, Jiang BH, Rue EA and Semenza GL . (1995). Proc. Natl. Acad. Sci. USA, 92, 5510–5514.
Wanner RM, Spielmann P, Stroka DM, Camenisch G, Camenisch I, Scheid A, Houck DR, Bauer C, Gassmann M and Wenger RH . (2000). Blood, 96, 1558–1565.
Wenger RH . (2002). FASEB J., 16, 1151–1162.
Wenger RH, Camenisch G, Desbaillets I, Chilov D and Gassmann M . (1998). Cancer Res., 58, 5678–5680.
Williams KJ, Telfer BA, Airley RE, Peters HP, Sheridan MR, van der Kogel AJ, Harris AL and Stratford IJ . (2002). Oncogene, 21, 282–290.
Zhong H, De Marzo AM, Laughner E, Lim M, Hilton DA, Zagzag D, Buechler P, Isaacs WB, Semenza GL and Simons JW . (1999). Cancer Res., 59, 5830–5835.
Zundel W, Schindler C, Haas-Kogan D, Koong A, Kaper F, Chen E, Gottschalk AR, Ryan HE, Johnson RS, Jefferson AB, Stokoe D and Giaccia AJ . (2000). Genes Dev., 14, 391–396.
Acknowledgements
We thank B Stier and S Schindler for excellent technical assistance, I Desbaillets for helpful advice and W Jelkmann for support. This work was supported by grants of the FSP-Oncology, University of Lübeck (to DMK and RHW) and the Deutsche Forschungsgemeinschaft (We2672/1-1 to RHW).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Unruh, A., Ressel, A., Mohamed, H. et al. The hypoxia-inducible factor-1α is a negative factor for tumor therapy. Oncogene 22, 3213–3220 (2003). https://doi.org/10.1038/sj.onc.1206385
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.onc.1206385
Keywords
This article is cited by
-
Hypoxic microenvironment in cancer: molecular mechanisms and therapeutic interventions
Signal Transduction and Targeted Therapy (2023)
-
Chloroquine prevents hypoxic accumulation of HIF-1α by inhibiting ATR kinase: implication in chloroquine-mediated chemosensitization of colon carcinoma cells under hypoxia
Pharmacological Reports (2023)
-
Interfering with Tumor Hypoxia for Radiotherapy Optimization
Journal of Experimental & Clinical Cancer Research (2021)
-
Crosstalk between endoplasmic reticulum stress and oxidative stress: a dynamic duo in multiple myeloma
Cellular and Molecular Life Sciences (2021)
-
Emerging role of tumor cell plasticity in modifying therapeutic response
Signal Transduction and Targeted Therapy (2020)