Abstract
OBJECTIVE: To evaluate the associations of body size and fat distribution with incidence of coronary heart disease (CHD) in Chinese women.
DESIGN: Population-based, prospective cohort study.
SUBJECTS: A total of 67 334 women aged 40–70 y, who had no prior history of CHD, stroke, and cancer at study recruitment.
MEASUREMENTS: Weight, standing and sitting heights, circumferences of waist and hip, and ratios of the anthropometric measurements. Outcome: incidence of CHD (non-fatal myocardial infarction (MI) or fatal CHD).
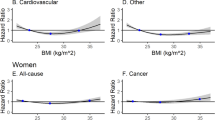
RESULTS: After a mean follow-up of 2.5 y (168 164 person-years), there were 70 incident cases of CHD (49 non-fatal MIs and 21 CHD deaths). Body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), waist-to-standing height ratio (WHtR), waist-to-sitting height ratio (WsHtR), and conicity index were all positively associated with the risk of CHD. With the exception of WHR, all other anthropometric indexes only predicted the risk of CHD among women ≤55 y of age at enrollment. The relative risks (RRs) between extreme tertiles of BMI were 9.0 (95% CI, 2.0–41.5; P for trend=0.002) for younger women vs 1.3 (0.6–3.0; P for trend=0.83) for older women. Similarly, the RRs for WC, WHtR, WsHtR, and conicity index were 6.1 (1.8–21.4) vs 1.9 (0.6–5.4), 9.4 (2.6–33.8) vs 1.2 (0.5–3.1), 15.2 (3.3–69.1) vs 1.0 (0.4–2.5), and 7.8 (2.2–28.0) vs 0.9 (0.4–2.3) for the young and elderly, respectively. In contrast, the RR for WHR was 3.2 (1.1–9.1) for the young and 2.9 (1.0–8.4) for the elderly.
CONCLUSIONS: WHR was positively associated with the risk of CHD in both younger and older women, while other anthropometrics, including BMI, were related to CHD risk primarily among younger women.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
National Task Force on the Prevention and Treatment of Obesity. Overweight, obesity, and health risk. Arch Intern Med 2000; 160: 898–904.
Manson JE, Colditz GA, Stampfer MJ, Willett WC, Rosner B, Monson RR, Speizer FE, Hennekens CH . A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med 1990; 322: 882–889.
Willett WC, Manson JE, Stampfer MJ, Colditz GA, Rosner B, Speizer FE, Hennekens CH . Weight, weight change, and coronary heart disease in women. JAMA 1995; 273: 461–465.
Rimm EB, Stampfer MJ, Giovannucci E, Ascherio A, Spiegelman D, Colditz GA, Willett WC . Body size and fat distribution as predictors of coronary heart disease among middle-aged and older US men. Am J Epidemiol 1995; 141: 1117–1127.
Rexrode KM, Carey VJ, Hennekens CH, Walters EE, Colditz GA, Stampfer MJ, Willett WC, Manson JE . Abdominal adiposity and coronary heart disease in women. JAMA 1998; 280: 1843–1848.
Rexrode KM, Buring JE, Manson JE . Abdominal and total adiposity and risk of coronary heart disease in men. Int J Obes Relat Metab Disord 2001; 25: 1047–1056.
Pouliot MC, Despres JP, Lemieux S, Moorjani S, Bouchard C, Tremblay A, Nadeau A, Lupien PJ . Waist circumference and abdominal sagittal diameter: best simple anthropometric indexes of abdominal visceral adipose tissue accumulation and related cardiovascular risk in men and women. Am J Cardiol 1994; 73: 460–468.
Han TS, van Leer EM, Seidell JC, Lean ME . Waist circumference action levels in the identification of cardiovascular risk factors: prevalence study in a random sample. BMJ 1995; 311: 1401–1405.
Dobbelsteyn CJ, Joffres MR, MacLean DR, Flowerdew G . A comparative evaluation of waist circumference, waist-to-hip ratio and body mass index as indicators of cardiovascular risk factors. The Canadian Heart Health Surveys. Int J Obes Relat Metab Disord 2001; 25: 652–661.
Ho SC, Chen YM, Woo JL, Leung SS, Lam TH, Janus ED . Association between simple anthropometric indices and cardiovascular risk factors. Int J Obes Relat Metab Disord 2001; 25: 1689–1697.
Hsieh SD, Yoshinaga H . Abdominal fat distribution and coronary heart disease risk factors in men-waist/height ratio as a simple and useful predictor. Int J Obes Relat Metab Disord 1995; 19: 585–589.
Hsieh SD, Yoshinaga H . Waist/height ratio as a simple and useful predictor of coronary heart disease risk factors in women. Intern Med 1995; 34: 1147–1152.
Deurenberg P, Deurenberg-Yap M . Differences in body-composition assumptions across ethnic groups: practical consequences. Curr Opin Clin Nutr Metab Care 2001; 4: 377–383.
Park YW, Allison DB, Heymsfield SB, Gallagher D . Larger amounts of visceral adipose tissue in Asian Americans. Obes Res 2001; 9: 381–387.
Deurenberg P, Deurenberg-Yap M, Guricci S . Asians are different from Caucasians and from each other in their body mass index/body fat per cent relationship. Obes Rev 2002; 3: 141–146.
Valdez R, Seidell JC, Ahn YI, Weiss KM . A new index of abdominal adiposity as an indicator of risk for cardiovascular disease. A cross-population study. Int J Obes Relat Metab Disord 1993; 17: 77–82.
Rose GA, Blackburn H . Cardiovascular survey methods. WHO monograph series, No. 58 World Health Organization: Geneva, Switzerland; 1982.
Zhang X, Shu XO, Gao YT, Yang G, Li Q, Li H, Jin F, Zheng W . Soy food consumption is associated with lower risk of coronary heart disease in Chinese women. J Nutr 2003; 133: 2874–2878.
Wen W, Gao YT, Shu XO, Yang G, Li HL, Jin F, Zheng W . Sociodemographic, behavioral, and reproductive factors associated with weight gain in Chinese women. Int J Obes Relat Metab Disord 2003; 27: 933–940.
Folsom AR, Kushi LH, Anderson KE, Mink PJ, Olson JE, Hong CP, Sellers TA, Lazovich D, Prineas RJ . Associations of general and abdominal obesity with multiple health outcomes in older women: the Iowa Women's Health Study. Arch Intern Med 2000; 160: 2117–2128.
Molarius A, Seidell JC . Selection of anthropometric indicators for classification of abdominal fatness—a critical review. Int J Obes Relat Metab Disord 1998; 22: 719–727.
Lean ME, Han TS, Morrison CE . Waist circumference as a measure for indicating need for weight management. BMJ 1995; 311: 158–161.
Kim KS, Owen WL, Williams D, Adams-Campbell LL . A comparison between BMI and Conicity index on predicting coronary heart disease: the Framingham Heart Study. Ann Epidemiol 2000; 10: 424–431.
Ashwell M, Cole TJ, Dixon AK . Ratio of waist circumference to height is strong predictor of intra-abdominal fat. BMJ 1996; 313: 559–560.
Willett WC, Dietz WH, Colditz GA . Guidelines for healthy weight. N Engl J Med 1999; 341: 427–434.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by NIH grant R01CA70867.
Rights and permissions
About this article
Cite this article
Zhang, X., Shu, X., Gao, YT. et al. Anthropometric predictors of coronary heart disease in Chinese women. Int J Obes 28, 734–740 (2004). https://doi.org/10.1038/sj.ijo.0802634
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0802634
Keywords
This article is cited by
-
Association of myocardial infarction and angina pectoris with obesity and biochemical indices in the South Korean population
Scientific Reports (2022)
-
Neck circumference as a measure of neck fat and abdominal visceral fat in Chinese adults
BMC Public Health (2014)
-
Body weight, fat distribution and colorectal cancer risk: a report from cohort studies of 134 255 Chinese men and women
International Journal of Obesity (2013)
-
Appropriateness of waist circumference and waist-to-hip ratio cutoffs for different ethnic groups
European Journal of Clinical Nutrition (2010)
-
Waist Circumference as a Cardiovascular and Metabolic Risk in Japanese Patients With Type 2 Diabetes
Obesity (2009)