Abstract
Background
Relative fat mass (RFM) is an emerging marker of obesity that estimates body fat percentage using a sex-specific formula containing height and waist circumference (WC). We studied the association of RFM with incident atrial fibrillation (AF), heart failure (HF), and coronary artery disease (CAD) and explored RFM cutoffs for cardiovascular disease (CVD) prediction.
Methods
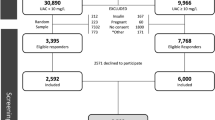
We studied 95,003 participants (age 45 ± 13 years, 59% women) without prevalent AF, HF or CAD from the population-based Lifelines study. Outcomes were ascertained using electrocardiography and self-reported questionnaire data. We used logistic regression to study the association of RFM with individual outcomes and a composite outcome (incident AF, HF, and/or CAD). Multivariable models were adjusted for components of the SCORE risk model (age, sex, systolic blood pressure, cholesterol, and smoking). Optimal cutoffs were determined using the Youden index.
Results
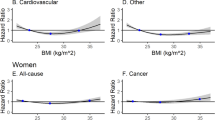
During a median follow-up of 3.8 (3.0–4.6) years, 224 (0.2%) participants developed AF, 1003 (1.1%) HF and 657 (0.7%) CAD. After multivariable adjustment, RFM was significantly associated with all outcomes (standardised OR 1.26, 95% CI 1.18–1.34 for the composite outcome). Optimal RFM cutoffs ( ≥26 for men, ≥38 for women) were lower than previously proposed RFM cutoffs ( ≥30 for men, ≥40 for women). In general, overall discriminative ability of RFM and its cutoffs was at least similar (in women) or better (in men) compared to BMI and WC. Since RFM was substantially correlated with age, we additionally determined age-specific cutoffs, which ranged from 23 to 27 in men and 33 to 43 in women.
Conclusions
RFM is associated with incident AF, HF, and CAD and may be used as a simple and intuitive marker of obesity and cardiovascular risk in the general population. This study provides potential RFM cutoffs for CVD prediction that may be used by future studies or preventive strategies targeting obesity and cardiovascular risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
Data may be obtained from a third party and are not publicly available. Researchers can apply to use the Lifelines data used in this study. More information about how to request Lifelines data and the conditions of use can be found on the Lifelines website (https://www.lifelines.nl/researcher/how-to-apply).
References
Kim MS, Kim WJ, Khera AV, Kim JY, Yon DK, Lee SW, et al. Association between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies. Eur Heart J. 2021;42:3388–403.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014;384:766–81.
Rothman KJ. BMI-related errors in the measurement of obesity. Int J Obes. 2008;32:S56–9.
Gelber RP, Gaziano JM, Orav EJ, Manson JAE, Buring JE, Kurth T. Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol. 2008;52:605–15.
Woolcott OO, Bergman RN. Relative fat mass (RFM) as a new estimator of whole-body fat percentage ─ a cross-sectional study in American adult individuals. Sci Rep. 2018;8:1–11.
Yu P, Huang T, Hu S, Yu X. Predictive value of relative fat mass algorithm for incident hypertension: a 6-year prospective study in Chinese population. BMJ Open. 2020;10:e038420.
Suthahar N, Meems LMG, Withaar C, Gorter TM, Kieneker LM, Gansevoort RT, et al. Relative fat mass, a new index of adiposity, is strongly associated with incident heart failure: data from PREVEND. Sci Rep. 2022;12:1–9.
Woolcott OO, Bergman RN. Defining cutoffs to diagnose obesity using the relative fat mass (RFM): Association with mortality in NHANES 1999–2014. Int J Obes. 2020;44:1301–10.
Andreasson A, Carlsson AC, Önnerhag K, Hagström H. Predictive capacity for mortality and severe liver disease of the relative fat mass algorithm. Clin Gastroenterol Hepatol. 2019;17:2619–20.
Suthahar N, Wang K, Zwartkruis VW, Bakker SJL, Inzucchi SE, Meems LMG, et al. Associations of relative fat mass, a new index of adiposity, with type-2 diabetes in the general population. Eur J Intern Med. 2023;109:73–8.
Scholtens S, Smidt N, Swertz MA, Bakker SJL, Dotinga A, Vonk JM, et al. Cohort profile: LifeLines, a three-generation cohort study and biobank. Int J Epidemiol. 2015;44:1172–80.
Zwartkruis VW, Groenewegen A, Rutten FH, Hollander M, Hoes AW, van der Ende MY, et al. Proactive screening for symptoms: a simple method to improve early detection of unrecognized cardiovascular disease in primary care. Results from the Lifelines cohort study. Prev Med. 2020;138:106143.
World Health Organisation (WHO). Waist circumference and waist–hip ratio. Report of a WHO Expert Consultation. Geneva, 8–11 December 2008
Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–35.
Welch Allyn. MEANS ECG Physicians’ Manual for Welch Allyn CP Series Electrocardiographs MEANS Physicians Manual Caution. 2016. www.welchallyn.com.
van der Ende MY, Siland JE, Snieder H, van der Harst P, Rienstra M. Population-based values and abnormalities of the electrocardiogram in the general Dutch population: the LifeLines cohort study. Clin Cardiol. 2017;40:865–72.
van der Ende MY, Hartman MHT, Schurer RAJ, van der Werf HW, Lipsic E, Snieder H, et al. Prevalence of electrocardiographic unrecognized myocardial infarction and its association with mortality. Int J Cardiol. 2017;243:34–9.
van der Ende MY, Hartman MHT, Hagemeijer Y, Meems LMG, de Vries HS, Stolk RP, et al. The LifeLines cohort study: prevalence and treatment of cardiovascular disease and risk factors. Int J Cardiol. 2017;228:495–500.
Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J. 2003;24:987–1003.
Huxley R, Mendis S, Zheleznyakov E, Reddy S, Chan J. Body mass index, waist circumference and waist: hip ratio as predictors of cardiovascular riska review of the literature. Eur J Clin Nutr. 2010;64:16–22.
Dunkley AJ, Stone MA, Patel N, Davies MJ, Khunti K. Waist circumference measurement: knowledge, attitudes and barriers in patients and practitioners in a multi-ethnic population. Fam Pract. 2009;26:365–71.
Senkus KE, Crowe-White KM, Locher JL, Ard JD. Relative fat mass assessment estimates changes in adiposity among female older adults with obesity after a 12-month exercise and diet intervention. Ann Med. 2022;54:1160–6.
Groenewegen A, Zwartkruis VW, Rienstra M, Hollander M, Koffijberg H, Cramer MJM, et al. Improving early diagnosis of cardiovascular disease in patients with type 2 diabetes and COPD: protocol of the RED-CVD cluster randomised diagnostic trial. BMJ Open. 2021;11:e046330.
Han TS, Tajar A, Lean MEJ. Obesity and weight management in the elderly. Br Med Bull. 2011;97:169–96.
Wagenaar CA, Dekker LH, Navis GJ. Prevalence of sarcopenic obesity and sarcopenic overweight in the general population: the lifelines cohort study. Clin Nutr. 2021;40:4422–9.
Klijs B, Scholtens S, Mandemakers JJ, Snieder H, Stolk RP, Smidt N. Representativeness of the LifeLines cohort study. PLoS ONE. 2015;10:1–12.
Aune D, Sen A, Norat T, Janszky I, Romundstad P, Tonstad S, et al. Body mass index, abdominal fatness, and heart failure incidence and mortality: a systematic review and dose-response meta-analysis of prospective studies. Circulation. 2016;133:639–49.
Aune D, Snekvik I, Schlesinger S, Norat T, Riboli E, Vatten LJ. Body mass index, abdominal fatness, weight gain and the risk of psoriasis: a systematic review and dose–response meta-analysis of prospective studies. Eur J Epidemiol. 2018;33:1163–78.
Okura Y, Urban LH, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Agreement between self-report questionnaires and medical record data was substantial for diabetes, hypertension, myocardial infarction and stroke but not for heart failure. J Clin Epidemiol. 2004;57:1096–103.
Englert H, Müller-Nordhorn J, Seewald S, Sonntag F, Völler H, Meyer-Sabellek W, et al. Is patient self-report an adequate tool for monitoring cardiovascular conditions in patients with hypercholesterolemia? J Public Health. 2010;32:387–94.
Acknowledgements
Part of this work was presented during the ESC Heart Failure 2022 Congress and published as a conference abstract (European Journal of Heart Failure 2022; 24 (Suppl. S2): 243, https://doi.org/10.1002/ejhf.2569).
Funding
This work was supported by the Dutch Heart Foundation (CVON RED-CVD, grant 2017-11).
Author information
Authors and Affiliations
Contributions
VWZ, NS, DI, MR, and RAdB contributed to the conception, design and acquisition of the work, data analysis and interpretation. VWZ drafted the manuscript. All authors contributed to the critical revision of the manuscript, gave final approval of the version to be published and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Competing interests
For the current manuscript, the authors declare no potential conflicts of interest. Outside of the submitted work, the authors disclosed the following financial support: RAdB reports grants from the Dutch Heart Foundation (CVON SHE-PREDICTS-HF, grant 2017-21; CVON RED-CVD, grant 2017-11; CVON PREDICT2, grant 2018-30; and CVON DOUBLE DOSE, grant 2020B005), leDucq Foundation (Cure PhosphoLambaN induced Cardiomyopathy) and the European Research Council (SECRETE-HF, ERC CoG 818715). RAdB has received research grants and/or fees from AstraZeneca, Abbott, Boehringer Ingelheim, Cardior Pharmaceuticals Gmbh, Ionis Pharmaceuticals, Inc., Novo Nordisk and Roche. RAdB has received speaker fees from Abbott, AstraZeneca, Bayer, Novartis, and Roche. MR reports grants from the Dutch Heart Foundation (CVON RACE V, grant 2014-09; CVON RED-CVD, grant 2017-11; CVON-AI, grant 2018B017; DECISION, grant 2018B024). The UMCG, which employs MR, received grants from SJM/Abbott (VIP-HF study) and Medtronic (Cryoballoon AF registry/biobank study).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zwartkruis, V.W., Suthahar, N., Idema, D.L. et al. Relative fat mass and prediction of incident atrial fibrillation, heart failure and coronary artery disease in the general population. Int J Obes 47, 1256–1262 (2023). https://doi.org/10.1038/s41366-023-01380-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-023-01380-8