Abstract
Congenital erythropoietic porphyria (CEP) or Günther’s disease is an inborn error of heme biosynthesis, transmitted as an autosomal recessive trait and characterized by a profound deficiency of uroporphyrinogen III synthase activity (UROIIIS). The molecular defects observed in CEP are mainly heterogeneous, except for one missense mutation, C73R (Cys to Arg substitution at codon 73) which represents nearly 40% of the disease alleles. A convenient strategy was designed to establish a rapid diagnosis at the genetic level in samples from patients with CEP. As a first step, the most frequent mutation is searched for by restriction analysis from genomic DNA amplified by PCR. Next, the nine coding exons and intron-exon boundaries are sequenced from genomic DNA. As an alternative, the mutation can be determined by sequencing the UROIIIS cDNA of the patient, using the RT-PCR technique on RNAs when a lymphoblastoid cell line can be established. Finally, for each new mutation in UROIIIS coding sequence, the corresponding mutant protein is expressed in Escherichia coli, in order to demonstrate the pathological significance of the mutation. This work describes the analysis of UROIIIS gene mutations in 10 new families with CEP and summarizes the data from 20 unrelated families studied in our laboratory. Three new missense mutations of UROIIIS coding sequence (H173Y, Q187P and P248Q) have been observed together with 8 known mutations. The significance of three intronic base changes (476 −31 T→C; 562 −4 A→T; 562 −23 A→G) is discussed. In 6 alleles out of 40 (15%), the mutation remains undetermined.
Similar content being viewed by others
Introduction
Porphyrias are a group of inherited disorders caused by specific defects along the heme biosynthetic pathway. Congenital erythropoietic porphyria (CEP) or Günther’s disease is a rare disease that is inherited as an autosomal recessive trait. CEP is characterized by severe cutaneous photosensitivity, chronic hemolysis and massive porphyrinuria resulting from the accumulation in the bone marrow, peripheral blood and other organs, of large amounts of predominantly type I porphyrins, which are not substrates for heme synthesis [1]. A characteristic abnormality of the disease is an 80–98% decrease in the erythrocytic activity of uroporphyrinogen III synthase (UROIIIS), the fourth enzyme of the heme biosynthetic pathway: hydroxymethylbilane hydrolase [cyclizing] (EC.4.2.1.75) [2, 3]. Human UROIIIS enzyme has been purified to homogeneity from erythrocytes as a monomeric protein, with an apparent molecular mass (Mr) of 29,500 [4]. The determination of the nucleotide sequence of the cDNA encoding UROIIIS [5] and the characterization of the UROIIIS gene structure [6] has made it possible to study the molecular lesions responsible for the disease. The gene encoding UROIIIS protein is unique, contains 10 exons and has been assigned to the chromosomal region 10q25.3→q25.6. The size of the coding sequence and the gene are 795 bp and 60 kb, respectively [6, 7].
The mutations causing CEP are mainly heterogeneous [8–16]. Eleven missense mutations are associated with different levels of residual UROIIIS activity: L4F, Y19C, P53L, T62A, A66V, C73R, V99A, A104V, S212P, G225S and T228M. Two point mutations are responsible for a truncated protein: the nonsense Q249X and the frameshift 633insA mutations. Four putative splicing defects have been observed: the deletion of exon 2, 4, or 9, corresponding to the changes (63 +1 G→A), (148 del 98) and (660 +4 del A), respectively, and an 80-bp insertion between the last two exons of UROIIIS gene (660ins80). The mutations are designated according to the nomenclature recommended by Beaudet and Tsui [17]. The missense mutation C73R is the most common, representing at least one third of the mutated alleles studied, while the other mutations are rarely observed in more than one family [10, 14].
In this work, we describe the analysis of UROIIIS gene mutations in 10 new families and summarize the analysis in twenty-one CEP patients, using cDNA and genomic sequencing together with cDNA-directed expression in a prokaryotic system of the corresponding mutant protein.
Materials and Methods
In vitro Amplification of Genomic DNA
High-quality genomic DNA was prepared from whole blood by extraction with phenol and chloroform after overnight digestion with proteinase K. Two hundred to 500 ng of genomic DNA were amplified on a Hybaid Omnigene thermal cycler. The reaction mix contained 50 mM KCl, 10 mM Tris-HCl pH 9, 0.1% Triton X-100, 0.15 mM MgCl2, 10 pmol of each primer, 200 nM of the four dNTPs and 1 U Taq polymerase (Promega, France) in a final volume of 50 µl. After a first denaturation step at 94°C during 3 min, 30 cycles consisted in denaturation at 92°C for 10 s, annealing at 45°C to 56°C for 30 s, depending on the Tm of the primers, and elongation at 72°C for 1 min, followed by a last elongation at 72°C for 5 min. The sequences of the primers are detailed in table 1. Each sense primer is biotinylated at the 5′ end to allow the purification of single-stranded DNA using its affinity for streptavidin for the subsequent sequencing step.
Restriction Analysis of the C73R Mutation
The fourth coding exon of the UROIIIS gene was amplified from genomic DNA using the primer set 4 (4S, 4AS1). One third of the PCR product was digested with the restriction enzyme MaeII, at 65°C for 3 h and analysed on a 3% agarose gel. The enzyme recognizes a new site when the mutation is present. A single 140-bp undigested fragment was detected in normal samples, a 100-bp fragment in homoallelic samples and both fragments in heteroallelic samples.
Direct Sequencing Using Paramagnetic Beads
A solid-phase sequencing protocol, using single stranded PCR products immobilized on paramagnetic beads, was chosen to obtain unambiguous sequencing results. The biotinylated strand of each PCR product was purified by affinity with streptavidin-coated paramagnetic beads by means of a magnetic separator (Dynabeads M-280 Streptavidin, Biosys, France).
40 µl of the PCR reaction were incubated with the beads, the strands were separated in 0.1 M NaOH and the nonbiotinylated strand was removed as recommended by the supplier. The biotinylated strand was used as template for dideoxy chain termination sequencing using a T7 sequencing kit (Pharmacia, France). The antisense primer was used for both PCR and sequencing with consistent results. An unusually high level of secondary structure was observed when sequencing exon 9 with primer set (9S1, 9AS) and the sequence was determined from the nonbiotinylated strand using a sense primer (9S2). Exon 10 was sequenced with an internal antisense primer (10AS2) in order to read directly the coding sequence of this last exon of the UROIIIS gene. The results of the sequence analysis of the mutant P248Q were ambiguous because of the present band compression. The mutation was confirmed by hydridization of the PCR product with an allele-specific mutated oligonucleotide as described [10].
In vitro Amplification of UROIIIS cDNA
Lymphoblastoid cell lines were successfully established in some patients by Epstein-Barr virus (EBV) transformation of peripheral B lymphocytes at the Généthon laboratory (Evry, France). Total RNAs were prepared by phenol-chloroform-isothiocyanate extraction [18] and reverse-transcribed from oligo(dT) primers, using Moloney murine leukemia virus reverse-transcriptase (RT), according to the manufacturer’s instructions (Gibco BRL). A first PCR was performed with the primers US2 and 10AS2, followed by a nested PCR with a biotinylated sense primer, US12B, and the antisense primer US4. PCR conditions were the same as those described for genomic DNA. The resulting PCR product was sequenced directly as a single-stranded product using M280-streptavidin beads and a T7 sequencing kit for manual sequencing.
Prokaryotic Expression of UROIIIS Mutant Proteins
The normal and mutant UROIIIS alleles were expressed in E. coli using the pKK 223.3 vector (Pharmacia, France) as previously described [10, 13]. The mutations H173Y, Q187P and P248Q are included in a 300-bp Ncol fragment of UROIIIS cDNA. Each mutated NcoI fragment was cloned as a mutated cassette in the normal pKK UROIIIS plasmid. The mutated cassettes for H173Y and Q187P were obtained from total RNAs by RT-PCR and a nested PCR using the primers US13E and US4. The mutated cassette for P248Q was constructed by mutagenesis using sequential PCR [19]. First, two overlapping mutated PCR fragments were obtained from the normal cDNA using the primer pairs US12B-US248MAS and US248MS-US4 and gel purified with the Wizard PCR purification system (Promega, France). The corresponding PCR products were self annealed and amplified with the external primers US12B and US4. The resulting PCR product was digested with NcoI, gel purified and cloned in the normal pKK UROIIIS plasmid. In the three constructs, the sequence of the mutated cassette was checked in both directions to confirm the engineered sequence and the absence of PCR errors. Bacterial growth, IPTG induction, and UROIIIS enzyme assay were performed as described [10, 13].
Results
Mutations in the UROIIIS gene were systematically searched for by cDNA and/or genomic sequencing in 11 new patients with CEP from 10 families (VIII, IX, XI, XII, XIV, XV, XVI, XVIII, XIX, and XX) described in table 2. A brief description of the patients is given in table 2, concerning sex, age at the time of the genetic analysis, geographic origin and disease severity. In mild and moderate forms, the symptoms were mainly cutaneous and often allowed a normal life in adulthood. In severe forms, transfusion dependency was observed due to recurrent anemia. Two infants (X and XVII) died from acute hemolysis at the age of 1 day and 2 months, respectively; a 3rd one was stillborn (XIX). Two patients were born of consanguineous parents: patient II (the parents are first cousins) and patient VIII (multiple consanguinity).
The most common mutation in CEP, C73R, was observed in 9 patients: 8 of them were heteroallelic (patients IX, XI, XII, XIV, XV, XVIII, XIX, and XX) and 1 was homoallelic for the mutation (patient XVI). The restriction patterns of normal (lane 1), homoallelic (lane 3) and heteroallelic (lanes 2, 4) samples are shown in figure 1. One previously reported mutation, T228M, was observed in 1 of the 9 new patients presented in table 2: patient IX was shown to be a compound heterozygote C73R/T228M. The analysis of the patients I–VII, X, XIII, and XVII have been published previously [8, 10, 12, 13, 16].
Identification of the C73R mutation by restriction analysis. A 140-bp PCR product containing exon 4 is amplified from genomic DNA and digested with MaeII enzyme which recognizes a new site when the mutation is present. A single 140-bp fragment is seen in normal samples (lane 1), a 100-bp fragment in homoallelic samples (lane 3) and both fragments in heteroallelic samples (lanes 2 and 4). A 100-bp ladder and a 140-bp undigested PCR product are loaded in lanes 5 and 6, respectively.
Three new exonic mutations were identified in four different patients: patient VIII was homoallelic for the mutation H173Y, patients XV was heteroallelic for the mutation Q187P, and patients XVIII and XX were both heteroallelic for the mutation P248Q. The missense mutation H173Y was identified by cDNA sequencing (fig. 2) and confirmed by sequencing the genomic fragment which contains exon 8. The mutation abolished a NsiI restriction site. The homozygosity was not surprising since multiple consanguinity was observed in the family. The missense mutation Q187P was also identified by cDNA sequencing (fig. 3) and confirmed by sequencing an exon 8 genomic fragment. The C73R mutant allele was transmitted by the mother and the Q187P mutant allele by the father of the proband. In patient XVIII, the mutation P248Q was identified by sequencing the genomic fragment containing exon 10. However, the sequence was ambiguous because of band compressions in the region of the nucleotide change C→A at nucleotide 743. RNAs were not available to analyze the cDNA in this patient. Therefore, the mutation was confirmed by allele specific oligonucleotide hybridization using the genomic fragment containing exon 10 (fig. 4). The same mutation was detected by automatic sequencing in a second family (XX) in two brothers aged 2 months and 2 years, respectively. The C73R mutant allele was transmitted by the mother, the P248Q mutant allele by the father of the proband in both pedigrees (XVIII and XX).
Confirmation of sequencing results by allele specific hybridization. The mutation P248Q was identified by direct sequencing of the last exon of UROIIIS gene, amplified from genomic DNA. Sequencing data were confirmed by hybridization of the PCR product with a 19-mer oligonucleotide containing the substitution. The samples from the proband and his father were both recognized by the mutated oligonucleotide allele while the sample from the mother was not.
The three new exonic mutations were introduced in the expression vector pKK 223.3 containing the normal UROIIIS cDNA sequence either by cloning the mutated cDNA obtained from RT-PCR products or by site-directed mutagenesis. None of the three mutated constructs expressed any residual UROIIIS activity in E. coli lysates (table 3).
In 4 patients (XI, XII, XIV and XIX), heterozygous for the common mutation C73R and in 3 previously described patients (III, VI, VII) a systematic analysis of the 9 exonic fragments of UROIIIS gene was performed. The genomic sequencing showed three intronic nucleotide changes in three of these heterozygous patients (III, VII, XII). In patient III, an A→T substitution is observed at position −4 from the 3′ acceptor site of intron 8: CTCAG is read instead of CACAG (542 −4 A→T). In patients VII and XII, the substitution is located in the region of the branch points of introns 7 and 8, 476 −31 T→C and 562 −23 A→G, respectively. The pathological significance of these intronic base changes is discussed in the next section.
Discussion
Different techniques were combined to analyze the mutations in amplified segments of the UROIIIS gene in CEP patients: restriction analysis of genomic exonic fragments, direct sequencing on genomic DNA or cDNA, allele-specific hybridization. Finally, the exonic mutations were expressed in a prokaryotic system in order to measure the UROIIIS residual activity of the corresponding mutated proteins.
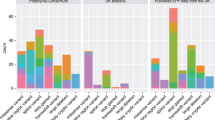
The mutations determined in 20 unrelated CEP families are presented in table 2 and the relative frequency estimated in table 4. The high frequency of the C73R mutation is obvious with 19 mutant alleles out of 40 (47.5%) in 15 independent families out of 20. As a consequence, in each new CEP patient, the C73R mutation is investigated first using a simple restriction analysis, and the systematic sequencing of the exons of the UROIIIS gene is undertaken afterwards. A lower frequency (26%) of the C73R mutation was described by Xu et al. [14] in patients of various ancestry, as opposed to the Caucasian origin of the patients described in this work. No clear racial or sexual predominance has been observed in CEP. However, the disease is too rare (200 cases reported before 1992 [1] to allow a valuable analysis of the allelic frequency as a function of ethnic origins.
The C73R mutation is usually associated with a severe phenotype at the homoallelic state and the family may ask for a prenatal diagnosis. In family XVII, a first child was diagnosed as homoallelic for the mutation C73R. On the next pregnancy the amniotic cells and the amniotic fluid were analysed for porphyrin accumulation and UROIIIS genotype at 16 weeks of gestation. The fetus was also homoallelic for the mutation and a large increase in uroporphyrin I was noted. The diagnosis led to the interruption of the pregnancy [16].
The strategy allowed a rapid determination of the sequence of the entire coding region and all intron/exon boundaries of the UROIIIS gene, a 60-kb gene encoding 10 exons [6]. A biotinylated primer was used in each amplification of either genomic DNA or cDNA to separate single strands for direct solid-phase sequencing [20]. This approach has proved to be more efficient than mutation detection methods such as the single strand conformation polymorphism technique, [21] heteroduplex analysis, [22] or the use of denaturing gradient gel electrophoresis [23] since each of them requires one round of mutation detection followed by sequencing. In the future, the use of an automatic sequencer should shorten the analysis and facilitate the comparison of the sequencing patterns of different patients. In the last patients studied (family XX), the mutations were identified by automatic sequencing using the cycle sequencing strategy and dye terminator labeling (ABI 377, Perkin Elmer).
Three new missense mutations were identified, H173Y, Q187P and P248Q, which markedly altered the nature of the encoded amino acid. The resulting mutant protein had no residual activity in the expression system. The H173Y mutation was observed at the homoallelic state in a consanguineous family and was associated with a severe phenotype. The Q187P and P248Q mutations were associated with the C73R mutant allele and resulted also in severe forms with mutilating cutaneous lesions and transfusion dependency. Unexpectedly, the P248Q mutation was detected in two unrelated Spanish families (XVIII and XX) who lived in distant regions, Madrid and Seville, respectively.
Recently, three point mutations responsible for a splicing defect in UROIIIS gene have been described: 63 +1 G→A, 148 del 98 (244 G→T) and 660 +4 del A, resulting in the deletion of exon 2, 4 and 9, respectively [14]. Special attention was given to intron-exon boundaries and three nucleotide changes were observed in three patients heteroallelic for the most common mutation C73R. In patient III, the A→T substitution at nucleotide −4 of the 3′ acceptor site of intron 8 should not influence the splicing since any nucleotide can be present at this position in the consensus sequence (fig. 5) [24]. In patient VII the T→C substitution at nucleotide −31 is located in the best-guess region for the branch point consensus sequence of intron 7 [24]. However, both nucleotides C or T can be seen at this position, as shown in figure 5. Therefore, these nucleotide changes were considered as rare polymorphisms rather than mutations linked to the disease. Three other polymorphisms were observed in the patients described in this report: one in intron 5, at position +64, and two in intron 8, at positions −26, and +19, respectively. For the 18 alleles tested, in intron 5, the allelic frequency was 0.89 and 0.11 for G and C, respectively. In the same sample, the allelic frequency was 0.72 and 0.28 for C and T, respectively, at both positions in intron 8. In patient XII the A→G substitution at position −23 in intron 8 is the best guess location for the A of the branch point consensus [25], as shown in figure 5. In a number of β-globin thalassemia variants, mutations of the pre-mRNAs generate new splice sites or activate cryptic ones, leading to aberrant splicing patterns [26] and providing a convenient model to study exon and intron sequences required for splicing [27]. Recently, in intron 7 of the IL-3 receptor gene (α-subunit) a 5-bp deletion at the branch point has been demonstrated to cause an aberrant splicing. This nucleotide change was considered as responsible for the mutant phenotype observed in the A/J mouse [28]. However, in patient XII, the immortalization of lymphoblastoid cells failed, blood samples were not suited for RNA preparation and the presence of abnormality spliced transcripts could not be documented.
Consensus sequences for the branch point and the 3′ acceptor sites and location of base changes in UROIIIs introns 7 and 8. The consensus sequences for the branch point and the 3′ acceptor sites are indicated together with the nucleotide frequency of each position. The consensus sequences are aligned with the normal sequences observed in UROIIIS introns 7 and 8. The best guess position for the A of the branch point is −23 in intron 8 and −29 in intron 7. Three individual base changes and a common polymorphism are shown.
The mutation was considered not determined in 6 of the 40 alleles described in table 2, from the sequencing of all 9 coding exons of the UROIIIS gene. The overall frequency of unknown alleles in CEP patients is 15% as shown in table 4. The undetected mutations may involve gene deletions, promoter mutations or other splicing defects. Unfortunately, the large size of UROIIIS gene precludes a complete analysis of gene defects as a routine analysis in patients with CEP.
Finally, the mutations of the UROIIIS gene are mainly heterogeneous since most defects appear only in individual families. Only four families were known to be consanguineous among 39 families mentioned in table 4 and 4 different mutations were observed: C73R [8], 660 +4 del A [14], S212P [15], and H173Y (this work). Of note, a second mutant allele (Q249X) was observed in the consanguineous family showing the S212P allele. In six homoallelic patients for the C73R mutation, only 1 was born of consanguineous parents (first cousins). Indeed, the prevalence of the disease is too low (less than 10−6) to analyze the genetic heterogeneity of the disease from the estimation of consanguineous marriages, as previously described [29].
As a conclusion, the identification of UROIIIS gene mutations in CEP allows a precise characterization of the disease, the detection of heterozygotes for accurate genetic counselling and improved prenatal diagnosis in severe cases.
References
Kappas AS, Sassa S, Galbraith RA, Nordmann Y: The porphyrias; in Scriver CR, Beaudet AL, Sly WS, Valle D (eds): The metabolic basis of inherited disease. New York, McGraw-Hill, 1995, pp 2103–2159.
Romeo G, Levin EY: Uroporphyrinogen III cosynthase in human congenital erythropoietic porphyria. Proc Natl Acad Sci USA 1969;63:856–863.
Deybach JC, De Verneuil H, Phung N, Nordmann Y, Puissant A, Boffety B: Congenital erythropoietic porphyria (Günther’s disease): Enzymatic studies on two cases of late onset. J Lab Clin Med 1981;97:551–558.
Tsai SF, Bishop DF, Desnick RJ: Purification and properties of uroporphyrinogen III synthase from human erythrocytes. J Biol Chem 1987;262:1268–1273.
Tsai SF, Bishop DF, Desnick RJ: Human uroporphyrinogen III synthase: Molecular cloning, nucleotide sequence and expression of a full-length cDNA. Proc Natl Acad Sci USA 1988; 85:7049–7053.
Warner CA, Yoo HW, Tsai SF, Roberts AG, Desnick RJ: Congenital erythropoietic porphyria: Characterization of the genomic structure and identification of mutations in the uroporphyrinogen III synthase gene (abstract). Am J Hum Genet 1990;47:83.
Astrin KH, Warner CA, Yoo HW, Goodfellow PJ, Tsai SF, Desnick RJ: Regional assignment of the human uroporphyrinogen III synthase (UROIIIS) gene to chromosome 10q25.2–q26.3. Hum Genet 1991;87:18–22.
de Verneuil H, Deybach JC, Grandchamp B, Nordmann Y: Coexistence of two point mutations in the uroporphyrinogen III synthase gene in one case of congenital erythropoietic porphyria. Blood 1989;74:105A.
Deybach JC, De Verneuil H, Boulechfar S, Grandchamp B, Normann Y: Point mutations in the uroporphyrinogen III synthase gene in congenital erythropoietic porphyria. Blood 1990;75:1763–1765.
Boulechfar S, Da Silva V, Deybach JC, Nordmann Y, Grandchamp B, De Verneuil H: Heterogeneity of mutations in uroporphyrinogen III synthase gene in congenital erythropoietic porphyria. Hum Genet 1992;88:320–324.
Warner CA, Yoo HW, Roberts AG, Desnick RJ: Congenital erythropoietic porphyria: Identification and expression of exonic mutations in the uroporphyrinogen III synthase gene. J Clin Invest 1992;89:693–700.
Verstraeten L, Van Regemorter N, Pardou A, De Verneuil H, Da Silva V, Rodesch F, Vermeylen D, Donner C, Noël JC, Nordmann Y, Hassoun A: Biochemical diagnosis of a fatal case of Günther’s disease in a newborn with hydrops foetalis. Eur J Clin Chem Clin Biochem 1993;31:121–128.
Bensidhoum M, Ged C, Hombrados I, Moreau-Gaudry F, Hift RS, Meissner P, Sturrock ED, De Verneuil H: Identification of two new mutations in congenital erythropoietic porphyria. Eur J Hum Genet 1995;3:102–107.
Xu W, Warner CA, Desnick RJ: Congenital erythropoietic porphyria: Identification and expression of 10 mutations in the uroporphyrinogen III synthase gene. J Clin Invest 1995;95: 905–912.
Tanigawa K, Bensidhoum M, Nakamura N, Namba H, Yamashita S, De Verneuil H, Ged C: A novel point mutation in congenital erythropoietic porphyria in two members of a Japanese family. Hum Genet, in press.
Ged C, Moreau-Gaudry F, Taine L, Hombrados I, Calvas P, Colombies P, De Verneuil H: Prenatal diagnosis in congenital erythropoietic porphyria by metabolic measurement and DNA analysis. Prenat Diagn 1996;16:83–86.
Beaudet AL, Tsui LP: A suggested nomenclature for designating mutations. Hum Mutat 1993;2:245–248.
Chomczynski P, Sacchi N: Single-step method for RNA isolation by acid guanidium thiocyanate-phenol-chloroform extraction. Anal Biochem 1987;162:156–159.
Cormack B: Mutagenesis by polymerase chain reaction; in Current Protocols in Molecular Biology, New York, Wiley, 1991, vol 1, suppl 15.
Hultman T, Stahl S, Hornes E, Uhlén M: Direct solid phase sequencing of genomic and Plasmid DNA using magnetic beads as solid support. Nucleic Acids Res 1989;17:4937–4946.
Orita M, Suzuki Y, Sekiya T, Hayashi K: Rapid and sensitive detection of point mutations and DNA polymorphisms using the polymerase chain reaction. Genomics 1989;5:874–879.
White WB, Carvalho M, Derse D, O’Brien SJ, Dean M: Detecting single base substitutions as heteroduplex polymorphisms. Genomics 1992; 12:301–306.
Myers RM, Maniatis T, Lerman IS: Detection and localization of single base changes by denaturing gel electrophoresis. Methods Enzymol 1987;155:501–527.
Shapiro MB, Senapathy P: RNA splice junction of different classes of eukaryotes: Sequence statistics and functional implications in gene expression. Nucleic Acids Res 1987; 15: 7155–7174.
Senapathy P, Shapiro MB, Harris NL: Splice junctions, branch point sites and exons: Sequence statistics, identification and applications to genome project. Methods Enzymol 1990;183:252–278.
Schwartz E, Benz EJ: The thalassemia syndrome; in Hoffman R, Benz EJ, Shattil SJ, Furie B, Cohen HJ (eds): Hematology: Basis Principles and Practice. New York, Churchill Livingstone, 1991, pp 368–392.
Dominski Z, Kole R: Identification and characterization by antisense oligonucleotides of exon and intron sequences required for splicing. Mol Cell Biol 1994;14:7445–7454.
Ichihara M, Hara T, Takagi M, Cho LC, Gorman DM, Miyajima A: Impaired interleukin-3 (IL-3) response of the A/J mouse is caused by a branch point deletion in the IL-3 receptor alpha subunit gene. EMBO J 1995;14:939–950.
Romeo G, Bianco M, Devoto M, Menozzi P, Mastella G, Giunta AM, Micalizzi C, Antonelli M, Battistini A, Santamaria F, Castello D, Marianelli A, Marchi AG, Manca A, Miano A: Incidence in Italy, genetic heterogeneity, and segregation analysis of cystic fibrosis. Am J Hum Genet 1985;37:338–349.
Acknowledgements
The authors wish to thank all the physicians for providing patient specimens, S. Labatut and M.-H. Dealbert for technical assistance and M.-T. Sanchez for typing the manuscript. The work was supported by grants from the Ministère de la Recherche et de la Technologie (MRT), the Institut National de la Santé et de la Recherche Médicale (INSERM-CRI 95042) and the Conseil Régional d’Aquitaine.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Fontanellas, A., Bensidhoum, M., de Salamanca, R.E. et al. A Systematic Analysis of the Mutations of the Uroporphyrinogen III Synthase Gene in Congenital Erythropoietic Porphyria. Eur J Hum Genet 4, 274–282 (1996). https://doi.org/10.1159/000472214
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1159/000472214
Key Words
This article is cited by
-
Pharmacogenetic and clinical risk factors for bevacizumab-related gastrointestinal hemorrhage in prostate cancer patients treated on CALGB 90401 (Alliance)
The Pharmacogenomics Journal (2024)
-
Mutational analysis of uroporphyrinogen III cosynthase gene in Iranian families with congenital erythropoietic porphyria
Molecular Biology Reports (2012)
-
Successful match-unrelated donor bone marrow transplantation for congenital erythropoietic porphyria (Günther disease)
European Journal of Pediatrics (2005)
-
Lentivirus-mediated gene transfer of uroporphyrinogen III synthase fully corrects the porphyric phenotype in human cells
Journal of Molecular Medicine (2003)
-
Congenital Erythropoietic Porphyria: Prenatal Diagnosis and Autopsy Findings in Two Sibling Fetuses
Pediatric and Developmental Pathology (2001)