Abstract
Study design:
Case report.
Objective:
To report on the need to consider the possibility of the superior mesenteric artery syndrome (SMAS) even after a long time from the initial spinal cord injury.
Setting:
Ulsan, South Korea.
Methods:
A 41-year-old man with complete tetraplegia was evaluated for nausea and vomiting. He had a cervical cord injury 11 years previously and his body mass index was 18.6 on admission. The contrast-enhanced abdominal computed tomography (CT) showed intestinal obstruction at the third-portion of the duodenum. With frequent position change and intravenous electrolyte support, the symptoms resolved. There was no relapse of the symptoms with some lifestyle modifications.
Conclusion:
Patients with spinal cord injury may develop SMAS even long after their initial injury.
Similar content being viewed by others
Introduction
The superior mesenteric artery syndrome (SMAS) is caused by obstruction of the third-portion of the duodenum between the superior mesenteric artery and aorta. SMAS is an uncommon condition that can develop where there is thinning of the intra-abdominal fat layer, thoraco-lumbar spine extension or prolonged immobilization in the supine position.
Previous studies on SMAS in patients with spinal cord injuries report its occurrence usually during the first week after injury. However, Laffont et al.1 reported that SMAS could occur ‘late’ after a spinal cord injury; however, ‘late’ SMAS usually occurred within 3 months after the spinal cord injury. And we found no reports of SMAS after several years of spinal cord injury.
We report SMAS in the tetraplegic patient 11 years after the initial cervical cord injury.
Case report
A 41-year-old man complained of nausea and frequent vomiting, sometimes bilious material, during the third week of hospitalization.
The cervical spinal cord was injured 11 years ago and the patient has had tetraplegia since then (motor level C5/C5, sensory level C5/C5 ASIA-A). On admission, the body mass index was 18.6 kg m−2.
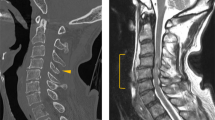
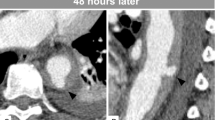
The physical examination revealed no pain, tenderness or muscle guarding of the abdomen. The blood pressure was 130/90 mm Hg, pulse rate was 80 min−1, slightly increased compared with the average of the previous week. The bowel sounds were decreased in the epigastric area on auscultation. The patient showed no improvement after 24 h of conservative therapy; oral feeding was restricted and intravenous electrolyte, fluid and supplementary anti-spasmotic agent therapy were provided. At 36 h after the onset of symptoms, a contrast-enhanced abdominal computed tomography (CT) was performed and showed obstruction at the third-portion of the duodenum and distension of the stomach with fluid (Figure 1). The aortomesenteric distance was 8 mm (10–28 mm in normal). A gastroduodenoscopy was performed and showed no mass or surface lesions in the stomach and duodenum. The patient was diagnosed with SMAS and encouraged to continue the frequent position changes lying on the side. Endoscopic suction and L-tube drainage was also performed. The symptoms resolved within 24 h and the patient had no relapse of the symptoms for 6 months.
Discussion
Superior mesenteric artery syndrome is characterized by postprandial epigastric pain, eructation, fullness and vomiting.2 However, SMAS is usually a diagnosis of exclusion; the diagnosis is often delayed because its symptoms are very similar to many other common disorders. For a patient with a cervical cord injury, it is even harder to diagnose because the visceral afferent pathway is often disrupted, and they may not be able to feel any pain even when they have serious abdominal pathology. In these cases, some signs and symptoms might be suggestive such as an elevated pulse rate, an elevated blood pressure, increased abdominal spasticity, sweating above the level of the lesion and autonomic dysreflexia.
Radiology studies are necessary for the diagnosis of the SMA syndrome. An upper gastrointestinal series and arteriography have been used to demonstrate the SMA syndrome; the upper gastrointestinal series shows dilated first and second portions of the duodenum, abrupt compression at the third portion of the duodenum and a delay of 4∼6 h in the gastroduodenal transit. However, the upper gastrointestinal may not be sensitive enough to detect changes associated with SMAS because the symptoms are often intermittent. Arteriography may show a decreased aortomesenteric angle (7∼22°) and a distance ranging from 2 to 8 mm; usually 25∼60° and 10–28 mm under normal conditions. At present, three-dimensional computed tomography may be more useful and convenient for the evaluation of the aortomesenteric distance and to visualize retroperitoneal and mesenteric fat, as well as obstruction and dilatation of the duodenum seen in the upper gastrointestinal series.3
There are some risk factors that can decrease the aortomesenteric angle and cause SMAS: (1) disorders associated with a decrease in the retroperitoneal or mesenteric fat; (2) acute or long-term trauma causing dystonic enervation of the abdominal wall and spinal muscles; and (3) spinal deformity, trauma or mass lesions.4 Prolonged immobilization in the supine position may also be a risk factor.5
During the early stage of a spinal cord injury, patients undergo weight loss, are immobilized and have decreased abdominal muscle tone; these are all risk factors for SMAS. However, in the case of tetraplegia, due to a cervical cord injury, these risk factors may persist. In our case, the patient had two of these risk factors: low body mass index and prolonged periods of time in the supine position. Therefore, SMAS should be considered in patients with spinal cord injuries long after the initial injury if risk factors are present.
References
Laffont I, Bensmail D, Rech C, Prigent G, Loubert G, Dizien O . Late superior mesenteric artery syndrome in paraplegia: case report and review. Spinal Cord 2002; 40: 88–91.
Wilkinson R, Huang CT . Superior mesenteric artery syndrome in traumatic paraplegia: a case report and literature review. Arch Phys Med Rehabil 2000; 81: 991–994.
Ha CD, Alvear DT, Leber DC . Duodenal derotation as an effective treatment of superior mesenteric artery syndrome: a thirty-three year experience. Am Surg 2008; 74: 644–653.
Baltazar U, Dunn J, Floresguerra C, Schmidt L, Browder W . Superior mesenteric artery syndrome: an uncommon cause of intestinal obstruction. South Med J 2000; 93: 606–608.
Adams JB, Hawkins ML, Ferdinand CH, Medeiros RS . Superior mesenteric artery syndrome in the modern trauma patient. Am Surg 2007; 73: 803–806.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kim, S., Yoon, J., Park, B. et al. Superior mesenteric artery syndrome in a tetraplegic patient, 11 years after a spinal cord injury: a case report. Spinal Cord 48, 838–839 (2010). https://doi.org/10.1038/sc.2010.24
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.24
Keywords
This article is cited by
-
Co-occurring superior mesenteric artery syndrome and nutcracker syndrome requiring Roux-en-Y duodenojejunostomy and left renal vein transposition: a case report and review of the literature
Journal of Medical Case Reports (2018)
-
Wilkie or Ogilvie?
Spinal Cord Series and Cases (2018)