Key Points
-
Fibroblastic reticular cells (FRCs) are heterogeneous stromal cells. Subsets of FRCs include: T cell zone reticular cells that produce interleukin-7 (IL-7) to support naive T cells; resident and inducible B cell zone reticular cells that support naive B cells and follicle integrity; pericytic FRCs that support high endothelial venule (HEV) barrier function; follicular dendritic cells (FDCs) that support germinal centre function; and marginal reticular cells that can differentiate into FDCs.
-
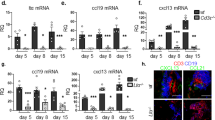
Crucial checkpoints in mesenchymal stromal cell development are retinoic acid signalling to mesenchymal progenitor cells, which creates the lymph node anlage, followed by the attraction of lymphotoxin ligand-bearing group 3 innate lymphoid cells (usually mediated by CXC-chemokine ligand 13 (CXCL13)). Lymphotoxin-β receptor (LTβR) signalling to mesenchymal precursor cells results in the development of CC-chemokine ligand 19 (CCL19)+CCL21+CXCL13+ receptor activator of NF-κB ligand (RANKL)+LTβR+ mucosal vascular addressin cell adhesion molecule 1 (MADCAM1)+ lymphoid tissue organizer cells (LTo cells). Although it is still unclear precisely how LTo cells relate to mature FRCs, an immature FRC subset has been identified that requires LTβR signalling for the acquisition of an immunologically mature phenotype.
-
FRCs give lymph nodes the flexibility to stretch and to contract to accommodate the trapping of naive lymphocytes during an active immune response. Podoplanin (PDPN) maintains tension in the FRC network during homeostatic conditions, and this function is inhibited during an immune response when an influx of dendritic cells expressing C-type lectin domain family 1 member B (commonly known as CLEC2) inhibits PDPN-mediated FRC contractility.
-
During a chronic infection such as with HIV-1, regulatory T cells upregulate transforming growth factor-β1 (TGFβ1) production, which signals to FRCs to markedly increase their extracellular matrix production. Naive T cells can no longer physically contact FRCs and lose access to IL-7, which results in widespread T cell death and prolonged immunodeficiency.
-
Therapeutic advances seeking to mimic or target FRC function include antifibrotic drugs to reverse lymph node fibrosis, the administration of recombinant IL-7 to support T cell recovery after immunodepletion, and the use of FRCs as a putative anti-inflammatory cell therapy.
Abstract
Over the past decade, a series of discoveries relating to fibroblastic reticular cells (FRCs) — immunologically specialized myofibroblasts found in lymphoid tissue — has promoted these cells from benign bystanders to major players in the immune response. In this Review, we focus on recent advances regarding the immunobiology of lymph node-derived FRCs, presenting an updated view of crucial checkpoints during their development and their dynamic control of lymph node expansion and contraction during infection. We highlight the robust effects of FRCs on systemic B cell and T cell responses, and we present an emerging view of FRCs as drivers of pathology following acute and chronic viral infections. Lastly, we review emerging therapeutic advances that harness the immunoregulatory properties of FRCs.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Link, A. et al. Fibroblastic reticular cells in lymph nodes regulate the homeostasis of naive T cells. Nature Immunol. 8, 1255–1265 (2007). This paper identifies T cell zone reticular cells in lymph nodes as a major source of IL-7 and reveals their importance in maintaining naive T cell survival.
Malhotra, D. et al. Transcriptional profiling of stroma from inflamed and resting lymph nodes defines immunological hallmarks. Nature Immunol. 13, 499–510 (2012). This paper describes the transcriptional characteristics of lymph node stromal cell subsets and the relationship between FRCs and fibroblasts from other locations.
Katakai, T., Hara, T., Sugai, M., Gonda, H. & Shimizu, A. Lymph node fibroblastic reticular cells construct the stromal reticulum via contact with lymphocytes. J. Exp. Med. 200, 783–795 (2004).
Bajenoff, M. et al. Stromal cell networks regulate lymphocyte entry, migration and territoriality in lymph nodes. Immunity 25, 989–1001 (2006).
Roozendaal, R. et al. Conduits mediate transport of low-molecular-weight antigen to lymph node follicles. Immunity 30, 264–276 (2009).
Heesters, B. A., Myers, R. C. & Carroll, M. C. Follicular dendritic cells: dynamic antigen libraries. Nature Rev. Immunol. 14, 495–504 (2014).
Fletcher, A. L. et al. Reproducible isolation of lymph node stromal cells reveals site-dependent differences in fibroblastic reticular cells. Front. Immunol. 2, 35 (2011).
Katakai, T. et al. Organizer-like reticular stromal cell layer common to adult secondary lymphoid organs. J. Immunol. 181, 6189–6200 (2008).
Gretz, J. E., Norbury, C. C., Anderson, A. O., Proudfoot, A. E. I. & Shaw, S. Lymph-borne chemokines and other low molecular weight molecules reach high endothelial venules via specialized conduits while a functional barrier limits access to the lymphocyte microenvironments in lymph node cortex. J. Exp. Med. 192, 1425–1440 (2000). This is the first paper to describe lymph node conduits and the principle of size exclusion that enables small molecules to rapidly diffuse into the deep cortex of the lymph node.
Malhotra, D., Fletcher, A. L. & Turley, S. J. Stromal and hematopoietic cells in secondary lymphoid organs: partners in immunity. Immunol. Rev. 251, 160–176 (2013).
Benezech, C. et al. Ontogeny of stromal organizer cells during lymph node development. J. Immunol. 184, 4521–4530 (2010).
Katakai, T. et al. A novel reticular stromal structure in lymph node cortex: an immuno-platform for interactions among dendritic cells, T cells and B cells. Int. Immunol. 16, 1133–1142 (2004).
Jarjour, M. et al. Fate mapping reveals origin and dynamics of lymph node follicular dendritic cells. J. Exp. Med. 211, 1109–1122 (2014). This paper reports that lymph node FDCs arise from the proliferation and the differentiation of marginal reticular cells.
Van de Pavert, S. A. et al. Chemokine CXCL13 is essential for lymph node initiation and is induced by retinoic acid and neuronal stimulation. Nature Immunol. 10, 1193–1199 (2009).
Benezech, C. et al. Lymphotoxin-β receptor signaling through NF-κB2-RelB pathway reprograms adipocyte precursors as lymph node stromal cells. Immunity 37, 721–734 (2012). These authors show that adipose tissue can be a source of stromal progenitor cells, which differentiate into various lymph node stromal cell types upon migration to newborn and adult lymph nodes.
Gil-Ortega, M. et al. Native adipose stromal cells egress from adipose tissue in vivo: evidence during lymph node activation. Stem Cells 31, 1309–1320 (2013).
Brendolan, A. & Caamano, J. H. Mesenchymal cell differentiation during lymph node organogenesis. Front. Immunol. 3, 381 (2012).
Luther, S. A., Ansel, K. M. & Cyster, J. G. Overlapping roles of CXCL13, interleukin 7 receptor-α, and CCR7 ligands in lymph node development. J. Exp. Med. 197, 1191–1198 (2003).
Eberl, G. et al. An essential function for the nuclear receptor RORγt in the generation of fetal lymphoid tissue inducer cells. Nature Immunol. 5, 64–73 (2004).
Ansel, K. M. et al. A chemokine-driven positive feedback loop organizes lymphoid follicles. Nature 406, 309–314 (2000).
Vondenhoff, M. F. et al. LTβR signaling induces cytokine expression and up-regulates lymphangiogenic factors in lymph node anlagen. J. Immunol. 182, 5439–5445 (2009).
Yoshida, H. et al. Different cytokines induce surface lymphotoxin-αβ on IL-7 receptor-α cells that differentially engender lymph nodes and Peyer's patches. Immunity 17, 823–833 (2002).
Onder, L. et al. Endothelial cell-specific lymphotoxin-β receptor signaling is critical for lymph node and high endothelial venule formation. J. Exp. Med. 210, 465–473 (2013).
Benezech, C. et al. CLEC-2 is required for development and maintenance of lymph nodes. Blood 123, 3200–3207 (2014).
Peters, A. et al. TH17 cells induce ectopic lymphoid follicles in central nervous system tissue inflammation. Immunity 35, 986–996 (2011).
Chai, Q. et al. Maturation of lymph node fibroblastic reticular cells from myofibroblastic precursors is critical for antiviral immunity. Immunity 38, 1013–1024 (2013).
Zeng, M. et al. Critical role of CD4 T cells in maintaining lymphoid tissue structure for immune cell homeostasis and reconstitution. Blood 120, 1856–1867 (2012).
Ngo, V. N., Cornall, R. J. & Cyster, J. G. Splenic T zone development is B cell dependent. J. Exp. Med. 194, 1649–1660 (2001).
Yang, C. Y. et al. Trapping of naive lymphocytes triggers rapid growth and remodeling of the fibroblast network in reactive murine lymph nodes. Proc. Natl Acad. Sci. USA 111, E109–E118 (2014).
Mionnet, C. et al. Identification of a new stromal cell type involved in the regulation of inflamed B cell follicles. PLoS Biol. 11, e1001672 (2013). This paper describes how a subset of T cell zone reticular cells, with a history of CD21 expression, differentiates into CXCL13+ B cell zone reticular cells to control the expanded boundaries of B cell follicles upon inflammation.
Katakai, T. Marginal reticular cells: a stromal subset directly descended from the lymphoid tissue organizer. Front. Immunol. 3, 200 (2012).
Krautler, N. J. et al. Follicular dendritic cells emerge from ubiquitous perivascular precursors. Cell 150, 194–206 (2012).
Denton, A. E., Roberts, E. W., Linterman, M. A. & Fearon, D. T. Fibroblastic reticular cells of the lymph node are required for retention of resting but not activated CD8+ T cells. Proc. Natl Acad. Sci. USA 111, 12139–12144 (2014).
Ame-Thomas, P. et al. Human mesenchymal stem cells isolated from bone marrow and lymphoid organs support tumor B cell growth: role of stromal cells in follicular lymphoma pathogenesis. Blood 109, 693–702 (2007).
Wang, X. et al. Follicular dendritic cells help establish follicle identity and promote B cell retention in germinal centers. J. Exp. Med. 208, 2497–2510 (2011).
Cremasco, V. et al. B cell homeostasis and follicle confines are governed by fibroblastic reticular cells. Nature Immunol. 15, 973–981 (2014). This paper reports that BAFF expression by B cell zone reticular cells supports B cell homeostasis.
Lammermann, T. et al. Rapid leukocyte migration by integrin-independent flowing and squeezing. Nature 453, 51–55 (2008).
Acton, S. E. et al. Podoplanin-rich stromal networks induce dendritic cell motility via activation of the C-type lectin receptor CLEC-2. Immunity 37, 276–289 (2012).
Chyou, S. et al. Fibroblast-type reticular stromal cells regulate the lymph node vasculature. J. Immunol. 181, 3887–3896 (2008).
Herzog, B. H. et al. Podoplanin maintains high endothelial venule integrity by interacting with platelet CLEC-2. Nature 502, 105–109 (2013). These authors show that PDPN+ FRCs maintain the integrity of HEVs through interactions with CLEC2-bearing platelets.
Lee, J. W. et al. Peripheral antigen display by lymph node stroma promotes T cell tolerance to intestinal self. Nature Immunol. 8, 181–190 (2007).
Nichols, L. A. et al. Deletional self-tolerance to a melanocyte/melanoma antigen derived from tyrosinase is mediated by a radio-resistant cell in peripheral and mesenteric lymph nodes. J. Immunol. 179, 993–1003 (2007).
Magnusson, F. C. et al. Direct presentation of antigen by lymph node stromal cells protects against CD8 T cell-mediated intestinal autoimmunity. Gastroenterology 134, 1028–1037 (2008).
Yip, L. et al. Deaf1 isoforms control the expression of genes encoding peripheral tissue antigens in the pancreatic lymph nodes during type 1 diabetes. Nature Immunol. 10, 1026–1033 (2009).
Fletcher, A. L. et al. Lymph node fibroblastic reticular cells directly present peripheral tissue antigen under steady-state and inflammatory conditions. J. Exp. Med. 207, 689–697 (2010).
Cohen, J. N. et al. Lymph node-resident lymphatic endothelial cells mediate peripheral tolerance via Aire-independent direct antigen presentation. J. Exp. Med. 207, 681–688 (2010).
Mueller, S. N. et al. Viral targeting of fibroblastic reticular cells contributes to immunosuppression and persistence during chronic infection. Proc. Natl Acad. Sci. USA 104, 15430–15435 (2007).
Lukacs-Kornek, V. et al. Regulated release of nitric oxide by nonhematopoietic stroma controls expansion of the activated T cell pool in lymph nodes. Nature Immunol. 12, 1096–1104 (2011).
Siegert, S. et al. Fibroblastic reticular cells from lymph nodes attenuate T cell expansion by producing nitric oxide. PLoS ONE 6, e27618 (2011).
Khan, O. et al. Regulation of T cell priming by lymphoid stroma. PLoS ONE 6, e26138 (2011).
Dubrot, J. et al. Lymph node stromal cells acquire peptide–MHCII complexes from dendritic cells and induce antigen-specific CD4+ T cell tolerance. J. Exp. Med. 211, 1153–1166 (2014). This paper shows that FRCs tolerize CD4+ T cells through antigen presentation via peptide–MHC class II complexes that are acquired directly from DCs.
Baptista, A. P. et al. Lymph node stromal cells constrain immunity via MHC class II self-antigen presentation. eLife 3, e04433 (2014).
Suenaga, F. et al. Loss of lymph node fibroblastic reticular cells and high endothelial cells is associated with humoral immunodeficiency in mouse graft-versus-host disease. J. Immunol. 194, 398–406 (2014).
Cording, S. et al. The intestinal micro-environment imprints stromal cells to promote efficient TReg induction in gut-draining lymph nodes. Mucosal Immunol. 7, 359–368 (2014).
Fletcher, A. L., Malhotra, D. & Turley, S. J. Lymph node stroma broaden the peripheral tolerance paradigm. Trends Immunol. 32, 12–18 (2011).
Acton, S. E. et al. Dendritic cells control fibroblastic reticular network tension and lymph node expansion. Nature 514, 498–502 (2014). This paper shows how interactions between DCs and FRCs control lymph node flexibility, thereby regulating lymph node expansion during an immune response.
Astarita, J. L. et al. The CLEC-2-podoplanin axis controls the contractility of fibroblastic reticular cells and lymph node microarchitecture. Nature Immunol. 16, 75–84 (2015). This paper shows how PDPN expression by FRCs controls stromal cell network morphology and lymph node expansion during an immune response.
Chyou, S. et al. Coordinated regulation of lymph node vascular-stromal growth first by CD11c+ cells and then by T and B cells. J. Immunol. 187, 5558–5567 (2011).
Pollitt, A. Y. et al. Syk and Src family kinases regulate CLEC-2 mediated clustering of podoplanin and platelet adhesion to lymphatic endothelial cells. J. Biol. Chem. 289, 35695–35710 (2014).
Hess, E. et al. RANKL induces organized lymph node growth by stromal cell proliferation. J. Immunol. 188, 1245–1254 (2012).
Lange, A. W. et al. Hippo/Yap signaling controls epithelial progenitor cell proliferation and differentiation in the embryonic and adult lung. J. Mol. Cell. Biol. 7, 35–47 (2014).
Steele, K. E., Anderson, A. O. & Mohamadzadeh, M. Fibroblastic reticular cell infection by hemorrhagic fever viruses. Immunotherapy 1, 187–197 (2009).
Twenhafel, N. A. et al. Pathology of experimental aerosol Zaire ebolavirus infection in rhesus macaques. Vet. Pathol. 50, 514–529 (2013).
Steele, K. E., Anderson, A. O. & Mohamadzadeh, M. Fibroblastic reticular cells and their role in viral hemorrhagic fevers. Expert Rev. Anti Infect. Ther. 7, 423–435 (2009).
Ng, C. T., Nayak, B. P., Schmedt, C. & Oldstone, M. B. Immortalized clones of fibroblastic reticular cells activate virus-specific T cells during virus infection. Proc. Natl Acad. Sci. USA 109, 7823–7828 (2012).
Scandella, E. et al. Restoration of lymphoid organ integrity through the interaction of lymphoid tissue-inducer cells with stroma of the T cell zone. Nature Immunol. 9, 667–675 (2008).
Mueller, S. N. et al. PD-L1 has distinct functions in hematopoietic and nonhematopoietic cells in regulating T cell responses during chronic infection in mice. J. Clin. Invest. 120, 2508–2515 (2010).
Estes, J. et al. Collagen deposition limits immune reconstitution in the gut. J. Infect. Dis. 198, 456–464 (2008).
Zeng, M. et al. Cumulative mechanisms of lymphoid tissue fibrosis and T cell depletion in HIV-1 and SIV infections. J. Clin. Invest. 121, 998–1008 (2011).
Estes, J. D. et al. Antifibrotic therapy in simian immunodeficiency virus infection preserves CD4+ T cell populations and improves immune reconstitution with antiretroviral therapy. J. Infect. Dis. 211, 744–754 (2014).
Estes, J. D. Pathobiology of HIV/SIV-associated changes in secondary lymphoid tissues. Immunol. Rev. 254, 65–77 (2013).
Guihot, A., Bourgarit, A., Carcelain, G. & Autran, B. Immune reconstitution after a decade of combined antiretroviral therapies for human immunodeficiency virus. Trends Immunol. 32, 131–137 (2011).
Horta, A. et al. Poor immune reconstitution in HIV-infected patients associates with high percentage of regulatory CD4+ T cells. PLoS ONE 8, e57336 (2013).
Onder, L. et al. IL-7-producing stromal cells are critical for lymph node remodeling. Blood 120, 4675–4683 (2012).
Perales, M. A. et al. Recombinant human interleukin-7 (CYT107) promotes T-cell recovery after allogeneic stem cell transplantation. Blood 120, 4882–4891 (2012).
Fletcher, A. L. et al. Lymph node fibroblastic reticular cell transplants show robust therapeutic efficacy in high-mortality murine sepsis. Sci. Transl. Med. 6, 249ra109 (2014).
Wang, Y., Chen, X., Cao, W. & Shi, Y. Plasticity of mesenchymal stem cells in immunomodulation: pathological and therapeutic implications. Nature Immunol. 15, 1009–1016 (2014).
Fasnacht, N. et al. Specific fibroblastic niches in secondary lymphoid organs orchestrate distinct Notch-regulated immune responses. J. Exp. Med. 211, 2265–2279 (2014).
Cupedo, T. et al. Presumptive lymph node organizers are differentially represented in developing mesenteric and peripheral nodes. J. Immunol. 173, 2968–2975 (2004).
Ohl, L. et al. Cooperating mechanisms of CXCR5 and CCR7 in development and organization of secondary lymphoid organs. J. Exp. Med. 197, 1199–1204 (2003).
Carragher, D. et al. A stroma-derived defect in NF-κB2−/− mice causes impaired lymph node development and lymphocyte recruitment. J. Immunol. 173, 2271–2279 (2004).
Drayton, D. L. et al. IκB kinase complex α kinase activity controls chemokine and high endothelial venule gene expression in lymph nodes and nasal-associated lymphoid tissue. J. Immunol. 173, 6161–6168 (2004).
Mourao-Sa, D. et al. CLEC-2 signaling via Syk in myeloid cells can regulate inflammatory responses. Eur. J. Immunol. 41, 3040–3053 (2011).
Acknowledgements
This work was supported by a Birmingham Fellowship (to A.L.F.) and a Henry Wellcome Fellowship (to S.E.A.). The authors thank J. Caamano for thoughtful suggestions on the manuscript and apologise to others whose work was not cited in this Review owing to space limitations.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
A.L.F. is an inventor on a patent related to the therapeutic use of fibroblastic reticular cells. S.E.A. and K.K. declare no competing interests.
Related links
DATABASES
Glossary
- Myofibroblasts
-
Cells that share characteristics with fibroblasts and smooth muscle cells and that are often associated with the response to inflammation.
- Follicular dendritic cells
-
(FDCs). Non-haematopoietic stromal cells found in B cell follicles that have an important role in antigen presentation to B cells.
- Lymphoid tissue organizer cells
-
(LTo cells). CXC-chemokine ligand 13 (CXCL13)+ lymphotoxin-β receptor (LTβR)+ podoplanin (PDPN)+CD45− mesenchymal stromal cells that engage in molecular crosstalk with lymphoid tissue inducer cells to induce lymph node formation.
- Lymphoid tissue inducer cells
-
(LTi cells; a subset of group 3 innate lymphoid cells). CD3−CD4+CD45+ innate lymphocytes that engage in crucial, carefully regulated molecular crosstalk with non-haematopoietic lymphoid tissue organizer cells to induce lymph node formation. Their development is dependent on the transcription factor retinoic acid receptor-related orphan receptor-γt (RORγt).
- Autoimmune regulator
-
(AIRE). A transcriptional modulator primarily expressed by thymic medullary epithelial cells, in which it enhances the transcription of tissue-restricted antigens. This facilitates T cell education, by enabling developing T cells to encounter a large range of self proteins.
- Ezrin, radixin and moesin family proteins
-
(ERM family proteins). Proteins that link the plasma membrane to the actin cytoskeleton. They are involved in cell adhesion, contraction and cortical morphogenesis.
- Ccl19–Cre × Ltbrfl/fl mice
-
A BAC transgenic mouse model using CC-chemokine ligand 19 (Ccl19) promoter activity to target Cre recombinase to fibroblastic reticular cells and related cells. When crossed to the Ltbrfl/fl mouse, Cre recombinase deletes the lymphotoxin-β receptor (Ltbr) gene in any CCL19+ cells at the moment that CCL19 becomes upregulated.
- Ccl19–Cre × iDTR mice
-
A BAC transgenic mouse model using CC-chemokine ligand 19 (Ccl19) promoter activity to target Cre recombinase to fibroblastic reticular cells (FRCs) and related cells. When crossed to the Cre-inducible diphtheria toxin receptor (iDTR) mouse, administration of diphtheria toxin depletes CCL19+ cells, including FRCs.
Rights and permissions
About this article
Cite this article
Fletcher, A., Acton, S. & Knoblich, K. Lymph node fibroblastic reticular cells in health and disease. Nat Rev Immunol 15, 350–361 (2015). https://doi.org/10.1038/nri3846
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri3846
This article is cited by
-
Whole-body cellular mapping in mouse using standard IgG antibodies
Nature Biotechnology (2024)
-
The cervical lymph node contributes to peripheral inflammation related to Parkinson’s disease
Journal of Neuroinflammation (2023)
-
The immunoregulatory roles of non-haematopoietic cells in the kidney
Nature Reviews Nephrology (2023)
-
The aging of the immune system and its implications for transplantation
GeroScience (2023)
-
Loss of vascular endothelial notch signaling promotes spontaneous formation of tertiary lymphoid structures
Nature Communications (2022)