Abstract
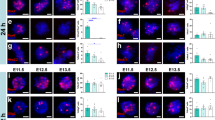
The corticospinal tract (CST) is the most important motor system in humans, yet robust regeneration of this projection after spinal cord injury (SCI) has not been accomplished. In murine models of SCI, we report robust corticospinal axon regeneration, functional synapse formation and improved skilled forelimb function after grafting multipotent neural progenitor cells into sites of SCI. Corticospinal regeneration requires grafts to be driven toward caudalized (spinal cord), rather than rostralized, fates. Fully mature caudalized neural grafts also support corticospinal regeneration. Moreover, corticospinal axons can emerge from neural grafts and regenerate beyond the lesion, a process that is potentially related to the attenuation of the glial scar. Rat corticospinal axons also regenerate into human donor grafts of caudal spinal cord identity. Collectively, these findings indicate that spinal cord 'replacement' with homologous neural stem cells enables robust regeneration of the corticospinal projection within and beyond spinal cord lesion sites, achieving a major unmet goal of SCI research and offering new possibilities for clinical translation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Liu, K., Tedeschi, A., Park, K.K. & He, Z. Neuronal intrinsic mechanisms of axon regeneration. Annu. Rev. Neurosci. 34, 131–152 (2011).
Tuszynski, M.H. & Steward, O. Concepts and methods for the study of axonal regeneration in the CNS. Neuron 74, 777–791 (2012).
Bareyre, F.M. et al. The injured spinal cord spontaneously forms a new intraspinal circuit in adult rats. Nat. Neurosci. 7, 269–277 (2004).
Rosenzweig, E.S. et al. Extensive spontaneous plasticity of corticospinal projections after primate spinal cord injury. Nat. Neurosci. 13, 1505–1510 (2010).
Weidner, N., Ner, A., Salimi, N. & Tuszynski, M.H. Spontaneous corticospinal axonal plasticity and functional recovery after adult central nervous system injury. Proc. Natl. Acad. Sci. USA 98, 3513–3518 (2001).
Schnell, L. & Schwab, M.E. Axonal regeneration in the rat spinal cord produced by an antibody against myelin-associated neurite growth inhibitors. Nature 343, 269–272 (1990).
GrandPré, T., Li, S. & Strittmatter, S.M. Nogo-66 receptor antagonist peptide promotes axonal regeneration. Nature 417, 547–551 (2002).
Liu, K. et al. PTEN deletion enhances the regenerative ability of adult corticospinal neurons. Nat. Neurosci. 13, 1075–1081 (2010).
Zukor, K. et al. Short hairpin RNA against PTEN enhances regenerative growth of corticospinal tract axons after spinal cord injury. J. Neurosci. 33, 15350–15361 (2013).
Ohtake, Y. et al. The effect of systemic PTEN antagonist peptides on axon growth and functional recovery after spinal cord injury. Biomaterials 35, 4610–4626 (2014).
Starkey, M.L. & Schwab, M.E. Anti-Nogo-A and training: can one plus one equal three? Exp. Neurol. 235, 53–61 (2012).
Hollis, E.R. II, Jamshidi, P., Löw, K., Blesch, A. & Tuszynski, M.H. Induction of corticospinal regeneration by lentiviral trkB-induced Erk activation. Proc. Natl. Acad. Sci. USA 106, 7215–7220 (2009).
Xu, X.M., Guénard, V., Kleitman, N., Aebischer, P. & Bunge, M.B. A combination of BDNF and NT-3 promotes supraspinal axonal regeneration into Schwann cell grafts in adult rat thoracic spinal cord. Exp. Neurol. 134, 261–272 (1995).
Vavrek, R., Pearse, D.D. & Fouad, K. Neuronal populations capable of regeneration following a combined treatment in rats with spinal cord transection. J. Neurotrauma 24, 1667–1673 (2007).
Lu, P. et al. Motor axonal regeneration after partial and complete spinal cord transection. J. Neurosci. 32, 8208–8218 (2012).
Lee, Y.S. et al. Nerve regeneration restores supraspinal control of bladder function after complete spinal cord injury. J. Neurosci. 33, 10591–10606 (2013).
Cummings, B.J. et al. Human neural stem cells differentiate and promote locomotor recovery in spinal cord–injured mice. Proc. Natl. Acad. Sci. USA 102, 14069–14074 (2005).
Bonner, J.F. et al. Grafted neural progenitors integrate and restore synaptic connectivity across the injured spinal cord. J. Neurosci. 31, 4675–4686 (2011).
Lu, P. et al. Long-distance growth and connectivity of neural stem cells after severe spinal cord injury. Cell 150, 1264–1273 (2012).
Lu, P. et al. Long-distance axonal growth from human induced pluripotent stem cells after spinal cord injury. Neuron 83, 789–796 (2014).
Peljto, M., Dasen, J.S., Mazzoni, E.O., Jessell, T.M. & Wichterle, H. Functional diversity of ESC-derived motor neuron subtypes revealed through intraspinal transplantation. Cell Stem Cell 7, 355–366 (2010).
Ma, L. et al. Human embryonic stem cell–derived GABA neurons correct locomotion deficits in quinolinic acid-lesioned mice. Cell Stem Cell 10, 455–464 (2012).
Mayer-Proschel, M., Kalyani, A.J., Mujtaba, T. & Rao, M.S. Isolation of lineage-restricted neuronal precursors from multipotent neuroepithelial stem cells. Neuron 19, 773–785 (1997).
Du Beau, A. et al. Neurotransmitter phenotypes of descending systems in the rat lumbar spinal cord. Neuroscience 227, 67–79 (2012).
Perry, R.B. et al. Subcellular knockout of importin β1 perturbs axonal retrograde signaling. Neuron 75, 294–305 (2012).
Cho, Y., Sloutsky, R., Naegle, K.M. & Cavalli, V. Injury-induced HDAC5 nuclear export is essential for axon regeneration. Cell 155, 894–908 (2013).
Fawcett, J.W., Schwab, M.E., Montani, L., Brazda, N. & Müller, H.W. Defeating inhibition of regeneration by scar and myelin components. Handb. Clin. Neurol. 109, 503–522 (2012).
Liu, Y. & Rao, M.S. Glial progenitors in the CNS and possible lineage relationships among them. Biol. Cell 96, 279–290 (2004).
Cao, Q.L., Howard, R.M., Dennison, J.B. & Whittemore, S.R. Differentiation of engrafted neuronal-restricted precursor cells is inhibited in the traumatically injured spinal cord. Exp. Neurol. 177, 349–359 (2002).
García-Alías, G., Barkhuysen, S., Buckle, M. & Fawcett, J.W. Chondroitinase ABC treatment opens a window of opportunity for task-specific rehabilitation. Nat. Neurosci. 12, 1145–1151 (2009).
Conner, J.M., Chiba, A.A. & Tuszynski, M.H. The basal forebrain cholinergic system is essential for cortical plasticity and functional recovery following brain injury. Neuron 46, 173–179 (2005).
Montoya, C.P., Campbell-Hope, L.J., Pemberton, K.D. & Dunnett, S.B. The “staircase test”: a measure of independent forelimb reaching and grasping abilities in rats. J. Neurosci. Methods 36, 219–228 (1991).
Wahl, A.S. et al. Neuronal repair. Asynchronous therapy restores motor control by rewiring of the rat corticospinal tract after stroke. Science 344, 1250–1255 (2014).
Alaverdashvili, M. & Whishaw, I.Q. Motor cortex stroke impairs individual digit movement in skilled reaching by the rat. Eur. J. Neurosci. 28, 311–322 (2008).
Whishaw, I.Q., Gorny, B. & Sarna, J. Paw and limb use in skilled and spontaneous reaching after pyramidal tract, red nucleus and combined lesions in the rat: behavioral and anatomical dissociations. Behav. Brain Res. 93, 167–183 (1998).
Girgis, J. et al. Reaching training in rats with spinal cord injury promotes plasticity and task specific recovery. Brain 130, 2993–3003 (2007).
Krajacic, A., Weishaupt, N., Girgis, J., Tetzlaff, W. & Fouad, K. Training-induced plasticity in rats with cervical spinal cord injury: effects and side effects. Behav. Brain Res. 214, 323–331 (2010).
Steward, O., Sharp, K.G. & Matsudaira Yee, K. Long-distance migration and colonization of transplanted neural stem cells. Cell 156, 385–387 (2014).
Tuszynski, M.H. et al. Neural stem cell dissemination after grafting to CNS injury sites. Cell 156, 388–389 (2014).
Tuszynski, M.H. et al. Neural stem cells in models of spinal cord injury. Exp. Neurol. 261, 494–500 (2014).
Steward, O., Sharp, K.G., Yee, K.M., Hatch, M.N. & Bonner, J.F. Characterization of ectopic colonies that form in widespread areas of the nervous system with neural stem cell transplants into the site of a severe spinal cord injury. J. Neurosci. 34, 14013–14021 (2014).
Garcia-Ovejero, D. et al. The ependymal region of the adult human spinal cord differs from other species and shows ependymoma-like features. Brain 138, 1583–1597 (2015).
Conti, L. & Cattaneo, E. Neural stem cell systems: physiological players or in vitro entities? Nat. Rev. Neurosci. 11, 176–187 (2010).
Chen, H. et al. Human-derived neural progenitors functionally replace astrocytes in adult mice. J. Clin. Invest. 125, 1033–1042 (2015).
Blackmore, M.G. et al. Krüppel-like Factor 7 engineered for transcriptional activation promotes axon regeneration in the adult corticospinal tract. Proc. Natl. Acad. Sci. USA 109, 7517–7522 (2012).
Norenberg, M.D., Smith, J. & Marcillo, A. The pathology of human spinal cord injury: defining the problems. J. Neurotrauma 21, 429–440 (2004).
Coumans, J.V. et al. Axonal regeneration and functional recovery after complete spinal cord transection in rats by delayed treatment with transplants and neurotrophins. J. Neurosci. 21, 9334–9344 (2001).
Molofsky, A.V. et al. Astrocyte-encoded positional cues maintain sensorimotor circuit integrity. Nature 509, 189–194 (2014).
Wu, Y., Liu, Y., Chesnut, J.D. & Rao, M.S. Isolation of neural stem and precursor cells from rodent tissue. Methods Mol. Biol. 438, 39–53 (2008).
Thomson, J.A. et al. Embryonic stem cell lines derived from human blastocysts. Science 282, 1145–1147 (1998).
Yu, J. et al. Induced pluripotent stem cell lines derived from human somatic cells. Science 318, 1917–1920 (2007).
Zhang, S.C., Wernig, M., Duncan, I.D., Brüstle, O. & Thomson, J.A. In vitro differentiation of transplantable neural precursors from human embryonic stem cells. Nat. Biotechnol. 19, 1129–1133 (2001).
Hu, B.Y. & Zhang, S.C. Differentiation of spinal motor neurons from pluripotent human stem cells. Nat. Protoc. 4, 1295–1304 (2009).
Weidner, N., Blesch, A., Grill, R.J. & Tuszynski, M.H. Nerve growth factor–hypersecreting Schwann cell grafts augment and guide spinal cord axonal growth and remyelinate central nervous system axons in a phenotypically appropriate manner that correlates with expression of L1. J. Comp. Neurol. 413, 495–506 (1999).
Kadoya, K. et al. Combined intrinsic and extrinsic neuronal mechanisms facilitate bridging axonal regeneration one year after spinal cord injury. Neuron 64, 165–172 (2009).
Jones, L.L. & Tuszynski, M.H. Spinal cord injury elicits expression of keratan sulfate proteoglycans by macrophages, reactive microglia, and oligodendrocyte progenitors. J. Neurosci. 22, 4611–4624 (2002).
Wang, D., Ichiyama, R.M., Zhao, R., Andrews, M.R. & Fawcett, J.W. Chondroitinase combined with rehabilitation promotes recovery of forelimb function in rats with chronic spinal cord injury. J. Neurosci. 31, 9332–9344 (2011).
Acknowledgements
We thank L. Graham, Y. Yang, E. Boehle, J.K. Lee, M. Kim, E. Liu, R. Pope and T. Moynihan for their technical assistance; Planned Parenthood; the Rat Resource and Research Center, University of Missouri, Columbia, Missouri, for providing GFP rats; James Thompson at the University of Wisconsin–Madison, for providing hiPSC line IMR90; K. Wewetzer, University of Freiburg, Germany, for providing 27C7 antibody; R. Darnell, the Rockefeller University, New York, for providing Hu antibody; Y. Jones for use of the electron-microscopy core facility at Cellular and Molecular Medicine, University of California, San Diego; and the Nikon Imaging Center at Hokkaido University for use of the confocal laser microscope. This work was supported by the US Veterans Administration (Gordon Mansfield Spinal Cord Injury Consortium; to M.H.T. and P.L.) the US National Institutes of Health (NS042291 to M.H.T. and GM008349 to J.K.); the Craig H. Neilsen Foundation (to K.K., H.K. and J.N.D.); the Bernard and Anne Spitzer Charitable Trust (to M.H.T.); the Dr. Miriam and Sheldon G. Adelson Medical Research Foundation (to M.H.T. and J.C.); Kobayashi Hospital Furate Research Fund (to K.K.); the Japan Society for the Promotion of Science (to H.K.); and the Busta Family and Bleser Family funds (to S.C.Z.).
Author information
Authors and Affiliations
Contributions
K.K. conceived and carried out experiments, interpreted the results and wrote the manuscript. P.L. contributed to the conception of the project and performed complete-transection experiments. K.N. and H.S. carried out experiments. C.L.-K. and J.N.D. contributed to behavior analysis. G.P. contributed to mouse experiments. H.K. contributed to the characterization of human NPCs. L.Y., J.K. and S.-C.Z. contributed to the generation of human NPCs from iPSCs. J.B., Y.T. and J.C. performed the electrophysiological analysis. M.H.T. contributed to the conception of the project and the interpretation of results, and wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Supplementary Text and Figures
Supplementary Figures 1–7 and Supplementary Table 1 (PDF 20425 kb)
Rights and permissions
About this article
Cite this article
Kadoya, K., Lu, P., Nguyen, K. et al. Spinal cord reconstitution with homologous neural grafts enables robust corticospinal regeneration. Nat Med 22, 479–487 (2016). https://doi.org/10.1038/nm.4066
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/nm.4066
This article is cited by
-
Generation of functional posterior spinal motor neurons from hPSCs-derived human spinal cord neural progenitor cells
Cell Regeneration (2023)
-
Regulation of axonal regeneration after mammalian spinal cord injury
Nature Reviews Molecular Cell Biology (2023)
-
Human induced neural stem cells support functional recovery in spinal cord injury models
Experimental & Molecular Medicine (2023)
-
MLL1 inhibits the neurogenic potential of SCAPs by interacting with WDR5 and repressing HES1
International Journal of Oral Science (2023)
-
Developmental stage of transplanted neural progenitor cells influences anatomical and functional outcomes after spinal cord injury in mice
Communications Biology (2023)