Abstract
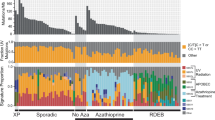
We characterized the mutational landscape of melanoma, the form of skin cancer with the highest mortality rate, by sequencing the exomes of 147 melanomas. Sun-exposed melanomas had markedly more ultraviolet (UV)-like C>T somatic mutations compared to sun-shielded acral, mucosal and uveal melanomas. Among the newly identified cancer genes was PPP6C, encoding a serine/threonine phosphatase, which harbored mutations that clustered in the active site in 12% of sun-exposed melanomas, exclusively in tumors with mutations in BRAF or NRAS. Notably, we identified a recurrent UV-signature, an activating mutation in RAC1 in 9.2% of sun-exposed melanomas. This activating mutation, the third most frequent in our cohort of sun-exposed melanoma after those of BRAF and NRAS, changes Pro29 to serine (RAC1P29S) in the highly conserved switch I domain. Crystal structures, and biochemical and functional studies of RAC1P29S showed that the alteration releases the conformational restraint conferred by the conserved proline, causes an increased binding of the protein to downstream effectors, and promotes melanocyte proliferation and migration. These findings raise the possibility that pharmacological inhibition of downstream effectors of RAC1 signaling could be of therapeutic benefit.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Bauer, J. et al. BRAF mutations in cutaneous melanoma are independently associated with age, anatomic site of the primary tumor, and the degree of solar elastosis at the primary tumor site. Pigment Cell Melanoma Res. 24, 345–351 (2011).
Bollag, G. et al. Clinical efficacy of a RAF inhibitor needs broad target blockade in BRAF-mutant melanoma. Nature 467, 596–599 (2010).
Chapman, P.B. et al. Improved survival with vemurafenib in melanoma with BRAF V600E mutation. N. Engl. J. Med. 364, 2507–2516 (2011).
Ribas, A. & Flaherty, K.T. BRAF targeted therapy changes the treatment paradigm in melanoma. Nat. Rev. Clin. Oncol. 8, 426–433 (2011).
Jakob, J.A. et al. NRAS mutation status is an independent prognostic factor in metastatic melanoma. Cancer published online, doi:10.1002/cncr.26724 (16 December 2011).
Pleasance, E.D. et al. A comprehensive catalogue of somatic mutations from a human cancer genome. Nature 463, 191–196 (2010).
Nikolaev, S.I. et al. Exome sequencing identifies recurrent somatic MAP2K1 and MAP2K2 mutations in melanoma. Nat. Genet. 44, 133–139 (2012).
Wei, X. et al. Exome sequencing identifies GRIN2A as frequently mutated in melanoma. Nat. Genet. 43, 442–446 (2011).
Berger, M.F. et al. Melanoma genome sequencing reveals frequent PREX2 mutations. Nature 485, 502–506 (2012).
Curtin, J.A. et al. Distinct sets of genetic alterations in melanoma. N. Engl. J. Med. 353, 2135–2147 (2005).
Brash, D.E. & Haseltine, W.A. UV-induced mutation hotspots occur at DNA damage hotspots. Nature 298, 189–192 (1982).
Bernet, A. & Fitamant, J. Netrin-1 and its receptors in tumour growth promotion. Expert Opin. Ther. Targets 12, 995–1007 (2008).
Solomon, D.A. et al. Mutational inactivation of PTPRD in glioblastoma multiforme and malignant melanoma. Cancer Res. 68, 10300–10306 (2008).
Stark, M.S. et al. Frequent somatic mutations in MAP3K5 and MAP3K9 in metastatic melanoma identified by exome sequencing. Nat. Genet. 44, 165–169 (2012).
Sivaram, M.V., Wadzinski, T.L., Redick, S.D., Manna, T. & Doxsey, S.J. Dynein light intermediate chain 1 is required for progress through the spindle assembly checkpoint. EMBO J. 28, 902–914 (2009).
Harbour, J.W. et al. Frequent mutation of BAP1 in metastasizing uveal melanomas. Science 330, 1410–1413 (2010).
Onken, M.D. et al. Loss of heterozygosity of chromosome 3 detected with single nucleotide polymorphisms is superior to monosomy 3 for predicting metastasis in uveal melanoma. Clin. Cancer Res. 13, 2923–2927 (2007).
Li, J. et al. CONTRA: copy number analysis for targeted resequencing. Bioinformatics 28, 1307–1313 (2012).
Whiteman, D.C., Pavan, W.J. & Bastian, B.C. The melanomas: a synthesis of epidemiological, clinical, histopathological, genetic, and biological aspects, supporting distinct subtypes, causal pathways, and cells of origin. Pigment Cell Melanoma Res. 24, 879–897 (2011).
Kabbarah, O. et al. Integrative genome comparison of primary and metastatic melanomas. PLoS ONE 5, e10770 (2010).
Koga, Y. et al. Genome-wide screen of promoter methylation identifies novel markers in melanoma. Genome Res. 19, 1462–1470 (2009).
Halaban, R. et al. Integrative analysis of epigenetic modulation in melanoma cell response to decitabine: clinical implications. PLoS ONE 4, e4563 (2009).
Fears, T.R. et al. Average midrange ultraviolet radiation flux and time outdoors predict melanoma risk. Cancer Res. 62, 3992–3996 (2002).
Wennerberg, K., Rossman, K.L. & Der, C.J. The Ras superfamily at a glance. J. Cell Sci. 118, 843–846 (2005).
Hakoshima, T., Shimizu, T. & Maesaki, R. Structural basis of the Rho GTPase signaling. J. Biochem. 134, 327–331 (2003).
Ménard, L. & Snyderman, R. Role of phosphate-magnesium–binding regions in the high GTPase activity of rac1 protein. Biochemistry 32, 13357–13361 (1993).
Reinstein, J., Schlichting, I., Frech, M., Goody, R.S. & Wittinghofer, A. p21 with a phenylalanine 28→leucine mutation reacts normally with the GTPase activating protein GAP but nevertheless has transforming properties. J. Biol. Chem. 266, 17700–17706 (1991).
Lin, R., Cerione, R.A. & Manor, D. Specific contributions of the small GTPases Rho, Rac, and Cdc42 to Dbl transformation. J. Biol. Chem. 274, 23633–23641 (1999).
Ridley, A.J., Paterson, H.F., Johnston, C.L., Diekmann, D. & Hall, A. The small GTP-binding protein rac regulates growth factor-induced membrane ruffling. Cell 70, 401–410 (1992).
Broekaert, S.M. et al. Genetic and morphologic features for melanoma classification. Pigment Cell Melanoma Res. 23, 763–770 (2010).
Viros, A. et al. Improving melanoma classification by integrating genetic and morphologic features. PLoS Med. 5, e120 (2008).
Crespo-Hernández, C.E., Cohen, B. & Kohler, B. Base stacking controls excited-state dynamics in A.T DNA. Nature 436, 1141–1144 (2005).
Ziegler, A. et al. Mutation hotspots due to sunlight in the p53 gene of nonmelanoma skin cancers. Proc. Natl. Acad. Sci. USA 90, 4216–4220 (1993).
Turajlic, S. et al. Whole genome sequencing of matched primary and metastatic acral melanomas. Genome Res. 22, 196–207 (2012).
Furney, S.J. et al. Genomic characterisation of acral melanoma cell lines. Pigment Cell Melanoma Res. 25, 488–492 (2012).
Li, M. et al. Inactivating mutations of the chromatin remodeling gene ARID2 in hepatocellular carcinoma. Nat. Genet. 43, 828–829 (2011).
Flavell, J.R. et al. Down-regulation of the TGF-β target gene, PTPRK, by the Epstein-Barr virus encoded EBNA1 contributes to the growth and survival of Hodgkin lymphoma cells. Blood 111, 292–301 (2008).
Pollock, P.M. et al. High frequency of BRAF mutations in nevi. Nat. Genet. 33, 19–20 (2003).
Bauer, J., Curtin, J.A., Pinkel, D. & Bastian, B.C. Congenital melanocytic nevi frequently harbor NRAS mutations but no BRAF mutations. J. Invest. Dermatol. 127, 179–182 (2007).
Vredeveld, L.C. et al. Abrogation of BRAFV600E-induced senescence by PI3K pathway activation contributes to melanomagenesis. Genes Dev. 26, 1055–1069 (2012).
Nogueira, C. et al. Cooperative interactions of PTEN deficiency and RAS activation in melanoma metastasis. Oncogene 29, 6222–6232 (2010).
Zeng, K., Bastos, R.N., Barr, F.A. & Gruneberg, U. Protein phosphatase 6 regulates mitotic spindle formation by controlling the T-loop phosphorylation state of Aurora A bound to its activator TPX2. J. Cell Biol. 191, 1315–1332 (2010).
Barr, F.A., Elliott, P.R. & Gruneberg, U. Protein phosphatases and the regulation of mitosis. J. Cell Sci. 124, 2323–2334 (2011).
Douglas, P. et al. Protein phosphatase 6 interacts with the DNA-dependent protein kinase catalytic subunit and dephosphorylates γ-H2AX. Mol. Cell. Biol. 30, 1368–1381 (2010).
Manfredi, M.G. et al. Characterization of Alisertib (MLN8237), an investigational small-molecule inhibitor of aurora A kinase using novel in vivo pharmacodynamic assays. Clin. Cancer Res. 17, 7614–7624 (2011).
Sehdev, V. et al. The Aurora kinase A inhibitor MLN8237 enhances cisplatin-induced cell death in esophageal adenocarcinoma cells. Mol. Cancer Ther. 11, 763–774 (2012).
Jensen, J.S., Omarsdottir, S., Thorsteinsdottir, J.B., Ogmundsdottir, H.M. & Olafsdottir, E.S. Synergistic cytotoxic effect of the microtubule inhibitor marchantin a from marchantia polymorpha and the Aurora kinase inhibitor MLN8237 on breast cancer cells in vitro. Planta Med. 78, 448–454 (2012).
Macarulla, T. et al. Phase I study of the selective Aurora A kinase inhibitor MLN8054 in patients with advanced solid tumors: safety, pharmacokinetics, and pharmacodynamics. Mol. Cancer Ther. 9, 2844–2852 (2010).
Chadee, D.N. et al. Mixed-lineage kinase 3 regulates B-Raf through maintenance of the B-Raf/Raf-1 complex and inhibition by the NF2 tumor suppressor protein. Proc. Natl. Acad. Sci. USA 103, 4463–4468 (2006).
Castets, M. et al. DCC constrains tumour progression via its dependence receptor activity. Nature 482, 534–537 (2012).
Krimpenfort, P. et al. Deleted in colorectal carcinoma suppresses metastasis in p53-deficient mammary tumours. Nature 482, 538–541 (2012).
Stransky, N. et al. The mutational landscape of head and neck squamous cell carcinoma. Science 333, 1157–1160 (2011).
Barretina, J. et al. The Cancer Cell Line Encyclopedia enables predictive modelling of anticancer drug sensitivity. Nature 483, 603–607 (2012).
Li, A. et al. Rac1 drives melanoblast organization during mouse development by orchestrating pseudopod-driven motility and cell-cycle progression. Dev. Cell 21, 722–734 (2011).
Lindsay, C.R. et al. P-Rex1 is required for efficient melanoblast migration and melanoma metastasis. Nat. Commun. 2, 555 (2011).
Xing, Y. et al. Structure of protein phosphatase 2A core enzyme bound to tumor-inducing toxins. Cell 127, 341–353 (2006).
Pai, E.F. et al. Refined crystal structure of the triphosphate conformation of H-ras p21 at 1.35 A resolution: implications for the mechanism of GTP hydrolysis. EMBO J. 9, 2351–2359 (1990).
Potterton, L. et al. Developments in the CCP4 molecular-graphics project. Acta Crystallogr. D Biol. Crystallogr. 60, 2288–2294 (2004).
Halaban, R. et al. PLX4032, a selective BRAF(V600E) kinase inhibitor, activates the ERK pathway and enhances cell migration and proliferation of BRAF(WT) melanoma cells. Pigment Cell Melanoma Res. 23, 190–200 (2010).
Donnelly, M.P. et al. The distribution and most recent common ancestor of the 17q21 inversion in humans. Am. J. Hum. Genet. 86, 161–171 (2010).
Tworkoski, K. et al. Phosphoproteomic screen identifies potential therapeutic targets in melanoma. Mol. Cancer Res. 9, 801–812 (2011).
Kong, Y. Btrim: A fast, lightweight adapter and quality trimming program for next-generation sequencing technologies. Genomics 98, 152–153 (2011).
Li, H. & Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 25, 1754–1760 (2009).
Li, H. et al. The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–2079 (2009).
Garla, V., Kong, Y., Szpakowski, S. & Krauthammer, M. MU2A—reconciling the genome and transcriptome to determine the effects of base substitutions. Bioinformatics 27, 416–418 (2011).
Sathirapongsasuti, J.F. et al. Exome sequencing-based copy-number variation and loss of heterozygosity detection: ExomeCNV. Bioinformatics 27, 2648–2654 (2011).
Thorvaldsdóttir, H., Robinson, J.T. & Mesirov, J.P. Integrative Genomics Viewer (IGV): high-performance genomics data visualization and exploration. Brief. Bioinform published online, doi:10.1093/bib/bbs017 (19 April 2012).
Koboldt, D.C. et al. VarScan 2: somatic mutation and copy number alteration discovery in cancer by exome sequencing. Genome Res. 22, 568–576 (2012).
Zhang, Q. et al. CMDS: a population-based method for identifying recurrent DNA copy number aberrations in cancer from high-resolution data. Bioinformatics 26, 464–469 (2010).
Wang, X., He, L., Wu, Y.I., Hahn, K.M. & Montell, D.J. Light-mediated activation reveals a key role for Rac in collective guidance of cell movement in vivo. Nat. Cell Biol. 12, 591–597 (2010).
Wu, Y.I. et al. A genetically encoded photoactivatable Rac controls the motility of living cells. Nature 461, 104–108 (2009).
Machacek, M. et al. Coordination of Rho GTPase activities during cell protrusion. Nature 461, 99–103 (2009).
Processing of X-ray diffraction data collected in oscillation mode. in Methods in Enzymology, Vol. 276 (eds. Otwinowski, Z. & Minor, W.) Ch. 20, 307–326 (Academic Press, New York, 1997).
McCoy, A.J., Grosse-Kunstleve, R.W., Storoni, L.C. & Read, R.J. Likelihood-enhanced fast translation functions. Acta Crystallogr. D Biol. Crystallogr. 61, 458–464 (2005).
Hirshberg, M., Stockley, R.W., Dodson, G. & Webb, M.R. The crystal structure of human rac1, a member of the rho-family complexed with a GTP analogue. Nat. Struct. Biol. 4, 147–152 (1997).
Perrakis, A., Harkiolaki, M., Wilson, K.S. & Lamzin, V.S. ARP/wARP and molecular replacement. Acta Crystallogr. D Biol. Crystallogr. 57, 1445–1450 (2001).
Murshudov, G.N., Vagin, A.A. & Dodson, E.J. Refinement of macromolecular structures by the maximum-likelihood method. Acta Crystallogr. D Biol. Crystallogr. 53, 240–255 (1997).
Emsley, P. & Cowtan, K. Coot: model-building tools for molecular graphics. Acta Crystallogr. D Biol. Crystallogr. 60, 2126–2132 (2004).
Chen, V.B. et al. MolProbity: all-atom structure validation for macromolecular crystallography. Acta Crystallogr. D Biol. Crystallogr. 66, 12–21 (2010).
Zhang, B., Zhang, Y., Wang, Z. & Zheng, Y. The role of Mg2+ cofactor in the guanine nucleotide exchange and GTP hydrolysis reactions of Rho family GTP-binding proteins. J. Biol. Chem. 275, 25299–25307 (2000).
Nagata, K. et al. The MAP kinase kinase kinase MLK2 co-localizes with activated JNK along microtubules and associates with kinesin superfamily motor KIF3. EMBO J. 17, 149–158 (1998).
Acknowledgements
This work was supported by the Yale SPORE in Skin Cancer funded by the National Cancer Institute grant number 1 P50 CA121974 (principal investigator, R.H.), the Melanoma Research Alliance (a Team award to R.H., M.B., M.K. and D.F.S.), The National Library of Medicine Training grant 5T15LM007056 (P.E.), the Department of Dermatology (R.H.), Yale Comprehensive Cancer Center (M.K.), the National Health and Medical Research Council of Australia (N.K.H. and K.D.-R.), Gilead Sciences, Inc. (J.S., M.K., R.H. and T.J.B.) and a generous gift from Roz and Jerry Meyer (R.H., M.S. and H.M.K.). We thank C. Truini, W. Meng, B. Speed, E. Straka, A. Raefski, M. Scallion and S. Levin for technical support, P. Parsons, C. Schmidt and colleagues at the Queensland Institute of Medical Research for generously providing many of the melanoma cell lines, the Yale Center for Genome Analysis and the Northeastern Collaborative Access Team (NE-CAT) facility at the Advanced Photon Source at Argonne National Laboratory.
Author information
Authors and Affiliations
Contributions
M.K., R.H., R.P.L., J.S. and T.J.B. designed and supervised the study. Y.K., P.E., M.C., J.P.M., S. Ma, G.G. and A.C. performed the bioinformatic analyses. A.B., E.C., E.C.H., M.J.D., K.D.-R., K.K.K., N.K.H. and S. Mane collected and analyzed the melanoma samples and performed the sequencing and functional experiments. B.H.H. and T.J.B. performed the crystallographic studies. S.A., D.N., M.B., M.S., H.M.K., M.A.M. and R.S.L. provided the clinical specimens and the clinical annotation. D.E.B. and D.F.S. analyzed sun-related mutations. All authors contributed to the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
About this article
Cite this article
Krauthammer, M., Kong, Y., Ha, B. et al. Exome sequencing identifies recurrent somatic RAC1 mutations in melanoma. Nat Genet 44, 1006–1014 (2012). https://doi.org/10.1038/ng.2359
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ng.2359
This article is cited by
-
Unique vulnerability of RAC1-mutant melanoma to combined inhibition of CDK9 and immune checkpoints
Oncogene (2024)
-
Cooperative function of oncogenic MAPK signaling and the loss of Pten for melanoma migration through the formation of lamellipodia
Scientific Reports (2024)
-
Deciphering neuroprotective mechanism of nitroxoline in cerebral ischemia: network pharmacology and molecular modeling-based investigations
Molecular Diversity (2024)
-
Alpha-melanocyte stimulating hormone (α-MSH): biology, clinical relevance and implication in melanoma
Journal of Translational Medicine (2023)
-
Sequence dependencies and mutation rates of localized mutational processes in cancer
Genome Medicine (2023)