Abstract
Micropapillary carcinoma has been reported as an aggressive variant of carcinoma in several organs, where it is associated with frequent lymphovascular invasion and poor clinical outcome. This study explored the clinicopathological features of colorectal adenocarcinoma with a micropapillary carcinoma component and compared them with those of conventional colorectal adenocarcinoma. One hundred seventy-eight consecutive cases of surgically resected colorectal carcinomas were studied for tumor size, type, depth of invasion, nodal and distant metastases, tumor stage, and percentage and extent of micropapillary component. Among 178 cases of colorectal carcinoma, 34 (19.1%) cases had a micropapillary component, which ranged from 5 to 60% of the entire tumor. Lymph node metastasis was identified in 25 of 34 (73.5%) carcinomas with micropapillary component, whereas they were detected in 61 of 144 (42.4%) cases without micropapillary component (P=0.001). Lymphovascular invasion was identified more frequently in carcinoma with micropapillary component (41.2%) than carcinoma without micropapillary component (20.1%; P<0.05). Distant metastases occurred in 4 of 34 cases (11.7%) with micropapillary component and in 10 of 144 cases (6.9%) without micropapillary component (P=0.311). Multivariate regression analysis demonstrated that the presence of micropapillary component, as well as tumor stage and lymphovascular invasion are independent predictors of regional nodal metastasis.
Similar content being viewed by others
Main
Colorectal carcinomas are among the most common malignant neoplasms and are the second and third most common cause of cancer death in men and women in the United States, respectively.1 The most important prognostic factors for colorectal cancers are the depth of invasion, lymph node status and distant metastasis. Currently, therapeutic decisions are mainly based on the TNM staging of cancer. No other reliable histomorphologic features are available for prognostication. Despite tremendous advances in our understanding of the molecular mechanisms of colorectal cancer in the last decade, reliable markers that can be used for prognosis and prediction of response to the treatment have not been identified.
Micropapillary carcinoma component has recently been described in several organs such as breast, bladder, lung and salivary glands. It has been reported to have an aggressive behavior with a high propensity for lymphovascular invasion, lymph node metastases and poor clinical outcome.2, 3, 4, 5
Pure micropapillary carcinoma is extremely rare. Micropapillary component is usually associated with conventional carcinoma. Histologically, micropapillary features are characterized by tight neoplastic cell clusters surrounded by cleft-like spaces. The tumor cells have eosinophilic cytoplasm and pleomorphic nuclei. Micropapillary colorectal carcinoma has not been well studied. To the best of our knowledge, there is only one previously published report of invasive micropapillary colorectal carcinoma, which described a series of patients from South Korea.6
Materials and methods
A total of 178 consecutive cases of colorectal carcinoma were retrieved from the archival files of The Methodist Hospital, Houston, Texas. The colorectal resection specimens were processed and examined according to standard procedures. For smaller tumors, the entire tumor was submitted for examination; for larger tumors, multiple sections with deepest invasion were submitted for examination. Proximal and distal margins were submitted for all tumors as well as radial margin when applicable. Regional lymph nodes were entirely submitted for microscopic examination. Information about tumor size, histologic type, depth of invasion, nodal and distant metastases, tumor stage, and percentage of micropapillary component was obtained from review of all slides and pathology reports. The H&E slides were examined separately by three pathologists (SS, BH and JR) using the predetermined criteria. A consensus diagnosis was reached for equivocal cases by reviewing the slides together using a multiheaded microscope.
Categorical variables such as gender, tumor location, tumor grade, nodal status, etc., were summarized by frequencies and percentages. Quantitative variables were summarized by mean, range and standard deviation (s.d.). Fisher's exact or χ2 test was used to compare categorical variables among carcinomas with or without micropapillary component. Independent Student's t-test was used for comparison of age, tumor size, total numbers of lymph nodes and positive lymph nodes. Binary multivariate regression analysis was used to assess the hazard ratio of each variable for prediction of nodal metastasis. Statistical analysis was performed with SPSS for Windows (release 13.0, SPSS Inc., Chicago, IL, USA).
Results
Patient age ranged from 25 to 97 years (mean 68.7). Ninety-four patients were men and 84 were women. The tumors were present in right colon including cecum (n=77), left colon (n=77), and rectum (n=13). The location of 11 tumors was not specified. The resected bowel length ranged from 6 to 129 cm with a mean of 24.9 cm. Tumor size ranged from 0.2 to 12.5 cm (mean 4.3 cm). Mean number of total lymph nodes dissected was 13.9 (range of 0–49) and mean positive lymph nodes was 1.9 (range of 1–24). Of 178 cases, 145 carcinomas were colorectal adenocarcinoma, not otherwise specified, 30 were mucinous adenocarcinoma, and three were signet-ring cell adenocarcinoma.
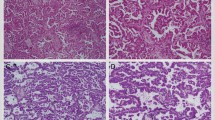
Micropapillary component was identified in 34 of 178 cases (19.1%) of colorectal carcinoma. The micropapillary growth pattern ranged from 5 to 60% of the entire tumor. In fact, less than 10% micropapillary growth pattern was seen in majority (70%) of the colorectal carcinoma with micropapillary component. Micropapillary pattern was characterized by typical tight small cluster of tumor cells with eosinophilic cytoplasm and a clear lacunar space around the tumor nest (Figure 1a). The nuclei were moderately to highly pleomorphic. The cytoplasm was abundant with eosinophilia (Figure 1b). Very often, the micropapillary focus was associated with single cell infiltration. Many tumor nests had a peculiar reverse glandular polarity (Figure 1c). The micropapillary component was often present at the invasive edge of the tumor. Many nodal metastatic foci showed typical micropapillary pattern (Figure 1d). Five carcinomas with micropapillary component were mucinous adenocarcinoma and the remainder was conventional colorectal adenocarcinoma.
Primary and metastatic colorectal adenocarcinoma with micropapillary features. (a) Colon adenocarcinoma diffusely infiltrates tissue as small nests and clusters with typical lacunar spaces (H&E: × 100). (b) Tumor cells with abundant eosinophilic cytoplasm (H&E: × 400). (c) Tumor cell nest with reverse polarity with an outer common border (H&E: × 400). (d) Nodal metastasis with striking micropapillary pattern (H&E: × 100).
The comparison of clinicopathologic features of colorectal carcinoma with and without micropapillary components are summarized in Table 1. The gender distribution and mean age were similar in both groups. Ninety-seven percent and 94% of the tumors were grade 2 or grade 3 in carcinomas with or without micropapillary component, respectively. The tumor locations and depth of invasion, and tumor sizes were also similar in both groups. There was slightly higher percentage of T3/T4 tumors in the micropapillary group than in the non-micropapillary group (76.5 vs 65.2%), but the difference was not statistically significant (P=0.23). While the total number of lymph nodes in both groups was similar (15.7 vs 13.5), the number of positive lymph nodes was significantly higher in carcinomas with micropapillary component than tumors without a micropapillary component (3.7 vs 1.4) (P=0.001). Twenty-five of 34 (73.5%) carcinomas with micropapillary component had nodal metastasis, compared with 42.4% nodal metastases in carcinomas without micropapillary component. Four patients in micropapillary group (11.7%) had distant metastases and 10 (6.9%) had distant metastases in the non-micropapillary component group (P=0.311). In addition, lymphovascular invasion was documented in 41.2% of the micropapillary group, which was significantly higher than that of the non-micropapillary group (20.1%, P=0.014).
To determine whether the extent or percentage of micropapillary component in colorectal carcinoma was associated with nodal metastasis, we analyzed nodal metastasis by carcinomas with less than or equal to 10% micropapillary component and those with more than 10%. As shown in Table 2, nine of nine (100%) carcinomas with more than 10% micropapillary component had nodal metastases and 16 of 25 (64%) of carcinomas with ≤10% micropapillary component had nodal metastases. This difference was not statistically significant (P=0.073).
To investigate further the importance of micropapillary pattern in colorectal adenocarcinoma and its association with nodal metastasis, multivariate regression analyses were performed with inclusion of patents' age, gender, tumor location, tumor grade, depth of invasion and lymphovascular invasion (Table 3). As expected, the depth of invasion (T stage) and status of lymphovascular invasion were highly associated with nodal metastasis. In addition, the presence of micropapillary component was also significantly associated with nodal metastasis with odds ratio even higher than that of the depth of invasion. Patient age, gender, tumor location and tumor grade were not significantly associated with lymph node metastasis.
Discussion
Several histological types of colorectal carcinomas and their clinical behavior have been well described, including mucinous adenocarcinoma, signet ring adenocarcinoma, basaloid carcinoma, clear cell carcinoma, medullary adenocarcinoma and anaplastic carcinoma.7, 8, 9, 10, 11, 12, 13, 14, 15 Some of these histological types are associated with a worse prognosis than that of conventional adenocarcinoma.16, 17, 18, 19 To the best of our knowledge, there has only been one previously published report of micropapillary colorectal carcinoma by Kim et al6 with a series from South Korea. Although no follow-up regarding patient's survival was provided, Kim et al6 consider this neoplasm as an aggressive variant of adenocarcinoma due to its presentation with high tumor stage, as well as more frequent nodal and distant metastasis. Our results are similar, but we have additionally shown that the presence of micropapillary component is an independent predictor of nodal metastasis.
As compared with conventional colorectal adenocarcinomas, our data demonstrate that colorectal carcinomas with micropapillary component have a significantly higher rate of lymph node metastasis and lymphovascular invasion. It is believed that the characteristic morphology of micropapillary carcinoma, including reverse polarity of neoplastic cells with apical surface facing stroma and expression of MUC1 in basal aspects is responsible for stromal and lymphovascular invasion; therefore, the dissemination of tumor cells.20, 21, 22 This is also supported by the finding that all of the micropapillary component of our study were present at the invasive edge of the tumor and most metastatic foci had a micropapillary features.
Our study demonstrates that invasive micropapillary component is not an uncommon finding in colorectal carcinoma with incidence of 19.1% in our series. It is much higher than the incidence reported by Kim et al,6 who identified a micropapillary component in 9.4% of 585 colorectal carcinoma cases. This difference may due to different study patient populations, different distribution of tumor stage or different criteria used for identification of micropapillary component. Although no statistical difference was observed, there was a trend that indicates that the proportion of micropapillary component may be an important factor as all nine cases (100%) with more than 10% micropapillary component had nodal metastasis, whereas 16 of 25 (64%) cases with equal or less than 10% micropapillary component had nodal metastasis. Larger sample size of carcinomas with micropapillary component will be necessary to verify the importance of proportion of micropapillary component.
Micropapillary component in colorectal carcinoma is usually a minor component of the entire tumor and is often present at the edge of invasive tumor. Sections of tumor at the interface with adjacent tissue and tumor at the deepest invasion may be helpful in identifying the micropapillary component. In our study, we did not find evidence of positive correlation of micropapillary component with high tumor stage. This result is different from that of Kim et al.6 In fact, of the 34 cases of colorectal carcinoma with micropapillary component, two of three T1 tumors (submucosal invasion) had nodal metastasis. Therefore, identification of micropapillary component in a tumor, particularly in biopsies, should alert the pathologist and treating physician that there is a high probability of nodal metastasis when considering extent of surgical resection.
Similar to the results of Kim et al,6 we have also shown that the presence of micropapillary component is associated with lymphovascular invasion. Furthermore, we have shown that both micropapillary component and lymphovascular invasion are strong predictors of lymph node metastasis. In tumors with micropapillary component, typical lacunar space around micropapillary component often simulate lymphovascular invasion. The tumor within the endothelial spaces, as well as in nodal metastasis often retains the micropapillary configuration. It is important not to overdiagnose tumor cells within the lacunar spaces as lymphovascular invasion and immunostaining with endothelial markers may be helpful in equivocal situations.
In the study of 55 micropapillary colorectal carcinomas, Kim et al6 found no significant difference in immunohistochemical profiles or microsatellite instability between colorectal carcinomas with micropapillary component and those without micropapillary component. We did not perform immunohistochemical studies on our cases. Our data show that colorectal adenocarcinoma with micropapillary component occurred in all sites of large bowel, not like colorectal carcinomas with microsatellite instability which often occur in the right colon and which may be medullary, undifferenciated, signet ring or mucinous.23, 24, 25, 26 The majority (18/34) of colorectal carcinomas with a micropapillary component were located in the sigmoid colon and rectum, 11 (11 of 34) cases were from right colon and cecum. Five cases were mucinous adenocarcinoma and the remainder was conventional adenocarcinoma.
A multivariate regression analysis of combined clinical and pathological factors (Table 3) demonstrated that age, gender, tumor location and tumor grade are not significant for predicting nodal metastasis. However, the presence of a micropapillary component is an independent predictor of nodal metastasis, in addition to depth of invasion and lymphovascular invasion. One of the limitations of our study is that there is no long-term follow-up of patient survival. Nevertheless, it is well documented in the literature that similar to carcinomas arising in other organs, nodal metastasis in colorectal carcinoma is one of the most important prognostic factors of patient survival.27 Once the tumor spreads to the lymph nodes, the 5-year survival rate drops dramatically. It remains to be determined whether the presence of a micropapillary component will be an independent prognostic factor in a larger cohort of patients with long term follow-up.
In summary, micropapillary component is not an infrequent finding in colorectal carcinoma. The presence of a micropapillary component is significantly associated with lymphovascular invasion and nodal metastasis. Its presence is an independent predictor of lymph node metastasis, and could be a significant histologic prognostic factor of survival. Future studies need to be directed to elucidate the molecular mechanisms of carcinogenesis and tumor progression of this unique morphologic pattern.
References
Jemal A, Siegel R, Ward E, et al. Cancer statistics, 2006. CA Cancer J Clin 2006;56:106–130.
Amin MB, Ro JY, el-Sharkawy T, et al. Micropapillary variant of transitional cell carcinoma of the urinary bladder. Histologic pattern resembling ovarian papillary serous carcinoma. Am J Surg Pathol 1994;18:1224–1232.
Amin MB, Tamboli P, Merchant SH, et al. Micropapillary component in lung adenocarcinoma: a distinctive histologic feature with possible prognostic significance. Am J Surg Pathol 2002;26:358–364.
Nagao T, Gaffey TA, Visscher DW, et al. Invasive micropapillary salivary duct carcinoma: a distinct histologic variant with biologic significance. Am J Surg Pathol 2004;28:319–326.
Siriaunkgul S, Tavassoli FA . Invasive micropapillary carcinoma of the breast. Mod Pathol 1993;6:660–662.
Kim MJ, Hong SM, Jang SJ, et al. Invasive colorectal micropapillary carcinoma: an aggressive variant of adenocarcinoma. Hum Pathol 2006;37:809–815.
Giacchero A, Aste H, Baracchini P, et al. Primary signet-ring carcinoma of the large bowel. Report of nine cases. Cancer 1985;56:2723–2736.
Hall-Craggs M, Toker C . Basaloid tumor of the sigmoid colon. Hum Pathol 1982;13:497–500.
Jessurun J, Romero-Guadarrama M, Manivel JC . Medullary adenocarcinoma of the colon: clinicopathologic study of 11 cases. Hum Pathol 1999;30:843–848.
Jewell LD, Barr JR, McCaughey WT, et al. Clear-cell epithelial neoplasms of the large intestine. Arch Pathol Lab Med 1988;112:197–199.
Lanza G, Gafa R, Matteuzzi M, et al. Medullary-type poorly differentiated adenocarcinoma of the large bowel: a distinct clinicopathologic entity characterized by microsatellite instability and improved survival. J Clin Oncol 1999;17:2429–2438.
Laufman H, Saphir O . Primary linitis plastica type of carcinoma of the colon. AMA Arch Surg 1951;62:79–91.
Newell KJ, Penswick JL, Driman DK . Basaloid carcinoma of the colon arising at the splenic flexure. Histopathology 2001;38:232–236.
Sasaki O, Atkin WS, Jass JR . Mucinous carcinoma of the rectum. Histopathology 1987;11:259–272.
Younes M, Katikaneni PR, Lechago J . The value of the preoperative mucosal biopsy in the diagnosis of colorectal mucinous adenocarcinoma. Cancer 1993;72:3588–3592.
Connelly JH, Robey-Cafferty SS, Cleary KR . Mucinous carcinomas of the colon and rectum. An analysis of 62 stage B and C lesions. Arch Pathol Lab Med 1991;115:1022–1025.
Green JB, Timmcke AE, Mitchell WT, et al. Mucinous carcinoma—just another colon cancer? Dis Colon Rectum 1993;36:49–54.
Nakahara H, Ishikawa T, Itabashi M, et al. Diffusely infiltrating primary colorectal carcinoma of linitis plastica and lymphangiosis types. Cancer 1992;69:901–906.
Sadahiro S, Ohmura T, Saito T, et al. An assessment of the mucous component in carcinoma of the colon and rectum. Cancer 1989;64:1113–1116.
Luna-More S, Gonzalez B, Acedo C, et al. Invasive micropapillary carcinoma of the breast. A new special type of invasive mammary carcinoma. Pathol Res Pract 1994;190:668–674.
Nassar H, Pansare V, Zhang H, et al. Pathogenesis of invasive micropapillary carcinoma: role of MUC1 glycoprotein. Mod Pathol 2004;17:1045–1050.
Pettinato G, Manivel CJ, Panico L, et al. Invasive micropapillary carcinoma of the breast: clinicopathologic study of 62 cases of a poorly recognized variant with highly aggressive behavior. Am J Clin Pathol 2004;121:857–866.
Copeland EM, Miller LD, Jones RS . Prognostic factors in carcinoma of the colon and rectum. Am J Surg 1968;116:875–881.
Ligtenberg MJ, Buijs F, Vos HL, et al. Suppression of cellular aggregation by high levels of episialin. Cancer Res 1992;52:2318–2324.
van de Wiel-van Kemenade E, Ligtenberg MJ, de Boer AJ, et al. Episialin (MUC1) inhibits cytotoxic lymphocyte-target cell interaction. J Immunol 1993;151:767–776.
Wesseling J, van der Valk SW, Hilkens J . A mechanism for inhibition of E-cadherin-mediated cell-cell adhesion by the membrane-associated mucin episialin/MUC1. Mol Biol Cell 1996;7:565–577.
Compton CC, Fielding LP, Burgart LJ, et al. Prognostic factors in colorectal cancer. College of American Pathologists Consensus Statement 1999. Arch Pathol Lab Med 2000;124:979–994.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Haupt, B., Ro, J., Schwartz, M. et al. Colorectal adenocarcinoma with micropapillary pattern and its association with lymph node metastasis. Mod Pathol 20, 729–733 (2007). https://doi.org/10.1038/modpathol.3800790
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/modpathol.3800790
Keywords
This article is cited by
-
Loss of CDX2 in colorectal cancer is associated with histopathologic subtypes and microsatellite instability but is prognostically inferior to hematoxylin–eosin-based morphologic parameters from the WHO classification
British Journal of Cancer (2021)
-
Metastatic colorectal micropapillary carcinoma presenting as lymphangitic lung carcinomatosis
Clinical Journal of Gastroenterology (2021)
-
The Increasing Relevance of Tumour Histology in Determining Oncological Outcomes in Colorectal Cancer
Current Colorectal Cancer Reports (2015)
-
Micropapillary component in gastric adenocarcinoma: an aggressive variant associated with poor prognosis
Gastric Cancer (2015)
-
Colorectal micropapillary carcinomas are associated with poor prognosis and enriched in markers of stem cells
Modern Pathology (2013)