Abstract
Our study aimed to validate the clinicopathological characteristics and prognosis of lung adenocarcinoma (ADC) with a filigree pattern and to further investigate the relationship between the filigree pattern and the classical micropapillary (MP) pattern. We retrospectively reviewed the clinical and pathologic characteristics of 461 Chinese patients with completely resected ADC (stage I, 310; stage II, 44; stage III, 107). The filigree pattern was more likely to be observed in ADC with a higher stage (p = 0.003) and the classical MP pattern (p < 0.001). Patients with filigree-predominant ADC showed poor survival, similar to those with classical MP-predominant ADC. Multivariate analysis confirmed that the presence of the filigree pattern was an independent prognostic factor for recurrence-free survival (hazard ratio (HR), 2.01; 95% confidence interval (CI), 1.50–2.68; p < 0.001) and overall survival (OS; HR, 1.83; 95% CI, 1.34–2.50; p < 0.001). Patients with both classical MP-positive and filigree-positive ADC had the worst survival compared with those with the filigree pattern or classical MP pattern alone. In stage I, ADC with both the filigree and classical MP patterns had a higher incidence of micrometastasis than ADC with the filigree pattern or classical MP pattern alone. Lymph node micrometastasis indicated poor survival in patients with ADC with the filigree pattern or classical MP pattern. Similar clinicopathologic features between patients with the filigree pattern and the classical MP pattern support the inclusion of the filigree pattern in the MP category. Recognition of the filigree pattern could provide helpful prognostic information, especially for stage I ADC.
Similar content being viewed by others
Introduction
The new classification of lung adenocarcinoma (ADC) proposed by the International Association for the Study of Lung Cancer, American Thoracic Society, and European Respiratory Society in 2011 has been widely adopted in clinical practice and research investigations [1,2,3,4]. The inclusion of the micropapillary (MP) pattern as the fifth common morphological subtype of ADC was one of the most important advances. Numerous studies have demonstrated that the MP pattern is associated with worse survival outcomes, a higher risk of disease recurrence after limited resection, survival benefits from adjuvant chemotherapy [5, 6]. More importantly, this clinical significance even extends to ADC with a small proportion of an MP component [7].
Recently, Emoto et al. [8] from Memorial Sloan Kettering Cancer Center introduced a novel morphological pattern named as the filigree pattern. Their first data indicated that the filigree pattern is frequently associated with the classical MP pattern. Furthermore, similar clinical features and survival outcomes were observed between these two morphological patterns. Thus, expanding the concept of the MP subtype to include the filigree pattern has been suggested.
However, these results were mainly based on an American population. Thus, we retrospectively reviewed pathology slides of 461 surgically resected cases of ADC in China. This present study aimed to investigate the clinicopathological characteristics and prognostic significance of the filigree pattern and to validate the relationship between the filigree pattern and classical MP pattern.
Materials and methods
Patient selection
The Institutional Review Board of Shanghai Pulmonary Hospital approved this study (K20-412). A total of 1123 patients with lung cancer underwent surgical resection at Shanghai Pulmonary Hospital from January 1, 2009 to December 31, 2009. The inclusion criteria for our study included the following: (1) pathologically diagnosis of primary ADC and (2) the presence of a solitary tumor. Patients were excluded if one of the following criteria was fulfilled: (1) the presence of multiple primary ADC lesions; (2) pathological diagnosis of ADC in situ, minimally invasive ADC, or variants of invasive ADC (mucinous, colloid, etc.); (3) receipt of neoadjuvant therapy; (4) receipt of R1 or R2 resection; and (5) lack of sufficient tumor slides for review. Tumor staging was assigned according to the 8th edition of the tumor, node, metastasis (TNM) classification [9]. Clinical data were retrospectively extracted from electronic medical records. Tumor recurrence was diagnosed based on clinical, radiological, or pathological data. Survival outcomes were collected from outpatient clinic visit records and telephone follow-up data. These patients were followed up until the end of 2016.
Histopathologic evaluation
Hematoxylin–eosin-stained tumor slides were microscopically evaluated independently by two pathologists (HX and SZ) who were blinded to the clinical information and survival outcomes. If any disagreement occurred, discussion was necessary before a consensus was reached.
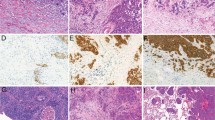
The MP pattern in the present study included the filigree pattern and classical pattern. The definition of the filigree pattern was in accordance with that reported by Emoto: (1) the tumor cells grow in delicate, lace-like, narrow stacks; (2) the stacks of tumor cells lack fibrovascular cores; and (3) the stacks of tumor cells consist of at least three tumor cells but up to three cells in width (Fig. 1A, B) [8]. The classical pattern was defined in the 2015 WHO classification system as tumors cells growing in papillary tufts forming florets with fibrovascular cores (Fig. 1C, D) [2]. The stromal pattern, which was defined as MP tufts located in spaces encased by connective tissues, was also identified and classified into the classical pattern [1, 2].
Examples of the filigree pattern. Lace-like narrow stacks of tumor cells without fibrovascular cores with at least 3 tumor cell nuclei piled up from the basal tumor cell layer (A ×100; B ×200). Examples of the classical micropapillary patterns. Tumor cells growing in papillary tufts forming florets with no fibrovascular cores (C ×100; D ×200).
Each tumor was reviewed according to the 2015 WHO classification system, and the percent of each histological component (lepidic, acinar, papillary, MP, and solid) was recorded in 5% increments. The pattern with the largest percent (even if <50%) was regarded as the predominant pattern, and the rest of the patterns that occupied at least 5% were considered minor components. Visceral pleural invasion, tumor spread through air spaces (STAS), and invasive tumor size were assessed according to the diagnostic methodology described in previous studies [10,11,12].
All resected lymph nodes of the patients with stage I ADC were evaluated for micrometastasis, which is defined as isolated tumors cells or cellular clusters ≤ 0.2 mm in the greatest dimension in nodes. The steps and methods for detection of lymph node micrometastasis were introduced in our previous study in detail [13]. Briefly, the presence of both cytokeratin AE1/AE3-positive and thyroid transcription factor-1-positive cells in serial lymph node tissue sections by immunohistochemical staining provided evidence of micrometastasis (Supplementary Fig. 1).
Statistical analysis
All clinicopathologic parameters are shown as the mean ± standard deviation, median (range), and number (percentage). Categorical data were compared by Pearson’s χ2 test, and numerical data were compared by Student’s t test between two groups. Recurrence-free survival (RFS) and overall survival (OS) were the outcomes of interest for prognosis. RFS was defined as the time from the date of operation to that of disease recurrence, and OS was defined as the time from the date of operation to that of death or last follow-up. The Kaplan–Meier method was used to estimate RFS and OS, and the difference between groups was assessed by the log-rank test. A Cox proportional hazards regression model was performed to identify the independent risk factors for RFS and OS. A logistic regression model was applied to evaluate the independent risk factors for lymph node micrometastasis. The input variables in the multivariate model were those with p values < 0.1 in the univariate analysis. A two-sided p value of <0.05 indicated statistical significance. All statistical analyses were conducted using SPSS 22.0 (IBM Corporation, Armonk, NY), and survival curves were plotted with GraphPad Prism 7.0 (GraphPad Software, San Diego, CA).
Results
Association between the filigree pattern and clinicopathologic features
A total of 461 patients with ADC met the inclusion criteria. The clinicopathologic characteristics of these patients are listed in Table 1. Of these patients, 229 (50%) were women, and 350 (76%) had no smoking history. Regarding the surgical type, a small number of patients underwent limited resection (6%). In addition, most patients with ADC were classified into stage I (67%), and acinar predominant ADC was the most common type (47%).
The filigree pattern was identified in 148 patients (32%). Table 1 showed that the filigree pattern was more likely to be observed in ADC with larger invasive tumors (p = 0.006), lymph node metastasis (p < 0.001), STAS (p < 0.001), and higher pathologic TNM stage (p = 0.003). Regarding the relationship with other morphologic patterns, the filigree pattern was less frequently associated with the lepidic pattern (p < 0.001) and more frequently associated with the classical MP pattern (p < 0.001).
Filigree pattern and survival outcomes
When all included patients were subclassified according to the predominant histological type, Fig. 2A, B shows that patients with lepidic-predominant ADC had the most favorable RFS and OS, while those with MP-predominant and solid-predominant ADC had the worst long-term survival (RFS: p < 0.001; OS: p < 0.001). Thirty-six patients with MP-predominant ADC could be further divided into 18 patients with classical MP-predominant ADC and 18 patients with filigree MP-predominant ADC. Log-rank tests showed comparable RFS and OS between the two groups (Fig. 2C, D) (RFS: p = 0.449; OS: p = 0.288).
Survival curves of the predominant histological subtypes after reclassification to include the filigree pattern (A, B). Survival comparison between filigree-predominant adenocarcinoma and classical MP-predominant adenocarcinoma (C, D). Survival in patients with lung adenocarcinoma stratified by the filigree pattern (E, F). Filigree (+), filigree pattern presence; Filigree (−), filigree pattern absence.
When the patients were separated by the presence of the filigree pattern (≥5%), patients without the filigree pattern had a better RFS (p < 0.001) and OS (p < 0.001) than those with the filigree pattern (Fig. 2E, F). Multivariate analyses confirmed that the presence of the filigree pattern was an independent risk factor for RFS (hazard ratio (HR) = 2.01, 95% confidence interval (CI): 1.25–2.38, p < 0.001) and OS (HR = 1.83, 95% CI: 1.34–2.50, p < 0.001). Furthermore, the presence of the classical MP pattern also had the ability to predict survival outcomes (RFS: HR = 1.72, 95% CI: 1.25–2.38, p = 0.001; OS: HR = 1.67, 95% CI: 1.18–2.36, p = 0.003) (Table 2).
Clinical and prognostic significance of the filigree pattern and classical pattern
When the MP pattern was stratified by the filigree pattern and classical MP pattern, our study included 202 patients without the MP pattern (44%), 58 patients with the filigree pattern alone (13%), 111 patients with the classical MP pattern alone (24%), and 90 patients with both the filigree and classical MP patterns (19%). Supplementary Table 1 summarizes the clinicopathologic characteristics of the four groups. Compared with the MP-negative group, the remaining three groups were closely associated with aggressive features, including invasive tumor size (p < 0.001), lymph node metastasis (p < 0.001), STAS (p < 0.001), and pathologic TNM stage (p < 0.001).
Survival analysis revealed the worst RFS and OS for patients with both the filigree and classical MP patterns, followed by patients with the filigree pattern alone and the classical MP pattern alone, and the best survival occurred in patients without the MP pattern (RFS: p < 0.001; OS: p < 0.001) (Fig. 3A, B). The worst prognosis of patients with both the filigree and classical MP patterns might be driven by MP-predominant ADC because the majority of these ADCs (23/36, 64%) were in this group. Similar survival results were observed after the exclusion of cases with MP-predominant ADC (Fig. 3C, D). The fact that cases with both filigree and classic MP patterns had a worse prognosis than cases with either pattern alone is probably related to the overall proportion of MP. Thus, we compared the overall proportion of MP component (overall MP proportion = percentage of classical MP component + percentage of filigree component) in the tumor. The overall MP proportion of ADCs with filigree pattern alone, classical MP pattern alone, and both filigree and classical MP patterns were demonstrated by boxplot (Fig. 3E, F). The overall MP proportion of ADCs with both filigree pattern and classical MP pattern was higher than that of ADCs with filigree pattern alone (p < 0.001), classical MP pattern alone (p < 0.001).
Survival in patients with lung adenocarcinoma (A, B) and non-micropapillary predominant adenocarcinoma (C, D) stratified by the filigree pattern and classical micropapillary pattern. Comparison of overall micropapillary proportion (percentage of filigree pattern plus percentage of classical micropapillary pattern) among lung adenocarcinomas with filigree pattern alone, classical micropapillary pattern alone, and both filigree pattern and classical micropapillary pattern (E, F). Micropapillary (−), filigree and classical micropapillary pattern absence; Filigree (+), filigree pattern presence; Filigree (−), filigree pattern absence; Classical (+), classical micropapillary pattern presence; Classical (−), classical micropapillary pattern absence.
Multivariate analysis revealed that the presence of any MP subtype was an independent prognostic factor, including the filigree pattern alone (RFS: HR = 1.90, 95% CI: 1.15–3.12, p = 0.012; OS: HR = 1.80, 95% CI: 1.04–3.12, p = 0.036), classical pattern alone (RFS: HR = 1.66, 95% CI: 1.09–2.52, p = 0.018; OS: HR = 1.65, 95% CI: 1.05–2.61, p = 0.031), and both the filigree and classic patterns (RFS: HR = 3.43, 95% CI: 2.28–5.17, p < 0.001; OS: HR = 3.04, 95% CI: 1.94–4.79, p < 0.001) (Table 2). The results also indicated that the highest risk was seen in patients with both the filigree and classic patterns.
Association between lymph node micrometastasis and the filigree pattern in stage I ADC
Overall, 235 patients with stage I ADC who underwent lymph node sampling and dissection were included in this part. Of those, 35 patients (14.9%) were diagnosed with lymph node micrometastasis, and its correlation with other clinicopathologic characteristics is listed in Supplementary Table 2. Our results showed that lymph node micrometastasis was associated with a high CEA level (p < 0.001), a large invasive tumor size (p = 0.04), a large number of resected lymph nodes (p = 0.023), and the presence of STAS (p = 0.015).
The lepidic pattern was associated with a lower probability of lymph node micrometastasis (p = 0.002). By contrast, the MP pattern (vs. absence: 26.6 vs. 5%; p < 0.001), filigree pattern (vs. absence: 26.8 vs. 10%; p = 0.001), and classical MP pattern (vs. absence: 37.1 vs. 7%; p < 0.001) were all associated with lymph node micrometastasis (Fig. 4A–C). In addition, when patients were divided by the subtypes of the MP pattern, the highest incidence of micrometastasis was 46.4% in patients with both the classical MP and filigree patterns (p < 0.001) (Fig. 4D).
Incidence of lymph node micrometastasis in stage I lung adenocarcinoma stratified by the classical micropapillary pattern and filigree pattern (A–D). Survival in lung adenocarcinoma stratified by micrometastasis, the filigree pattern, and the classical micropapillary pattern (E–H). Micropapillary (+), filigree and classical micropapillary pattern presence; Micropapillary (−), filigree and classical micropapillary pattern absence; Micrometastasis (+), lymph node micrometastasis presence; Micrometastasis (−), lymph node micrometastasis absence; Filigree (+), filigree pattern presence; Filigree (−), filigree pattern absence; Classical (+), classical micropapillary pattern presence; Classical (−), classical micropapillary pattern absence.
Multivariate logistic regression analysis showed that the filigree pattern was an independent risk factor for an increased frequency of lymph node micrometastasis (odds ratio (OR) = 2.65, 95% CI: 1.10–6.43, p = 0.031) as well as the classical MP pattern (OR = 6.93, 95% CI: 2.78–17.27, p < 0.001) (Supplementary Table 3). In addition, the second logistic model revealed that the presence of both the classical MP pattern and the filigree pattern was an independent predictor of lymph node micrometastasis with the highest OR (OR = 18.18, 95% CI: 5.00–68.32, p < 0.001) compared with that of the classical MP pattern only (OR = 8.33, 95% CI: 2.45–28.33, p = 0.001) and filigree pattern alone (OR = 3.28, 95% CI: 0.92–11.73, p < 0.001) (Supplementary Table 3).
Prognostic significance of lymph node micrometastasis and its association with the filigree pattern
Kaplan–Meier analysis showed that lymph node micrometastasis was associated with worse RFS (p < 0.001) and OS (p < 0.001) (Supplementary Fig. 2). When patients were categorized by the filigree pattern and micrometastasis, survival analysis revealed the worst RFS and OS for patients with filigree-positive/micrometastasis-positive ADC, followed by patients with filigree-positive/micrometastasis-negative ADC; the best survival occurred in patients without the filigree pattern (RFS: p < 0.001; OS: p < 0.001) (Fig. 4E, F). Multivariate Cox regression analysis further indicated that filigree-positive/micrometastasis-positive ADC was an independent prognostic factor for worse RFS (HR = 2.66; 95% CI, 1.35–5.21; p = 0.005) in patients with stage I ADC (Supplementary Table 4).
When considering presence of the classical MP pattern, survival analysis revealed the worst RFS and OS for patients with filigree-positive/classical MP-positive/micrometastasis-positive ADC, followed by patients with filigree-positive/classical MP-positive/micrometastasis-negative ADC and patients with filigree-positive or classical MP-positive ADC; the best survival occurred in patients without the MP pattern (RFS: p < 0.001; OS: p < 0.001) (Fig. 4G, H). Multivariate Cox regression analysis further indicated that filigree-positive/classical-positive/micrometastasis-positive ADC was associated with the worst RFS (HR = 5.65; 95% CI, 2.49–12.83; p < 0.001) and OS (HR = 5.34; 95% CI, 2.00–14.25; p = 0.001) in patients with stage I ADC (Supplementary Table 4).
Discussion
Our study investigated the relationship between the newly defined filigree pattern and the classical MP pattern in a Chinese cohort. We found that the presence of the filigree pattern was highly associated with the classical MP pattern. Filigree-predominant ADC was associated with a poor prognosis, similar to classical MP-predominant ADC. The presence of a small amount of the filigree pattern was a prognostic factor for poor survival, which was also similar to the classical MP pattern. In stage I ADC, the filigree pattern was associated with the presence of lymph node micrometastasis. When categorizing the filigree pattern into the MP pattern, the presence of the MP pattern indicated higher tumor invasiveness and a greater incidence of lymph node micrometastasis than the presence of the classical MP pattern alone. Our study supported that the newly described filigree pattern is an expansion of the MP ADC concept rather than a proposed new subtype. This could provide more precise prognostic information in clinical practice.
Emoto et al. [8] introduced the histologic features of the filigree pattern in detail: (1) the tumor cells grow in delicate, lace-like, narrow stacks; (2) the stacks of tumor cells lack fibrovascular cores; and (3) the stacks of tumor cells consist of at least three tumor cells but up to three cells in width. The lepidic, acinar, and papillary patterns were found to be accompanied by the filigree pattern. The filigree pattern was associated with a larger total tumor size, a larger invasive tumor size, a higher pathologic stage, the presence of pleural invasion, the presence of lymphovascular invasion, the presence of necrosis, and the presence of STAS. Filigree-predominant ADC showed a poor prognosis. In addition, a small amount of the filigree pattern was significantly associated with worse cumulative incidence of recurrence in the multivariate analysis. However, these results were mainly based on an American population. Thus, we retrospectively reviewed pathology slides from 461 cases of surgically resected ADC in China. According to the same diagnostic criteria, the filigree pattern was found in 148 cases (32%). The filigree pattern was associated with a larger invasive tumor size, more lymph node metastasis, STAS, and a more advanced TNM stage. The filigree pattern as a predominant pattern or a minor component predicted worse survival. The highly consistent results of these two studies indicate that the filigree pattern is a predictor of the aggressive nature of ADC tumors.
The frequent association of the classical MP pattern with a poor prognosis supports the inclusion of the filigree pattern in the MP subtype. In 148 lung ADCs with the filigree pattern, 90 (61%) cases also had the classical MP pattern. The presence of the filigree pattern as a predominant pattern or minor component was associated with poor prognosis for patients with ADC, similar to the presence of the classical MP pattern. Furthermore, our results showed that recognition of the filigree pattern could provide additional prognostic information in lung ADC with the classical MP pattern. Patients with ADC with both the filigree pattern and classical pattern had a worse prognosis than those with the classical pattern alone. Similarly, Emoto et al. [14] also reported that patients with filigree-positive/classical MP-positive lung ADC had worse survival than those with the filigree pattern alone or classical MP pattern alone at the 19th World Conference on Lung Cancer (5-year OS: ADC without the MP pattern, 89%; ADC with the classical MP pattern alone: 80%; ADC with the filigree pattern alone, 76%; ADC with the filigree and classical MP patterns, 70%). The prognostic value of the MP pattern may be underestimated in clinical practice because of an unrecognized filigree pattern. For example, the “low papillary structure” reported by Fukutomi et al. [15] is the filigree pattern in a lepidic area according to the criteria, which is associated with poor survival in patients with lung ADC. Thus, it is necessary to include the filigree pattern in the MP pattern [16]. This observation could also explain the doubt about the results of the study “Filigree and Classical Micropapillary Pattern Are Orientation-Dependent Views of the Same Lesion” by Drs. Thunnissen and Flieder [17]. If the filigree pattern is a masquerading pseudopattern, the prognostic impact of the MP pattern will not increase when categorizing the filigree pattern into the MP pattern.
According to our previous study, lymph node micrometastasis was associated with the MP pattern and poor prognosis [13]. To further validate the association between the filigree pattern and classical MP pattern, we investigated the correlation of lymph node micrometastasis with the filigree pattern. A total of 235 patients with stage I ADC were included to detect lymph node micrometastasis. Lymph node micrometastasis was a predictor of poor prognosis. Approximately 54% of ADCs with micrometastasis had a filigree pattern. Patients with ADC with the filigree pattern, classical MP pattern, and micrometastasis had the worst survival among all patients. When categorizing the filigree pattern into the MP pattern, the incidence of lymph node micrometastasis in ADC with the MP pattern was higher than that in ADC with the classical MP pattern. This could be another result supporting the expansion of the MP concept. For stage I ADC, lymph node micrometastasis is a vital prognostic factor. Careful search for lymph node micrometastasis should be recommended to provide more accurate pathologic information for stage I ADC with the MP pattern.
As a retrospective study, we need to acknowledge some limitations of this study. First, performance bias and selection bias were inevitable. Second, the sample size might not have been large enough, which is a possible reason for the insignificant OS difference between filigree-positive/classical MP-positive/micrometastasis-positive ADC and filigree-positive/classical MP-positive/micrometastasis-negative ADC. In addition, detection of lymph node micrometastasis was only performed in 235 patients with stage I ADC because of insufficient time and cost. Thus, the small sample size might have influenced the results of the multivariate Cox regression model. Third, because of the surgical strategy in our hospital, most patients with lung ADC underwent lobectomy. The prognostic significance of the filigree pattern in patients with lung ADC who underwent limited resection is unknown. As a final comment, we did not have the mutation data for these patients. The prognostic impact of common driver mutations could not be analyzed. However, patients with early-stage ADC rarely receive postoperative targeted therapy. Thus, this limitation might have little influence on our results.
In conclusion, the criteria for MP ADC should be expanded to include the filigree pattern as well as the classical MP pattern because these patterns are frequently associated with each other and with similar clinical features and prognosis. For ADC with the new MP pattern, careful search for lymph node micrometastasis is recommended to provide more accurate information on stage I ADC.
References
Travis WD, Brambilla E, Noguchi M, Nicholson AG, Geisinger KR, Yatabe Y, et al. International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society International Multidisciplinary classification of lung adenocarcinoma. J Thorac Oncol. 2011;6:244–85.
Travis WD, Brambilla E, Nicholson AG, Yatabe Y, Austin JHM, Beasley MB, et al. The 2015 World Health Organization classification of lung tumors. J Thorac Oncol. 2015;10:1243–60.
Hung JJ, Yeh YC, Jeng WJ, Wu KJ, Huang BS, Wu YC, et al. Predictive value of the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification of lung adenocarcinoma in tumor recurrence and patient survival. J Clin Oncol. 2014;32:2357–64.
Warth A, Muley T, Meister M, Stenzinger A, Thomas M, Schirmacher P, et al. The novel histologic International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society classification system of lung adenocarcinoma is a stage-independent predictor of survival. J Clin Oncol. 2012;30:1438–46.
Nitadori J, Bograd AJ, Kadota K, Sima CS, Rizk NP, Morales EA, et al. Impact of micropapillary histologic subtype in selecting limited resection vs lobectomy for lung adenocarcinoma of 2cm or smaller. J Natl Cancer Inst. 2013;105:1212–20.
Tsao MS, Marguet S, Le Teuff G, Lantuejoul S, Shepherd FA, Seymour L, et al. Subtype classification of lung adenocarcinoma predicts benefit from adjuvant chemotherapy in patients undergoing complete resection. J Clin Oncol. 2015;33:3439–46.
Lee G, Lee HY, Jeong JY, Han J, Cha MJ, Lee KS, et al. Clinical impact of minimal micropapillary pattern in invasive lung adenocarcinoma: prognostic significance and survival outcomes. Am J Surg Pathol. 2015;39:660–6.
Emoto K, Eguchi T, Tan KS, Takahashi Y, Aly RG, Rekhtman N, et al. Expansion of the concept of micropapillary adenocarcinoma to include a newly recognized filigree pattern as well as the classical pattern based on 1468 Stage I lung adenocarcinomas. J Thorac Oncol. 2019;14:1948–61.
Detterbeck FC, Boffa DJ, Kim AW, Tanoue LT. The eighth edition lung cancer stage classification. Chest. 2017;151:193–203.
Kawase A, Yoshida J, Miyaoka E, Asamura H, Fujii Y, Nakanishi Y, et al. Visceral pleural invasion classification in non-small-cell lung cancer in the 7th edition of the tumor, node, metastasis classification for lung cancer: validation analysis based on a large-scale nationwide database. J Thorac Oncol. 2013;8:606–11.
Dai C, Xie H, Su H, She Y, Zhu E, Fan Z, et al. Tumor spread through air spaces affects the recurrence and overall survival in patients with lung adenocarcinoma >2 to 3 cm. J Thorac Oncol. 2017;12:1052–60.
Travis WD, Asamura H, Bankier AA, Beasley MB, Detterbeck F, Flieder DB, et al. The IASLC lung cancer staging project: proposals for coding T categories for subsolid nodules and assessment of tumor size in part-solid tumors in the forthcoming eighth edition of the TNM classification of lung cancer. J Thorac Oncol. 2016;11:1204–23.
Dai C, Xie H, Kadeer X, Su H, Xie D, Ren Y, et al. Relationship of lymph node micrometastasis and micropapillary component and their joint influence on prognosis of patients with stage I lung adenocarcinoma. Am J Surg Pathol. 2017;41:1212–20.
Emoto K, Eguchi T, Vaghjiani R, Takahashi Y, Rekhtman N, Adusumilli P, et al. MA09.06 the newly recognized filigree pattern of micropapillary (MIP) lung adenocarcinoma (LADC) iS as Clinically Important as the classical pattern. J Thorac Oncol. 2018;13:S386–S7.
Fukutomi T, Hayashi Y, Emoto K, Kamiya K, Kohno M, Sakamoto M. Low papillary structure in lepidic growth component of lung adenocarcinoma: a unique histologic hallmark of aggressive behavior. Hum Pathol. 2013;44:1849–58.
Emoto K, Tan KS, Rekhtman N, Adusumilli PS, Travis WD. The newly described filigree pattern is an expansion of the micropapillary adenocarcinoma concept rather than a proposed new subtype. J Thorac Oncol. 2020;15:e121–4.
Thunnissen E, Flieder D. Morphologic logic: “filigree” and “classical” micropapillary pattern are orientation-dependent views of the same lesion. J Thorac Oncol. 2020;15:e120–1.
Funding
Supported by the grants from National Natural Science Foundation of China (81802256, 81902335) and the Fundamental Research Funds for the Central Universities (22120180607); the “Chen Guang” project was supported by Shanghai Municipal Education Commission and Shanghai Education Development Foundation (18CG19); and the “Outstanding young talent” project was supported by Shanghai Pulmonary Hospital (FKYQ1907) and Shanghai Rising-Star Program (20QA1408300) and Shanghai Hospital Development Center (SHDC2020CR4028).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Zhu, E., Xie, H., Gu, C. et al. Recognition of filigree pattern expands the concept of micropapillary subtype in patients with surgically resected lung adenocarcinoma. Mod Pathol 34, 883–894 (2021). https://doi.org/10.1038/s41379-020-00711-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41379-020-00711-8