Abstract
Small human lung specimens are frequently used for cell biological studies of the pathogenesis of emphysema. In general, lung function and other clinical parameters are used to establish the presence and severity of emphysema/chronic obstructive pulmonary disease without morphological analysis of the specimens under investigation. In this study we compared three morphological methods to analyze emphysema, and evaluated whether clinical data correlate with the morphological data of individual lung samples. A total of 306 lung specimens from resected lung(lobes) from 221 patients were inflated and characterized using three morphological parameters: the Destructive Index, the Mean Linear Intercept, and Section Assessment. Morphological data were related to each other, to lung function data, and to smoking behavior. Significant correlations (P < .001) were observed between Section Assessment and Destructive Index (r = 0.92), Mean Linear Intercept with Destructive Index (r = 0.69) and Mean Linear Intercept with Section Assessment (r = 0.65). Section Assessment, being much less time consuming than Mean Linear Intercept and Destructive Index, is the parameter of choice for initial analysis. Destructive Index is the most sensitive parameter. There was a significant (P < .001), but weak correlation for all three parameters with the diffusion capacity for CO (KCO) (Destructive Index: r = −0.28; Mean Linear Intercept: r = −0.34; Section Assessment: r = −0.32), and with FEV1/IVC (Destructive Index: r = −0.29; Mean Linear Intercept: r = −0.33; Section Assessment: r = −0.28), but not with other lung function parameters. A significant difference (P < .05) between (ex-) smokers and never-smokers was observed for Destructive Index and Section Assessment. It is concluded that the application of the three morphological parameters represents a useful method to characterize emphysematous lesions in a (semi-)quantitative manner in small human lung specimens, and that Section Assessment is a suitable and fast method for initial screening. The extent of emphysema of individual lung specimens should be established by means of morphometry, rather than lung function data.
Similar content being viewed by others
INTRODUCTION
Pulmonary emphysema is a progressive lung disease mostly affecting elderly people. Because emphysema is defined as “abnormal permanent enlargement of the air spaces distal to the terminal bronchioles, accompanied by destruction of their walls and without obvious fibrosis” (1, 2), characterization of the disease with morphological and/or morphometrical parameters is a prerequisite to study the pathogenesis. Although lung function tests are useful tools to diagnose chronic obstructive pulmonary disease, it is difficult to distinguish emphysema from other obstructive lung diseases (3). Characterization of the disease with functional parameters is controversial (4). The relations between lung function data and morphological/morphometrical data have been described as poor (5). Lung function data may not be representative for the part of the lung used for study. However, many data on the pathogenesis have been generated without a firm basis of thoroughly characterized lung tissue (6).
Even if the morphology of the specimen is known, immunohistochemical and biochemical studies on the pathogenesis of emphysema should be performed on tissue very close to that that has been morphologically characterized since emphysema is a very heterogeneous process. We therefore set up a large collection of lung tissue containing specimens derived from 221 individuals. Each specimen was divided into three small, adjacent parts. The middle part was used for morphological analysis, the two outer parts processed for molecular biological and immunohistological studies, to be conducted later. Morphological analysis was performed using two morphometric parameters: the Destructive Index as a measure for alveolar destruction (7), and the Mean Linear Intercept as a measure for air space enlargement (8). In addition, the Section Assessment parameter was selected for morphological grading of emphysematous lesions (9). Morphometric and morphological data were related to each other and to age, to lung function, and to smoking behavior.
PATIENTS AND METHODS
Patients
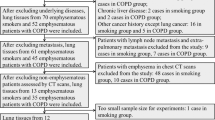
Lung specimens were obtained from patients undergoing lobectomy or pneumonectomy for a localized malignant pulmonary process, at the University Lung Center Nijmegen, or Rijnstate Hospital Arnhem, the Netherlands. All subjects were studied according to the guidelines of the Medical Ethical Committee of the University Medical Center Nijmegen; all patients had given informed consent. The collection of lung tissue consists of lung resection specimens from 221 patients. Of the original number of lung specimens from 282 patients (1 to 3 specimens per patient), specimens from 61 patients were excluded in this study. Of these excluded patients 2 were non-Caucasian, 2 had metastases in the specimens, 5 had been irradiated, 47 resulted in specimens that were not fully inflated and therefore not measurable, and 5 resulted in too few morphometric measurements.
Of the 221 patients 187 were male and 34 were female. In the male group 100 were current smokers, 67 were ex-smokers (abstinence from smoking for at least one year), 3 were never-smokers, and 17 had an unknown smoking history. In the female group 14 were smokers, 7 were ex-smokers, 6 were never-smokers, and 7 had an unknown smoking history. The average age of the entire group was 61.9 ± 11.1 years (range 24–84 y). Clinical data of patients are presented inTable 1.
Clinical Analysis
Lung function tests were performed before surgery. Static and dynamic lung function tests were performed with a wet spirometer and with a closed-circuit helium-dilution method (Pulmonet III, Sensormedics, Bilthoven, the Netherlands). Diffusion capacity for carbon monoxide per liter/lung (alveolar) volume (DL,CO/VA) was measured with the single breath-holding carbon monoxide method (Sensormedics 2450) and was corrected for actual hemoglobin. Measurements were performed at least 12 h after smoking. Predicted spirometric values were derived from the E.R.S. standards (10).
Tissue Processing
Small lung specimens (about 1 cc) were taken subpleurally from resected lung lobes at a maximum distance from the tumor the patient was operated for. Specimens were processed within 1–2 h after surgical removal. These specimens were free of tumor and inflammatory areas. Each specimen was cut in three pieces juxtaposed to each other, and of equal size. The middle part was inflated in phosphate-buffered saline (PBS) containing 4% (v/v) formalin under vacuum (13 kPa) for 20 min using a routine water stream-driven device (water aspirator), as described (11). The specimens were then dehydrated and embedded in paraffin. Sections (5 μm) were cut, and care was taken to prevent overstretching. The sections were stained with hematoxylin-eosin. One outer part was immediately frozen in liquid nitrogen and subsequently stored at −80°C for future biochemical and molecular-biological research. The other outer part was immersed in PBS, subsequently inflated under vacuum (13 kPa) for 20 min and then frozen in liquid nitrogen followed by storage at −80°C, for future immunohistochemical purposes.
Morphometry—Parenchymal Destruction
The degree of parenchymal destruction was determined by a microscopic point count technique (7). This so-called Destructive Index analysis was performed using a transparent sheet with 50 counting points (Fig. 1). The sheet was laid on an A5-size print, on which the microscopic images from the stained sections were projected using PC_Image 2.1® (Foster Findlay, Newcastle upon Tyne, United Kingdom) and Corel Photopaint 5.0® (Corel Corporation, Ottawa, Canada) software. Images free of large bronchi(oli), vessel, collapsed tissue, or extensive fibrosis were selected. The final magnification of the images was 82x. From each lung specimen, an average of 5 different sections was used, and in the sections generally 3 to 10 representative non-overlapping fields were selected, depending on the histomorphology of that section. Alveolar and duct spaces lying underneath the counting points were evaluated for the presence of destruction. Destruction was defined on base of one or more of the following criteria: (a) at least two alveolar wall defects, (b) at least two intraluminal parenchymal rags in alveolar ducts, (c) clearly abnormal morphology, or (d) classic emphysematous changes (7). Microscopic fields in which more than 20% of the points coincided with vessels, or conducting airways were excluded. Fields with alveolar and ductular spaces with a minimum diameter of more than 0.6 mm were also excluded. The percentage of all the points falling into the several categories of destroyed air spaces was computed to reveal the Destructive Index, using the formula [D/(D+N)] x100%, where D = destroyed, and N = normal. The measurements were done by one observer (AR), and for the intraobserver correlation 200 randomly selected prints were determined two times. A minimum of 3 prints per patient was measured. Generally, 750 counting points were analyzed per specimen with maxima up to 5000 points.
Morphometry—Air Space Enlargement
Enlargement of air spaces was evaluated in the Mean Linear Intercept measurement technique, originally described by Dunnill (8). The Mean Linear Intercept represents the average size of alveoli. The same printed images as described above were used. To measure the intercepts, a transparent sheet with 10 horizontal and 11 vertical lines was laid over the images (Fig. 2). The intercepts of alveolar walls with these lines were counted. Intercepts of bronchioli, blood vessels or septae were counted for one half since they are more or less part of the structure of surrounding alveolar spaces (8). Images with bronchi, large bronchioli or blood vessels were excluded from the measurements. Images showing compression of alveolar space - observed as meandering walls - were also excluded. Values were corrected for tissue shrinkage by measuring the dimensions before and after histological processing. The correction factor was 0.82, in accordance with data from Weibel (12). As with the Destructive Index, a minimum of 3 prints per specimen was analyzed. Generally, 2500 intercepts were counted per patient with maxima up to 18,000 intercepts.
Schematic representation of the Mean Linear Intercept analysis. A transparent sheet with 10 equally distributed horizontal lines is laid over the printed digitized image of a HE-stained section. A transparent sheet with 11 equally distributed vertical lines is used thereafter (not shown). For each line the intercepts with the tisue structures is counted according the criteria mentioned in the Methods section.
Morphology –Section Assessment
All sections used for morphometric analysis were determined for the degree of emphysema as represented by a panel of reference images as first described by Nagai et al. (9). Section Assessment (ranging from 0% (normal tissue) to 100% (complete destruction)) was evaluated microscopically at a low (25x) magnification. The Section Assessment value was expressed as an average percentage of severity of the lesions resulting from separate measurements of the sections. The average number of measured slides per patient was 6.
Statistical Analysis
Relations between the morphometric and morphologic results, and lung function data were analyzed with the 2-tailed Spearman’s rank correlation, and the Bonferroni correction for multiple comparisons (13). Statistical significance was accepted at the 0.05 level of confidence. Morphometric data from 306 lung specimens derived from 221 patients were compared with each other, with lung function data, and smoking behavior. All data were analyzed with SPSS 6.1.3 software (SPSS Inc., Chicago Ill., USA).
RESULTS
Morphological Data
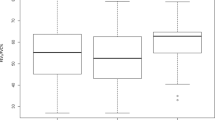
Lung specimens from 221 patients were studied with the Destructive Index, Mean Linear Intercept, and Section Assessment. The average Destructive Index was 60.5 ± 24.1% (mean ± SD; n = 306; range 4.3–99.5%). Analysis of lung parenchyma from young patients resulted in low Destructive Index values ranging from 5 to 20%, indicative for a proper measurement of alveolar destruction. The intraobserver correlation coefficient was 0.89 (n = 200, P < .001), representing a good reproducibility of the Destructive Index assessment. The average Mean Linear Intercept was 0.329 ± 0.059 mm (mean ± SD; n = 306; range 0.205–0.580 mm), and is comparable with values found by other groups (7, 14, 15). The intraobserver coefficient for Mean Linear Intercept was 0.98 (n = 200, P < .001). The average Section Assessment percentage was 59 ± 22% (mean ± SD; n = 306; range 5–90%). The intraobserver coefficient for Section Assessment was 0.94 (n = 200, P < .001). The Section Assessment values correlate with Destructive Index (r = 0.92, P < .001, Fig. 3). Destructive Index and Section Assessment show a similar pattern when related to Mean Linear Intercept (r = 0.69, P < .001 for Destructive Index vs. Mean Linear Intercept; r = 0.65, P < .001 for Section Assessment vs. Mean Linear Intercept; Figs. 4 and 5). The curves describing the relation between Mean Linear Intercept and Destructive Index, and Mean Linear Intercept and Section Assessment have a steep initial phase, indicating that Destructive Index and Section Assessment are more sensitive parameters with respect to disturbance of parenchymal lung architecture, compared to Mean Linear Intercept.
Relations between Morphological Data and Lung Function Data
Destructive Index, mean linear intercept, and Section Assessment were related to lung function data (TLC, IVC, RV, FEV1, FEV1/IVC, KCO; seeTable 2). Significant (P < .001; n = 221), but weak correlations for all three morphological parameters were found with KCO (Destructive Index: r = −0.28; Mean Linear Intercept: r = −0.34; Section Assessment: r = −0.32), and with FEV1/IVC (Destructive Index: r = −0.29; Mean Linear Intercept: r = −0.33; Section Assessment: r = −0.28). Mean Linear Intercept showed a significant but weak correlation with TLC (r = 0.29). Section Assessment showed a significant but weak correlation with TLC (r = 0.25) and VC (r = 0.26).
Relation between Morphological Data and Smoking Behavior
For Destructive Index and Section Assessment, a significant difference (P < .05) was observed between (ex-) smokers and never-smokers (Table 3). For Mean Linear Intercept no significant relation was found between (ex-)smokers and never-smokers.
DISCUSSION
In this study, 306 lung specimens derived from 221 patients were characterized thoroughly with morphological parameters. The specimens represent a broad range of parenchymal destruction and air space enlargement, ranging from normal to severe emphysema. The definition of pulmonary emphysema is based on morphological criteria, viz. parenchymal destruction and abnormal air space enlargement. We applied three indices to characterize the tissue morphologically. The simultaneous assessment of parameters reflecting destruction and air space enlargement for a reproducible characterization of emphysematous lesions has been explicitly recommended by Thurlbeck (16). The significant interrelationships of Destructive Index, Mean Linear Intercept, and Section Assessment indicate that morphological characterization of the lung collection with these three parameters results in a reliable approach to assess emphysematous lesions in a quantitative manner.
Destructive Index (DI)
Destructive Index has a high sensitivity in the determination of mild forms of emphysema (7). The average Destructive Index value of smokers and ex-smokers (69.2%; n = 188) is lower than the value of 79.2% (n = 41) found by Matsuba et al. (17), but higher than data reported in other studies: Saetta et al. (7) 47.1% (n = 31), Eidelman et al. (18) 49.1% (n = 23), Kuwano et al. (19) 34.8% (n = 28), and Willems et al. (20) 34.2% (n = 27). The higher Destructive Index values found in our study may be due to the high stringency of our measurement conditions, ruling out possible biases such as suboptimally inflated tissue. In addition, most specimens were sampled subpleurally, at a maximal distance from the tumor the patient was operated for. The stronger mechanical forces in the subpleural area during breathing may also have resulted in increased alveolar damage (18).
Mean Linear Intercept (Lm)
Mean Linear Intercept is a reflection of the mean air space diameter. This parameter was chosen to give additional information about alveolar abnormalities, observed as air space enlargement. The average value of Mean Linear Intercept of smokers (0.340 mm; n = 188) is lower than the values found by Matsuba et al. (17) 0.691 mm (n = 41), but comparable with those from Saetta et al. (7) 0.343 mm (n = 31), Eidelman et al. (18) 0.332 mm (n = 23), and Willems et al. (20) 0.343 mm (n = 27) We observed a significant correlation between Mean Linear Intercept and Destructive Index (r = 0.69, P < .001), in accordance with other studies (e.g., reference7). When Mean Linear Intercept is plottedversus Destructive Index, a steep initial phase is observed reflecting a more rapid increase of Destructive Index values as compared with the Mean Linear Intercept values (Fig. 4) This indicates that Destructive Index is a more sensitive parameter for parenchymal alterations. It supports the hypothesis (7) that destruction of lung tissue (reflected by increased Destructive Index) precedes the increase in the size of air spaces (reflected by increased Mean Linear Intercept). Saito et al. (5), however, postulated a parallel proceeding of alveolar destruction with air space enlargement.
Section Assessment (SA)
Section Assessment (9) reflects the morphological abnormalities at a low magnification using a panel of reference images. Analysis of Section Assessment is much less time consuming in comparison with Destructive Index and, to a lesser extent, Mean Linear Intercept. Section assessment takes about 5 min per specimen, whereas analysis of Destructive Index takes several hours (7). We observed a good correlation between Section Assessment and Destructive Index, and between section assessment and Mean Linear Intercept. This implies that analysis of section assessment may already indicate characteristics of the aging lung along with pathological abnormalities resulting in emphysema. Section Assessment may therefore be the parameter of choice for an initial morphological analysis of emphysematous lung specimens.
Relation with Lung Function Data
Values of Destructive Index, Mean Linear Intercept, and Section Assessment were poorly related to most lung function data. A poor correlation is predictable since lung function data reflects the condition of the lung as a whole, whereas the morphological data applies only to the specimen under investigation. Obviously, the specimens studied may not reflect the morphology of other parts of the lung. The process of emphysema is notoriously heterogenous in this respect. Parts of the lung characterized by destruction may be adjacent to parts that are morphologically normal or even fibrotic. Cell biological and immunohistochemical studies are, therefore, only meaningful if the specimens are well characterized with respect to morphology. Of the lung function data, only KCO and FEV1/IVC showed significant correlations with the three morphologic parameters. KCO is considered to be the most sensitive lung function parameter for emphysema, since it represents the effectiveness of gas exchange in alveolar tissue (10). FEV1/IVC, also known as the Tiffenau-index, is considered as a lung function parameter for chronic obstructive pulmonary disease since FEV1/IVC is a hallmark for obstruction of the airways (10).
Relation with Smoking Behavior
Both Destructive Index and Section Assessment show significant correlations with smoking behavior, whereas Mean Linear Intercept does not. The lack of correlation of Mean Linear Intercept with smoking behavior may be explained by the manifestation of senile emphysema, a natural occurring phenomenon in elderly people. The majority of our patients may already exhibit features of senile emphysema, as observed by increased alveolar diameter, and increased in patients with pulmonary emphysema (21).
CONCLUSION
In summary, 306 parenchymal lung samples from 221 patients were morphologically evaluated for emphysema using parameters for parenchymal destruction and air space enlargement. There was a poor correlation between morphological and most lung function data. It is concluded that for cell biological and immunohistochemical studies on the pathogenesis of emphysema, characterization of lung tissue specimens should be based on morphological evaluation rather than lung function data.
References
American Thoracic Society. The definition of emphysema. Report of the National Heart, Lung, and Blood Institute, Division of Lung Diseases workshop. Am Rev Respir Dis 1985; 132: 182–185.
American Thoracic Society. Definitions, epidemiology, pathophysiology, diagnosis, and staging. Am J Respir Crit Care Med 1995; 152: S78–S83.
Snider GL . Emphysema: the first two centuries and beyond. A historical overview, with suggestions for future research: Part 1. Am Rev Respir Dis 1992; 146: 1334–1344.
Nagai A, West WW, Paul JL, Thurlbeck WM . The National Institutes of Health Intermittent Positive-Pressure Breathing trial: pathology studies. I. Interrelationship between morphologic lesions. Am Rev Respir Dis 1985; 132: 937–945.
Saito K, Cagle P, Berend N, Thurlbeck WM . The “Destructive Index” in nonemphysematous and emphysematous lungs. Morphologic observations and correlation with function. Am Rev Respir Dis 1989; 139: 308–312.
Thurlbeck WM . Emphysema then and now. Can Respir J 1994; 1: 21–39.
Saetta M, Shiner RJ, Angus GE, Kim WD, Wang NS, King M, et al. Destructive Index: a measurement of lung parenchymal destruction in smokers. Am Rev Respir Dis 1985; 131: 764–769.
Dunnill MS . Quantitative methods in the study of pulmonary pathology. Thorax 1962; 17: 320–328.
Nagai A, Yamawaki I, Thurlbeck WM, Takizawa T . Assessment of lung parenchymal destruction by using routine histologic tissue sections. Am Rev Respir Dis 1989; 139: 313–319.
Quanjer PH, Tammeling GJ, Cotes JE, Pedersen OF, Peslin R, Yernault JC . Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur Respir J Suppl 1993; 16: 5–40.
Van Kuppevelt TH, Robbesom AA, Versteeg EMM, Veerkamp JH, Van Herwaarden CLA, Dekhuijzen PNR . Restoration by vacuum inflation of original alveolar dimensions in small human lung specimens. Eur Respir J 2000; 15: 771–777.
Weibel ER . Principles and methods for the morphometric study of the lung and other organs. Lab Invest 1963; 12: 131–155.
Bland JM, Altman DG . Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 1986; 1 (8476): 307–310.
Willems LN, Kramps JA, Stijnen T, Sterk PJ, Weening JJ, Dijkman JH . Antileukoprotease-containing bronchiolar cells. Relationship with morphologic disease of small airways and parenchyma. Am Rev Respir Dis 1989; 139: 1244–1250.
Hogg JC, Wright JL, Wiggs BR, Coxson HO, Saez AO, Pare PD . Lung structure and function in cigarette smokers. Thorax 1994; 49: 473–478.
Thurlbeck WM . Overview of the pathology of pulmonary emphysema in the human. Clin Chest Med 1983; 4: 337–350.
Matsuba K, Ikeda T, Nagai A, Thurlbeck WM . The National Institutes of Health Intermittent Positive-Pressure Breathing Trial: pathology studies. IV. The Destructive Index. Am Rev Respir Dis 1989; 139: 1439–1445.
Eidelman D, Saetta MP, Ghezzo H, Wang NS, Hoidal JR, King M, et al. Cellularity of the alveolar walls in smokers and its relation to alveolar destruction. Functional implications. Am Rev Respir Dis 1990; 141: 1547–1552.
Kuwano K, Matsuba K, Ikeda T, Murakami J, Araki A, Nishitani H, et al. The diagnosis of mild emphysema. Correlation of computed tomography and pathology scores. Am Rev Respir Dis 1990; 141: 169–178.
Willems LN, Kramps JA, Stijnen T, Sterk PJ, Weening JJ, Dijkman JH . Relation between small airways disease and parenchymal destruction in surgical lung specimens. Thorax 1990; 45: 89–94.
Verbeken EK, Cauberghs M, Mertens I, Clement J, Lauweryns JM, Van de Woestijne KP . The senile lung. Comparison with normal and emphysematous lungs. 1. Structural aspects. Chest 1992; 101: 793–799.
Acknowledgements
The authors express their gratitude to The Netherlands Asthma Foundation for their financial support (NAF project 95.44). The lung specimens were kindly provided by the Department of Lung Diseases, University Lung Center Nijmegen, the Department of Lung Diseases, Canisius-Wilhelmina Hospital (head: dr. J.P. Janssen), Nijmegen, and the Department of Pulmonary Diseases Rijnstate Hospital (head: dr. F.J.J. van den Elshout), Arnhem, The Netherlands. Assistance with the handling of the resected samples was kindly provided by the pathologists of the Departments of Pathology of University Medical Center, Nijmegen, and Canisius-Wilhelmina Hospital Nijmegen, The Netherlands. Assistance with statistical analysis was kindly provided by A.F.J. de Haan MSc, Dept. of Medical Statistics, University Medical Center, Nijmegen.
Antoine A. Robbesom, M.Sc., and Elly M.M. Versteeg were supported by Grant 95.44 from the Netherlands Asthma Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Robbesom, A., Versteeg, E., Veerkamp, J. et al. Morphological Quantification of Emphysema in Small Human Lung Specimens: Comparison of Methods and Relation with Clinical Data. Mod Pathol 16, 1–7 (2003). https://doi.org/10.1097/01.MP.0000043519.29370.C2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1097/01.MP.0000043519.29370.C2
Keywords
This article is cited by
-
A retinoid X receptor partial agonist attenuates pulmonary emphysema and airway inflammation
Respiratory Research (2019)
-
Astragalus polysaccharides mediated preventive effects on bronchopulmonary dysplasia in rats
Pediatric Research (2014)
-
Tumor necrosis factor-related apoptosis-inducing ligand translates neonatal respiratory infection into chronic lung disease
Mucosal Immunology (2014)
-
Neutral sphingomyelinase 2 deficiency is associated with lung anomalies similar to emphysema
Mammalian Genome (2012)
-
Activated charcoal filter effectively reduces p-benzosemiquinone from the mainstream cigarette smoke and prevents emphysema
Journal of Biosciences (2010)