Abstract
Angiogenesis is fundamentally required for the initialization, development and metastatic spread of cancer. A rapidly expanding number of new experimental, chemical modulators of endothelial cell function have been described for the therapeutic inhibition of angiogenesis in cancer. Despite this expansion, there has been very limited parallel growth of in vitro angiogenesis models or experimental tools. Here we present the Responsive Angiogenic Implanted Network (RAIN)-Droplet model and novel angiogenesis assay using an endothelial cell culture model of microvascular endothelial cells encapsulated in a spontaneously self-assembling, toroidal hydrogel droplet uniquely yielding discrete, pre-formed, angiogenic networks that may be embedded in 3D matrices. On embedding, radial growth of capillary-like sprouts and cell invasion was observed. The sprouts formed not only as outgrowths from endothelial cells on the surface of the droplets, but also, uniquely, from the pre-formed network structures within the droplet. We demonstrate proof of principle for the utility of the model showing significant inhibition of sprout formation (P<0.001) in the presence of bevacizumab, an anti-angiogenic antibody. Using the RAIN-Droplet assay, we also demonstrate a novel dose-dependent pro-angiogenic function for the characteristically anti-angiogenic multi-kinase inhibitor sorafenib. Exposure of endothelial cells in 3D culture to low, non-lethal doses (<1 μM) of sorafenib after initiation of sprouting resulted in the formation of significantly (P<0.05) more endothelial sprouts compared with controls over a 48-h period. Higher doses of sorafenib (5 μM) resulted in a significant (P<0.05) reduction of sprouting over the same time period. The RAIN-Droplet model is a highly versatile and simply constructed 3D focal sprouting approach well suited for the study of vascular morphogenesis and for preclinical testing of drugs. Furthermore, the RAIN-Droplet model has facilitated the discovery of a novel pro-angiogenic capacity for sorafenib, which may impact the clinical application and dosing regimen of that drug.
Similar content being viewed by others
Main
Uncontrolled and persistent angiogenesis is the hallmark of several diseases, including cancer, autoimmune diseases, age-related macular degeneration and atherosclerosis. Angiogenesis is the mechanism by which new vasculature forms from a pre-existing vascular bed. It requires cell migration through extracellular matrix, cell proliferation, individual cell differentiation and cell–cell interaction to form multicellular structures generally in response to secreted mediators.1 A broad range of fields now focus on angiogenesis as a discrete primary or controlling mechanism; however, functional cellular studies have been limited to a few established in vitro models. These may be conveniently divided into models of single cellular functions and models of multiple cellular functions able to differentiate responses of endothelial cells to varying growth conditions or exogenous mediators.2, 3 Single function models are generally based on chemotaxis or proliferation of endothelial cells on two-dimensional (2D) surfaces, while multiple function models generally combine chemotaxis with changes in cell differentiation, morphology, polarization or cell-to-cell interaction together combined in the formation of angiogenic capillary-like sprouting structures.3 The latter models are based on culture of isolated endothelial cells, defined co-cultures or ex vivo tissue in a supportive physiological 3D matrix such as collagen. Cells in vivo are surrounded by similar extracellular protein matrices; hence, in vitro culture in a 3D matrix is likely a better reflection of normal physiological growth conditions, particularly when primary cells are studied.2, 4
In addition to workable models for study of angiogenic mechanisms, successful anti-angiogenic drug development is dependent on the ability to assay the cellular effects of current drugs and functionally screen for future efficacious compounds. By 2007 there were at least 10 anti-angiogenic drugs approved for clinical use by the FDA and related international organizations.5 Beside these specific anti-angiogenic drugs, 40 other drugs in clinical trial by 2007 also possessed some anti-angiogenic capacity.5 Due possibly to complexity of construction, lack of flexibility or requirement for specialized equipment 3D angiogenesis models are rarely used as first-line assays in the literature, instead several 2D models predominate. Indeed, despite often elegantly reflecting angiogenic cellular morphogenesis, no 3D in vitro model seems to have challenged the 2D matrigel model of tube formation, the monolayer scratch-test assay or the modified Boyden chamber/transwell assay for initial assessment of angiogenic events.
Here we describe a novel 3D angiogenesis assay, the Responsive Angiogenic Implanted Network (RAIN)-Droplet assay, using an original angiogenesis model combining the flexibility, utility and ease of construction of current 2D assays, the physiological relevance of 3D cell growth and further creating a platform for a planar, radial, focal point-based assay protocol for quantification of endothelial sprouting. Uniquely, the RAIN-Droplet models angiogenic outgrowth of human dermal microvascular endothelial cells (HDMECs) from a defined structure bearing a pre-activated population of both single endothelial cells and multicellular structures. We show utility of the model in solid proof-of-principle assays of angiogenesis inhibitors in current clinical use. Finally, we use the model to uncover a novel facet of pro-angiogenic activity from the normatively anti-angiogenic multi-kinase inhibitor sorafenib.
MATERIALS AND METHODS
Cell Culture
HDMECs were obtained from Lonza and were maintained in EGM2-MV (Lonza, Walkersville, MD, USA). Lonza verify isolated endothelial cells by morphology and testing positive for acetylated low-density lipoprotein, positive for factor VIII and negative for α-smooth muscle actin.
Cell Preparation in Puramatrix
Puramatrix (PM) (BD Biosciences) cell suspension was made as directed by the manufacturer. Briefly, HDMECs were trypsinized and washed once in 10% sucrose solution at 4 °C to remove culture medium. All further manipulations were carried out on ice. Cells were counted by hemacytometer, placed in microcentrifuge tube and pelleted for 6 s at 16 000 r.c.f. Supernatant sucrose solution was carefully removed by pipette and the cells gently resuspended in ice-cold PM.
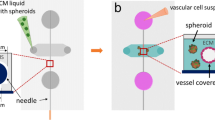
Droplet Formation and Implantation for RAIN-Droplet assay
Toroid formation is illustrated in Figure 1. Cells, 4 × 106 cells per ml, were suspended in 0.05% (w/v) PM. Cell suspension (3 μl) was drawn into the tip of a 20 μl pipette. Droplet volumes of 1–15 μl were achievable with this size of pipette tip, although 3 μl was routinely used for most assays. A droplet was formed at the end of the tip by gently depressing the pipette plunger to the first stop. Holding the pipette in a vertical position, the droplet was touched to the surface of complete cell culture medium causing the droplet to release and to instantly form a gel toroid. In most cases, this was performed in low attachment cell culture plates to avoid loss of cells to the plastic surface during longer term cultures.
Toroid contraction occurred over 24–72 h in floating culture. Collagen gels (Purecol, San Diego, CA, USA) (2.3 mg/ml, 0.5 ml per well) were precast in the wells of a 12-well plate as described by the manufacturer. Droplets were transferred to the gel surface using a 200 μl pipette tip with the end 5 mm cut or using a wide bore pipette tip. After placing the droplet on the gel, any excess medium was carefully removed by pipette, and collagen (0.1 ml per well) was placed on top of the lower collagen layer to sandwich the droplet. Collagen was set at 37 °C for 1 h in normal atmosphere. In some instances, growth factors were added to the upper layer before sandwiching the droplet. Finally, culture medium was layered over the gel.
For drug treatment studies, droplets were prepared as described and embedded in collagen with 50 ng/ml VEGF in the top layer (5 ng in 0.1 ml) of collagen. HDMECs were generally allowed to sprout for 24–72 h before drug addition, although where indicated droplets were occasionally treated immediately after embedding. Medium containing Avastin (Bevacizumab; Genentech Inc., South San Francisco, CA, USA) (25 μg/ml) was then layered onto the collagen. In sorafenib (LC Laboratories, Woburn, MA, USA) studies, the compound (5–5000 nM), diluted in medium, was layered onto the collagen. Samples were incubated at 37 °C, 5% CO2 for 24–48 h before counting sprout number.
Sprout Quantification
Sprouts were quantified under phase contrast microscopy. It was used for simplicity, although cells could be labeled as described below and then counted. For purposes of counting, sprouts were defined as multicellular capillary-like elongated structures radiating out from the RAIN-Droplet toroid and with the base of the sprout attached to the circumference of, or at a point within, the toroid. A start point was determined, generally at a ‘12 o’clock' position, and then sprouts were counted clockwise around the toroid until returned to the start position.
Sprouts were observed using an Olympus IMT-2 microscope with Olympus CK20 LWD C A 20PL × 20 objective ( × 200 final magnification). Image acquisition was performed using Evolution/QImaging microscope-mounted Digital Camera, CCD 2/3′′ ICX-282 with 2560 × 1960 resolution controlled by QCapture Pro image capture software (Media Cybernetics, Silverspring, MD, USA). Some images were converted to grayscale using grayscale conversion function on Photoshop 7.0, and no further image manipulation was used for brightfield photomicrographs.
Labeling of Droplets
Toluidine blue staining of embedded droplets: Embedded droplets were washed twice in PBS (MediaTech. Inc., Manassas, VA, USA), then fixed in 3.7% paraformaldehyde (USB, Cleveland, OH, USA) and again washed twice in PBS. Sufficient toluidine blue (Sigma/Aldrich, St Louis, MO, USA) in 0.1% methanolic solution was layered onto the gels to cover and incubated on the bench top for 2–5 min. The level of staining was monitored microscopically. To remove excess dye and destain the surrounding collagen, water was layered onto the surface of the gel, incubated for 5–10 min and then removed. This destain process was repeated if contrast between droplet and collagen was insufficient when viewed microscopically. Samples were then imaged under the phase contrast microscope system described above using bright field without the phase ring in place.
Fluorescent labeling of embedded droplets: Embedded droplets were stained by the actin probe Alexa Fluor 488 Phalloidin (Invitrogen) or by CellTracker Green (Invitrogen). Droplets were fixed in paraformaldehyde (3.7%), then washed twice in PBS and extracted with 0.1% Triton for 40 min in PBS before washing twice with PBS. Samples were blocked for 1 h with 0.1% albumin/0.2% fetal bovine serum at room temperature (RT) and then Alexa Fluor 488 Phalloidin (2 U per well) was added for 40 min at RT. Samples were washed in PBS and then layered with 50% Prolong Gold plus DAPI in PBS before imaging by confocal microscope.
For CellTracker staining, the embedded droplets were incubated with 10 μM CellTracker Green for 30 min, and then PBS for 15 min before fixation for 15 min with paraformaldehyde (3.7%). Samples were washed twice with PBS and then layered with 50% Prolong Gold plus DAPI in PBS before imaging by confocal microscope.
For immunohistochemical staining of sorafenib or control treated cells, droplets were prepared and allowed to sprout for 48 h before adding drug or vehicle, and subsequently culturing for up to a further 72 h. Then, the droplets were fixed in situ as for the fluorescent phalloidin staining above. Collagen disks containing embedded droplets were then popped out of the wells using a blunt spatula and the discs processed and embedded in paraffin. Slides were prepared from thin sections cut from the paraffin blocks and sent to the University of Michigan Cancer Center Research Histology and Immunoperoxidase Lab for commercial staining using Ki-67 (mouse) primary antibodies and ApopTag apoptosis labeling kit.
Equipment/Software Specifications for Confocal Images
The Olympus IX71 Fluoview 500 Laser Scanning Confocal Microscope running Olympus Fluoview image acquisition software version 4.3 bearing objective lens UPLAPO × 20 was used to capture the images using the following filters and dichroic mirrors: DM405/488; SDM490; BA430–460; and BA505IF. 3D reconstruction of confocal stacks, without volume or surface rendering, were performed automatically by opening Fluoview multi-Tif files under the Surpass option using the Imaris software (Bitplane Inc., St Paul, MN, USA). To better visualize the toroidal sprouting structure in solely Figure 4a, the green and blue channels were enhanced using Photoshop Variations option; original unaltered image is available for comparison on request. Volume rendering: following 3D reconstruction the Blend option was selected and Phalloidin 488 threshold was set to 800–1400. Surface rendering was performed for DAPI-stained nuclei by selecting the Surfaces option, setting Area Detail to 0.621 (smooth) and finally selecting Absolute Intensity threshold and setting to 955–3943. In all rendered images, gamma was unchanged. Finally, rendered images were visually compared with original captured microscopic image for fidelity. Full-image capture details are available, but withheld presently because of space requirements.
Transmission Electron Microscopy
Droplets were fixed in Karnovsky's fixative, a mixture of 3% paraformaldehyde and 2.5% glutaraldehyde in 0.1 M Sorensen's buffer, pH 7.4. After several buffer rinses, they were post-fixed for 1 h in 1% osmium tetroxide in the same buffer. They were then rinsed in double-distilled water to remove phosphate and then en bloc stained with aqueous 3% uranyl acetate for 1 h. Next, they were dehydrated in ascending concentrations of ethanol, treated with propylene oxide and embedded in Epon epoxy resin. Semi-thin sections were stained with toluidine blue for tissue orientation. Selected areas were ultra-thin sectioned 70 nm in thickness and stained with uranyl acetate and lead citrate. They were examined using a Philips CM100 electron microscope at 60 kV. Images were recorded digitally using a Hamamatsu ORCA-HR camera system operated using AMT software (Advanced Microscopy Techniques Corp., Danvers, MA, USA).
Deltavision Movie of Sprout Formation
Droplets embedded in collagen within chamber coverslips (Nunc, Rochester, NY, USA) were maintained at 37 °C, 5% CO2 in a humidified atmosphere for the duration of the experiment using a Weather Station (Precision Control LLC) cell culture environment designed for the Olympus IX-71 inverted microscope. Time-lapse images were captured and was controlled using SoftWoRx 3.5.1. Images were captured every 600 s. Video was also constructed from captured images using SoftWoRx 3.5.1 and converted to Quicktime file using MPEG Streamclip 2.1 for Windows Vista (http://www.squared5.com), where aspect ratio was changed from 768 × 768 to 320 × 240.
Sulforhodamine B Assay
The sulforhodamine B (SRB) cytotoxicity assay was used as described.6, 7 Briefly, primary HDMECs (Lonza) were seeded at 2.5 × 104 per well in a 96-well plate and allowed to adhere overnight. Drug or control was diluted in EGM2-MV (Lonza) and layered onto cells, which were allowed to incubate for times as indicated in the figures. Cells were fixed on the plates by the addition of cold trichloroacetic acid (10% final concentration) for 1 h at 4 °C. Cellular protein was stained by the addition of 0.4% SRB (Sigma/Aldrich, St Louis, MO, USA) in 1% acetic acid and incubation at RT for 30 min. Unbound SRB was removed by washing with 1% acetic acid and the plates were air-dried. Bound SRB was resolubilized in 10 μmol/l unbuffered Tris-base and absorbance was determined on a microplate reader at 560 nm (Genius; Tecan, Graz, Austria). Test results were normalized against initial plating density and drug-free controls.
Matrigel Assay
HDMECs were subject to the 2D matrigel cord formation assay. Matrigel was allowed to set in the wells and cells were added on top in the presence or absence of sorafenib (0.5 and 5 μM). After incubation for 24–72 h, the cells were photographed and the number of endothelial cords were counted manually using Image J (NIH) point counter. A cord was defined for quantification purposes as a discrete directional cord of cells stretching between two junction nodes.
Statistics
Statistics performed were one-way ANOVA on either SigmaStat 2.0 software (SPSS, Chicago, IL, USA) or Microsoft Excel software.
RESULTS
RAIN-Droplet Model
The following procedure was developed for the creation of toroidal droplet gels appropriate for 3D embedding in collagen. Cell suspensions in PM were drawn into the tip of a 20 μl pipette and the plunger of the pipette was depressed to form a droplet at the end of the tip. The droplet, gently touched to the surface of complete cell culture media in an ultra-low attachment plate, broke the surface tension of the culture medium and was released. A discrete, free-floating hydrogel scaffold was instantly formed encapsulating the cells with little or no observable loss of cells into the surrounding media, shown pictorially in Figure 1.
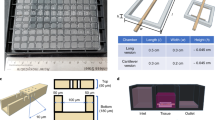
PM Concentration is Critical to Formation of Toroidal Gels
We hypothesized that the differential matrix resistance exerted on HDMEC by varying concentrations of PM would result in distinct droplet shapes. To test this, we prepared suspensions of fixed cell number in varying concentrations of PM. Interestingly, we found that PM concentration was closely linked to polymerized droplet shape and therefore also to the utility of the droplet in the RAIN-Droplet assay (Figure 2). Using 0.05% (w/v) hydrogel, encapsulating 4 × 106 cells per ml, consistent flat toroidal shapes with even cell distribution were created on droplet gelation (Figure 2). Regular, toroidal gel structures are unique to this method of mold-free droplet formation and were not achievable by running the droplet down the wall of the culture well. The above preparation was used for all experimental procedures, unless stated otherwise.
Formation of toroids was dependent on Puramatrix (PM) concentration (upper panels), scale bar 400 μm. Toroids formed from concentrations of 0.1% (w/v) PM and below. Toroids contracted as sprouting human dermal microvascular endothelial cell (HDMEC) networks were formed within the droplet. The same toroidal droplet is shown after 48 h incubation in culture medium (lower panel).
Contraction of the cell bearing toroidal 0.05–0.1% hydrogel structures was observed over the first 48 h, with little further change after this time (Figure 2, lower panel). This contraction event is in general agreement with Sieminski and co-workers,8 who observed that, in flat bed 1 and 2% PM gels, embedded endothelial cell reorganization induces gel contraction proportional to gel concentration.8
Characterization of Single and Multicellular Structures within Toroidal Droplet Gels
Distinct cellular features were revealed within the toroidal droplets using brightfield and transmission electron microscopy (TEM) (Figure 3a–c). Common to all analyzed droplets was a continuous cell coverage around the droplet circumference (Figure 3a, arrows). This coverage was characterized by cell–cell contacts displaying distinct electron-dense (darker) regions in the electron photomicrograph (Figure 3b, arrows). It appeared to develop over the 24–72 h toroid contraction period, while newly formed droplets did not appear to display a layer of contiguous cells at the gel surface. Significantly, the HDMEC within the toroids formed organized structures of two or more intact cells, often centered around large lumenal spaces free of extracellular matrix in many cases (Figure 3c, arrow). The exact nature of the cell–cell junctions and luminal spaces apparent in the droplets is subject to continuing investigation. However, the electron-dense regions at cell–cell interfaces were common and were suggestive of tight junctions (Figure 3b).
Brightfield and transmission electron micrographs of Responsive Angiogenic Implanted Network (RAIN)-droplets. (a) Continuous coverage of 0.05% Puramatrix (PM) toroid circumference by human dermal microvascular endothelial cells (HDMECs) (arrows), scale bar 200 μm. (b) Cell junctions at circumference; matrix is clearly visible within the toroid to left of cells. Arrows indicate electron-dense regions at cell–cell interface, scale bar 500 nm. (c) Structures in contracted toroids included a variety of cell structures, some bearing lumen-like vacuoles empty of surrounding matrix (arrow), scale bar 2 μm.
Characterization of Radial Capillary Sprouts after Collagen Embedding of Toroidal Droplet Gels
Sprouting was always preceded by invasion of a proportion of the endothelial cells into the surrounding matrix. An initial exploratory burst during the first 24–48 h accounted for the majority of the individual cell invasion with multicellular sprout formation beginning over 12–24 h post-embed (Supplementary video 1 online). In the video, one sprout is seen to form in the center of the field towards the end of the sequence. Interestingly, once initiated, the position of the sprouts generally did not change, but the cells contributing to the sprout changed rapidly during the initial formation stage. Cells were frequently observed using the sprout as a migratory route from the body of the droplet into the surrounding matrix (Supplementary video 1 online). Fluorescent labeling of HDMEC (Figure 4a and Supplementary video 2 online) show sprouts originating from both cells around the droplet circumference (Figure 4a, arrow) and the pre-existing endothelial cell network within the droplet (Figure 4a, arrow head). Sprouts could be maintained in culture for between 9 and 14 days with a change of media every second day, although for most routine testing or assay of sprout formation described in this study, 2–7 days were sufficient.
Responsive Angiogenic Implanted Network (RAIN)-Droplet model in 3D culture and assay for effect of angiogenesis inhibitors on endothelial sprouting. (a) Actin was labeled with Alexa Fluor 488 Phalloidin (green) and nuclear staining with 4′,6-diamidino-2-phenylindole (DAPI) (bright blue), representative of multiple labeling studies. Human dermal microvascular endothelial cell (HDMEC) sprouts originating from sprouting structures within the toroid (arrowhead) and from cells along the toroid circumference (arrow). The RAIN-Droplet toroid is visible as an arch at the top right of the panel bordered by arches of green actin phalloidin-stained cells. The droplet is potentially diffusely fluorescent because of either slight autofluorescence or differential retention of DAPI after labeling compared with the surrounding collagen. (b) Embedded RAIN-Droplet toroids were exposed to vascular endothelial growth factor (VEGF) (50 ng/ml) for 24 h and then bevacizumab (25 μg/ml) for up to 48 h. Scale bar is 100 μm. Bevacizumab (center panel) significantly inhibited endothelial sprouts compared with control (right panel) and caused marked attenuation of cell invasion (insets) (n=7–8, P<0.001).
Assay of Angiogenic Function using the RAIN-Droplet Model
As proof of principle of the RAIN-Droplet assay function, we treated embedded droplets with bevacizumab (Avastin; Genentech), an anti-VEGF antibody inhibitor of angiogenesis,9, 10 which resulted in a significant (n=7–8, P<0.001, representative of three independent assays) reduction in sprout number (Figure 4b, arrows indicate control sprouts in right panel). Using the RAIN-Droplet assay, we also found clear inhibition of endothelial cell invasion using sorafenib (LC Laboratories), a multi-kinase inhibitor and anti-angiogenic compound11 (Supplementary Figure 1 online). Quantification of invasion was not the primary aim of this study and unlike the sprouting it did not occur on a narrow horizontal plane. Although an efficient method for quantification of 3D invasion in this model is being investigated, the radial nature of the RAIN-Droplet assay provides clear visual evidence of differences in cellular invasion patterns in both bevacizumab- and sorafenib-treated samples (Figure 4b insets and Supplementary Figure 1). As proof of utility, we also showed that genetically manipulated cells could be used in the RAIN-Droplet model. Droplets were created from HDMEC engineered to overexpress the anti-apoptotic protein Bcl-2 by infection with a lentiviral vector bearing the bcl-2 gene sequence (Supplementary Figure 2). It may be seen that Bcl-2 overexpression produced highly prolific sprouting and cell invasion. Although clearly not optimized for quantification, this demonstrated the potential for study of cell signaling pathways using the RAIN-Droplet model.
Dose-Dependent Stimulation of Endothelial Angiogenesis by Sorafenib
Interestingly, we noted a surprising event after droplets were treated with sorafenib at varying concentrations after sprouting had been allowed to occur. It was clear that sorafenib appeared to have a directly dose-dependent inhibitory effect on single-cell invasion into collagen surrounding the droplet (Supplementary Figure 1). However, owing to limits of image resolution what may be unclear in the photographs is that the drug had a paradoxical stimulatory effect on endothelial sprout formation. To investigate this further, we performed an SRB proliferation assay to determine the sensitivity of HDMEC to sorafenib. It was determined that under normal culture conditions sorafenib at <1 μM had no significant inhibitory effect on HDMEC proliferation (Figure 5a). Above 1 μM sorafenib began to inhibit endothelial cell proliferation (Figure 5a). Importantly, when non-cytotoxic, low-dose sorafenib (0.5 μM) was administered for 48 h to droplets with pre-existing capillary sprouts, the number of sprouts increased significantly in number (P<0.05) and robustness (Figure 5b). When the same low dose of sorafenib was given before sprouting, normal sprout formation was significantly inhibited as expected (Figure 5c). Under both endothelial sprouting regimens, higher, cytotoxic doses of sorafenib (5 μM) significantly inhibited sprout formation (P<0.05) (Figures 5b and c). It is beyond the scope of this study to make a detailed investigation into the molecular signaling involved in this paradoxical process, but some observations may be made at the cellular level. In Figure 6, we present a time course of RAIN-Droplet sprouting and sprout anastomosis induced by initial exposure to VEGF in the presence or absence of sorafenib (0.5 μM). The difference in organizational level is clear with sorafenib treatment causing a rapid and, importantly, sustained aggregation of scattered cells into clearly aligned and robust multicellular sprouting structures. The control cells are also driven to form sprouts, but they are poorly organized and, without additional VEGF supplementation, do not maintain consistent structures (Figure 6). This comparison is highly representative of several separate experiments examining the effect of sorafenib on sprout structure. Immunohistochemical staining of sections cut from collagen-embedded droplets did not indicate any notable difference in expression of proliferation markers (Ki-67) or apoptosis markers (ApopTag) in sprouts exposed to sorafenib compared with controls (data not shown). Furthermore, when HDMECs were exposed to sorafenib in the traditional matrigel 2D cord formation assay, sorafenib-treated cells formed significantly more cords than controls (P≤0.01), whereas controls clearly displayed notably non-angiogenic cell growth as evidenced by the broad monolayer sheets of cells on the matrigel surface (Figure 7).
Concentration-dependent bi-phasic stimulatory and inhibitory effects of the multi-kinase inhibitor sorafenib on endothelial capillary sprout formation. (a) Proliferation assay for human dermal microvascular endothelial cells (HDMECs) exposed to varying concentrations of sorafenib. Cells were plated in 96-well plates in the presence or absence of sorafenib at indicated concentrations. Tetrazolium dye WST-1 was added at 24, 48 and 72 h to individual plates and absorbance was determined by microplate reader at 540 nm. Test readings were normalized against absorbance at initial plating density and also as a percentage of untreated time-point controls (n=6 for all points). (b) HDMECs were encapsulated in Responsive Angiogenic Implanted Network (RAIN)-Droplet gels and embedded in collagen with vascular endothelial growth factor ((VEGF) (5 ng in 0.1 ml collagen). Sorafenib was added to the wells in fresh culture medium after initial formation of capillary sprouts had occurred (24–72 h). Capillary sprout number was assessed by observation under high power microscope ( × 200). (c) HDMECs were treated as for panel b, but sorafenib was added immediately after embedding and before capillary sprout formation (n=4 for all sprouting assays data points).
Sorafenib promotes formation of robust endothelial sprouts during sprouting anastomosis between two Responsive Angiogenic Implanted Network (RAIN)-Droplets. Human dermal microvascular endothelial cells (HDMEC) were prepared for the RAIN-Droplet model as previously described and embedded in collagen containing vascular endothelial growth factor (VEGF) (50 ng/ml). Droplets were incubated 72 h to establish sprouts and were then treated with plus or minus sorafenib (0.5 μM) for a further 72 h with images of the same field captured every 24 h. Notably before treatment, the fields look very similar; however, the sorafenib appears to drive the HDMECs to rapidly organize and aggregate in one or two robust sprouts. The control cells form thinner, less coherent sprouts that become disorganized without further stimulation.
Effect of low concentration sorafenib on endothelial cell cord formation in the matrigel angiogenesis assay. Human dermal microvascular endothelial cells (HDMECs) were plated onto matrigel in the presence or absence of sorafenib (0.5 and 5 μM). Cells were incubated for up to 72 h with the same field being photographed per well every 24 h. Cord numbers were counted manually using the Image J (NIH) point counter function, n≥3 wells per concentration. Cords were defined as a discrete and linearly directional cord of cells stretching between two junction nodes. Sorafenib was found to increase cord number relative to controls with 5 μM sorafenib inducing significantly greater numbers of cords (P≤0.01). The color reproduction of this figure is available at the Laboratory Investigation journal online.
DISCUSSION
Conceptually, angiogenesis models that allow the use of a defined cell population are attractive for further defining specific reactivities or mechanisms related to physical, chemical or biological experimental stimuli. However, traditional culture of defined cell isolates or lines as 2D monolayers provide growth conditions relatively far removed from the normal physiological environment. Indeed, it is increasingly appreciated through gene expression analyses that the interface between the cell and the culture surface may significantly affect protein secretion and thus cell function and response to changes in external conditions.12 Thus, conditions that mimic the normal 3D environment of the cell population, while still not a replacement for the in vivo milieu, may provide a better reflection of the normal physiological state.13 Previous attempts at making discrete endothelial cell-bearing vehicles for 3D endothelial sprouting and invasion have generally but not exclusively taken three directions. The simplest are variations on casting single-cell suspensions of endothelial cells in matrices such as collagen.14 In some instances, cells are suspended in a gel cast within an especially designed mold, but other protocols cast the gels in plates from which areas of gel are punched out with specialized equipment. Both methods produce discrete, large and fragile gel discs with usage primarily limited by the physical nature of the discs.
Foci for angiogenic sprouting have also been created by growing endothelial cells on cell culture-compatible microcarrier beads, the bead effectively acting as a culture surface.15 This may be performed by incubating endothelial cells in specialized stirring flasks for a number of days. The coated beads are then embedded in a surrounding matrix allowing cell invasion and sprouting.4, 15
The third distinct platform for production of discrete 3D endothelial sprouting foci is a derivative of the well-described tumor spheroid protocol. Tumor cells will aggregate if prevented from adhering to a culture surface, and ultimately the aggregated cells will order into spheroid. Endothelial cells do not normally form spheroids and rapidly die by anoikis if prevented from attaching. By suspending endothelial cells under very precise conditions in a highly viscous medium, providing limited physical support, the cells are able to survive and migrate towards each other to form endothelial spheroids.16 The spheroids are initially loose cell aggregates that readily dissociate if cultured in 2D or 3D conditions. However, if allowed to mature over a period of up to 7 days, the surface cells form a discrete monolayer of differentiated and polarized cells, while spontaneous apoptosis and necrosis inside the spheroid result in a virtually cell-free lumenal void.16
We utilized distinctive properties of a nanoscale self-assembling hydrogel, PM (BD Biosciences), to encapsulate HDMEC in free-toroidal droplets suitable for implantation in biological matrices. Uniquely within this class of in vitro model, the RAIN-Droplets contain a heterogeneous population of angiogenically activated endothelial cells forming a branching and active network of endothelial cell structures that include capillary sprouts, multicellular spheroidal foci and active single cells. The toroidal RAIN-Droplets are simple to create, require only common laboratory equipment for preparation and provide a novel platform for in vitro study of angiogenesis.
PM is composed of 16-mer peptide chains in 1% (w/v) aqueous solution.17 This matrix instantly and spontaneously organizes into a nanoscale scaffold under physiological conditions. It promotes survival and maintains angiogenic activity of endothelial cells.8, 17 Until now, PM has been used primarily as a replacement for extracellular matrices in cell monolayer, embedded cell suspensions or transwell invasion studies.18, 19 Although microfluidic protocols have also taken advantage of the unusual polymerization properties of the hydrogel.20
Notably, a far lower concentration of PM, ∼10-fold lower, was used here than is described for any other applications of the hydrogel in the available literature.8, 17, 18, 19, 20 Above 0.1% hydrogel concentrations, inconsistent shapes were obtained (Figure 2), and above 0.2%, uneven comet-shaped pellets were generally formed (Figure 2). Importantly, low concentration conditions allowing adequate toroidal gel contraction were critical for creating droplets suitable for the angiogenesis assay. While culture plates bearing toroidal gels could be carefully moved immediately after droplet formation, direct manipulation or excessive shaking readily disrupted newly formed toroids of 0.05–0.1% PM. However, incubation under normal cell culture conditions allowed gel contraction, over 24–72 h, and consistently resulted in rigid toroids that could be transferred by pipette without disruption. Thus, 4 × 106 cells per ml in 0.05% (w/v) hydrogel produced consistent, tightly contracted, evenly shaped toroids bearing complex populations of HDMECs suitable for study or assay of angiogenic activity.
The resulting toroidal droplet gels were robust showing little obvious disruption under normal cell culture handling procedures. Droplets were easily harvested using a wide bore, 200 μl pipette tip or a regular 200 μl pipette tip with the end 4–5 mm cut. For use in the assay of angiogenesis modulation, the droplets were then embedded between two layers of collagen gel (Figure 1). Embedding gels could be formed with or without added pro-angiogenic stimuli (eg VEGF, bFGF). It was most economical and sufficient to add the growth factors to the top layer of gel alone. This format maintained sprouting activity using the smallest amount of growth factor. Implanted sprouting droplets could be consistently maintained in the presence of growth factors for up to 9 days and often up to 2 weeks with care and bi-daily changes of VEGF supplemented medium. Despite the inherent variability and limited culture capacity of primary cells compared with immortalized cell lines, for example, the RAIN-Droplet assay has been consistent enough in our hands to say that 7–9 days survival is repeatedly achievable with sprouts formed from healthy endothelial cells. Longer times are achievable and are indeed likely for low passage number, highly viable human microvascular endothelial cells.
The initial cell invasion events of the RAIN-Droplet model after embedding droplets in collagen are currently being investigated with a view to quantitatively assaying invasion concurrently with sprout formation. This is a unique function within the existing engineered 3D angiogenesis models. Even without numerical quantification, the RAIN-Droplet model allowed a very clear qualitative assessment of drug effects on endothelial cell invasion. The primary concern with determining invasion is that unlike the capillary sprouts, which virtually all grow out along the horizontal plane of the RAIN-Droplet-like spokes on a wheel, the single invading cells have a tendency to spread the full depth of the collagen embedding gel.
Quantification of unstained sprouts was easily accomplished using phase contrast microscopy. As mentioned above and distinct from other 3D angiogenesis models, the sprouts extended out from the toroid within a relatively narrow plane making quantification of sprout number or length relatively easy. By their nature bead-based or spheroid-based 3D models of angiogenesis produce multi-directional sprouts around the entire spherical structure, while in the RAIN-Droplet model virtually all the sprouts radiated horizontally out along the plane of the toroidal droplet gel and were readily visible within virtually the same focal plane of a medium to high power microscope lens ( × 50–200 magnification). Alternatively, samples were fixed with paraformaldehyde at RT, washed with water, stained with toluidine blue and viewed under a brightfield microscope. In both instances, sprouts viewed at × 200 magnification were clearly discerned and could be counted by eye around the full circumference of the toroid. Endothelial sprouts were defined for the purposes of this study as robust single or multicellular structures radiating out from the toroid, but being attached to the toroid at their base. With particular respect to imaging sprouts, this horizontal, radial sprouting protocol is a significant improvement over most previous matrix-embedded models that generally require cross-sectioning of the gel to clearly view endothelial sprouts.14
In evaluating the RAIN-Droplet model for its potential as an assay for angiogenesis, we tested two known angiogenesis inhibitors. Both bevacizumab and sorafenib are in active clinical trials, and the mechanisms of action have been well described for both drugs.9, 10, 11 As expected, bevacizumab, the anti-VEGF antibody, was highly effective at inhibition of sprouts over a period of 24–72 h in the presence of up to 50 ng/ml VEGF contained in the embedding gel. Sorafenib was very effective at inhibiting de novo growth of endothelial capillary sprouts, markedly inhibiting virtually all signs of cell invasion from the droplets into the surrounding collagen. However, when the same concentrations of sorafenib were tested on droplets that had been allowed to initiate capillary sprout formation into the collagen, a paradoxical increase in sprout number was observed. Indeed, microscopic examination revealed that these new structures were highly robust, thick sprouts comprised of apparently more cells than the control sprouts. It was determined that the sorafenib concentration consistently inducing significantly more sprouts that persisted over time (0.5 μM) was insufficient to affect cell proliferation over the same period. Thus, the multi-kinase inhibitor sorafenib appears to display both anti-angiogenic and pro-angiogenic activity dependent on concentration of the drug and on the maturity of the capillary sprouts. It may be assumed that existing in vitro assays of sorafenib have failed to differentiate this important bi-phasic function of sorafenib on angiogenesis activation as there is no other discussion of it in the literature. Indeed surprisingly, little literature describes pre-clinical in vitro anti-angiogenesis testing of sorafenib; primarily it has included in vivo treatment and assessment of anti-angiogenic effect on xenograft models. That in vitro literature, which is available typically, uses concentrations of sorafenib well above the 0.5 μM concentration limit we observe here for stimulatory effects on angiogenesis.21, 22, 23
However, the observation of a paradoxical stimulatory effect of sorafenib on endothelial cells is in agreement with very recent observations by Rose and co-workers,24 who describe a stimulatory effect of sorafenib on a variety of bladder cancer cell lines in the same dose range as this study shows the stimulatory effects on endothelial cells. Rose and co-workers24 also examined renal cancer cells but did not observe the same stimulation, suggesting that the stimulatory effects of sorafenib are cell specific.24 The results of sorafenib activity on the RAIN-Droplet model suggest that endothelial cells actively undergoing angiogenic sprout formation are among the cell types sensitive to this bi-phasic drug activity. Indeed, the 2D matrigel cord formation angiogenesis assay confirms the sprouting phenotype seen in the RAIN-Droplet model as it also demonstrates an increase in endothelial cord number by cells exposed to sorafenib. It should be noted that in the matrigel assay, 5 μM sorafenib significantly increased cord number, whereas it was decreased in the RAIN-Droplet model. While the paradoxical pattern of sorafenib induced sprouting increase was confirmed, the disparity between the effects of 5 μM sorafenib in the RAIN-Droplet model compared with the matrigel assay is likely due to the short-term protective quality of growth factors present in the matrigel, which is a non-defined extracellular matrix. It may also potentially be due to batch-to-batch variation inherent in primary cells such as the HDMECs. Importantly, these initial findings from the 3D RAIN-Droplet model for angiogenesis, in conjunction with those of Rose and co-workers,24 may have significant implications for the choice of dosing schedule used in therapeutic application of sorafenib. Furthermore, they warrant continued investigation, because identification of a common mechanism would allow better classification of stimulation sensitive cell lines and potential development of compounds that could bypass this effect.
The RAIN-Droplet assay utilizes an innovative, flexible, planar, focal point-based 3D angiogenesis sprouting model. In addition to endothelial cell sprouting, this focal point-based approach to the assay of migrating and invading cells has wider potential for any cells able to expand or migrate into a 3D matrix material. The RAIN-Droplet assay combines the ease of construction of 2D gel assays with the physiological relevance of more complex 3D angiogenesis assays. Radial sprouting from a focal point within a narrow plane allows visual sprout quantification by the simplest of microscopical techniques, but readily translates to more complex imaging methodologies. Notably, the RAIN-Droplet model allowed us to observe and quantify a new function of a known compound that had not been described to date in other angiogenesis assays. An easily performed 3D culture protocol such as that of the RAIN-Droplet assay would provide a novel, accessible model for in vitro angiogenesis and expands the fine but limited repertoire of in vitro angiogenesis screening assays.
References
Nagy JA, Dvorak AM, Dvorak HF . VEGF-A and the induction of pathological angiogenesis. Annu Rev Pathol 2007;2:251–275.
Staton CA, Stribbling SM, Tazzyman S, et al. Current methods for assaying angiogenesis in vitro and in vivo. Int J Exp Pathol 2004;85:233–248.
Taraboletti G, Giavazzi R . Modelling approaches for angiogenesis. Eur J Cancer 2004;40:881–889.
Goodwin AM . In vitro assays of angiogenesis for assessment of angiogenic and anti-angiogenic agents. Microvasc Res 2007;74:172–183.
Folkman J . Angiogenesis: An organizing principle for drug discovery? Nat Rev Drug Discov 2007;6:273–286.
Zeitlin BD, Spalding AC, Campos MS, et al. Metronomic small molecule inhibitor of bcl-2 (TW-37) is antiangiogenic and potentiates the antitumor effect of ionizing radiation. Int J Radiat Oncol Biol Phys 2010;78:879–887.
Ashimori N, Zeitlin BD, Zhang Z, et al. TW-37, a small-molecule inhibitor of bcl-2, mediates S-phase cell cycle arrest and suppresses head and neck tumor angiogenesis. Mol Cancer Ther 2009;8:893–903.
Sieminski AL, Was AS, Kim G, et al. The stiffness of three-dimensional ionic self-assembling peptide gels affects the extent of capillary-like network formation. Cell Biochem Biophys 2007;49:73–83.
Bevacizumab anti-VEGF monoclonal antibody, avastin, rhumab-VEGF. Drugs RD 2002;3:28–30.
Stahl A, Paschek L, Martin G, et al. Combinatory inhibition of VEGF and FGF2 is superior to solitary VEGF inhibition in an in vitro model of RPE-induced angiogenesis. Graefes Arch Clin Exp Ophthalmol 2009;247:767–773.
Lyons JF, Wilhelm S, Hibner B, et al. Discovery of a novel raf kinase inhibitor. Endocr Relat Cancer 2001;8:219–225.
Li GN, Livi LL, Gourd CM, et al. Genomic and morphological changes of neuroblastoma cells in response to three-dimensional matrices. Tissue Eng 2007;13:1035–1047.
Tibbitt MW, Anseth KS . Hydrogels as extracellular matrix mimics for 3D cell culture. Biotechnol Bioeng 2009;103:655–663.
Davis GE, Black SM, Bayless KJ . Capillary morphogenesis during human endothelial cell invasion of three-dimensional collagen matrices. In Vitro Cell Dev Biol Anim 2000;36:513–519.
Nehls V, Drenckhahn D . A novel, microcarrier-based in vitro assay for rapid and reliable quantification of three-dimensional cell migration and angiogenesis. Microvasc Res 1995;50:311–322.
Korff T, Augustin HG . Integration of endothelial cells in multicellular spheroids prevents apoptosis and induces differentiation. J Cell Biol 1998;143:1341–1352.
Narmoneva DA, Oni O, Sieminski AL, et al. Self-assembling short oligopeptides and the promotion of angiogenesis. Biomaterials 2005;26:4837–4846.
Shirai K, Ishisaki A, Kaku T, et al. Multipotency of clonal cells derived from swine periodontal ligament and differential regulation by fibroblast growth factor and bone morphogenetic protein. J Periodontal Res 2009;44:238–247.
Wang S, Nagrath D, Chen PC, et al. Three-dimensional primary hepatocyte culture in synthetic self-assembling peptide hydrogel. Tissue Eng Part A 2008;14:227–236.
Kim MS, Yeon JH, Park JK . A microfluidic platform for 3-dimensional cell culture and cell-based assays. Biomed Microdevices 2007;9:25–34.
Murphy DA, Makonnen S, Lassoued W, et al. Inhibition of tumor endothelial ERK activation, angiogenesis, and tumor growth by sorafenib (BAY43-9006). Am J Pathol 2006;169:1875–1885.
Plastaras JP, Kim SH, Liu YY, et al. Cell cycle dependent and schedule-dependent antitumor effects of sorafenib combined with radiation. Cancer Res 2007;67:9443–9454.
Wustehube J, Bartol A, Liebler SS, et al. Cerebral cavernous malformation protein CCM1 inhibits sprouting angiogenesis by activating DELTA-NOTCH signaling. Proc Natl Acad Sci USA 2010;107:12640–12645.
Rose A, Grandoch M, vom Dorp F, et al. Stimulatory effects of the multi-kinase inhibitor sorafenib on human bladder cancer cells. Br J Pharmacol 2010;160:1690–1698.
Acknowledgements
We thank Chris Edwards and Shelley Almburg for great help with confocal imaging and digital volume rendering and Dotty Sorenson for TEM study. We also thank Professor I.J. Zeitlin for his comments on reading the manuscript, Chris Jung for illustration and Chris Strayhorn for preparation of slides for immunocytochemistry. Finally, we thank Dr Kristy Meyers for her time and help growing the HDMEC-Bcl-2. This work was supported by Grant P50-CA97248 (University of Michigan Head and Neck SPORE) from the NIH/NCI, and Grants R01-DE14601, R01-DE15948, R01-DE16586, R21-DE19279 and R01-DE021139 from the NIH/NIDCR (JEN).
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Laboratory Investigation website
A novel three-dimensional model for angiogenesis is applied to investigate biological and pharmacological changes in endothelial sprouting due to the anti-angiogenic tyrosine kinase inhibitor, sorafenib. Unexpectedly, a paradoxical, dose-dependent, pro-angiogenic effect is observed that may impact the clinical application and dosing regimen of the drug.
Rights and permissions
About this article
Cite this article
Zeitlin, B., Dong, Z. & Nör, J. RAIN-Droplet: a novel 3D in vitro angiogenesis model. Lab Invest 92, 988–998 (2012). https://doi.org/10.1038/labinvest.2012.77
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/labinvest.2012.77
Keywords
This article is cited by
-
In vitro 3D angiogenesis assay in egg white matrix: comparison to Matrigel, compatibility to various species, and suitability for drug testing
Laboratory Investigation (2014)
-
Endothelial cells expressing low levels of CD143 (ACE) exhibit enhanced sprouting and potency in relieving tissue ischemia
Angiogenesis (2014)