Abstract
OBJECTIVE
To retrospectively determine mean arterial pressure (MAP) for stable concordant and discordant triplets during the first 7 days of life.
BACKGROUND
Morbidity and mortality for prematurely born triplets is high, therefore, MAP monitoring during the first day of life is important for their clinical management. MAP reference values for special populations such as triplets have not been published. Recently, we reported that in stable discordant twins MAP values during the first day of life were significantly lower in the smaller than in their larger siblings. Comparable information for triplets is not available.
DESIGN
Retrospective cohort study.
METHODS
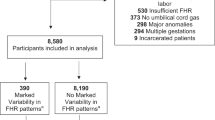
We studied 30 sets of concordant and 29 sets of discordant (birth weight difference ≥20%) consecutively born triplets. Stable patients were defined as those having umbilical cord hemoglobin ≥13 g/dl, normal blood gases, who were never treated for hypotension, and survived at least 7 days. MAP (torr) were measured by oscillometry in 3410, and by transducer via an umbilical arterial catheter in 1251 instances.
RESULTS
Concordant and discordant triplets were similar in demographics, history of preterm labor (63 and 63%), chorioamnionitis (10 and 10%), pre-eclampsia (53 and 48%), cesarean delivery (100 and 100%), antenatal steroids (77 and 73%), cord hemoglobin (16 and 16 g/dl), combined triplets birth weight (4922 and 4732 g), gestational age (32 and 33 weeks), normal head ultrasounds or Grade I intracranial hemorrhage (96 and 100%) and neonatal mortality (2 and 1%), but were different in the number of infants requiring mechanical ventilation (57 and 31%). A total of 80 (89%) concordant triplets and 77 (88%) discordant triplets were stable according to our definition. Concordant stable triplets, whether small, medium or large, had similar MAP at birth. Their MAP values increased noticeably from birth to 24 hours and more subtlely to 7 days. Triplets of ≤32 weeks GA had lower MAP throughout than those of ≥33 weeks GA. Discordant stable triplets were divided into 27 small (1382 g), 26 medium (1683 g) and 27 large (1969 g); during the first 24 hours, medium and smaller triplets had MAP values that were lower than those of their larger siblings. From the second to the seventh day of life, all MAP values and trends were similar. Among discordant triplets, 86% of the smallest, 13% of the medium and 13% of the largest infants had asymmetrical intrauterine growth restriction.
CONCLUSION
In stable concordant and stable discordant triplets, MAP correlates with birth weight, gestational age and postnatal age. MAP values increase noticeably during the first 24 hours and more subtlely during the next 7 days. Concordant or discordant, small, medium, and large triplets have similar MAP values and trends to that of their siblings. Small and medium discordant triplets have lower MAP values during the first day of life than their larger siblings but by the second day there MAP trends and values were no longer different.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Wright VC, Schieve LA, Reynolds MA, Jeng G, Kissin D . Assisted reproductive technology surveillance — United States, 2001. MMWR 2004;53:1–20.
Kaufman GE, Malone FD, Harvey-Wilkes KB, Chelmow D, Penzias AS, E'Alton ME . Neonatal morbidity and mortality associated with triplet pregnancy. Obstet Gynecol 1998;91:342–348.
Shieve LA, Meilke SF, Ferre C, Peterson HB, Jeng G, Wilcox LS . Low and very low birth weight in infants conceived with use of assisted reproductive technology. N Engl J Med 2002;346:731–737.
Miall-Allen VM, de Vries LS, Dubowitz LMS, Whitelaw AGL . Blood pressure fluctuation and intraventricular hemorrhage in the preterm infant of less than 31 weeks' gestation. Pediatrics 1989;83:657–661.
Watkins AMC, West CR, Cooke RWI . Blood pressure and cerebral haemorrhage and ischaemia in very low birth weight infants. Early Hum Dev 1989;19:103–110.
Bada HS, Korones SB, Perry EH, et al. Mean arterial blood pressure changes in premature infants and those at risk for intraventricular hemorrhage. J Pediatr 1990;117:607–614.
Low JA, Froese AB, Galbraith RS, Smith JT, Sauerbrei EE, Derrick EJ . The association between preterm newborn hypotension and hypoxemia and outcome during the first year. Acta Paediatr 1993;82:433–437.
Cunningham S, Symon AG, Elton RA, Zhu C, McIntosh N . Intra-arterial blood pressure reference ranges, death and morbidity in very low birth weight infants during the first seven days of life. Early Hum Dev 1999;56:151–165.
Gill AB, Weindling AM . Echocardiographic assessment of cardiac function in shocked very low birth weight infants. Arch Dis Child 1993;68:17–21.
Seri I, Evans J . Controversies in the diagnosis and management of hypotension in the newborn infant. Curr Opin Pediatr 2001;13:116–123.
Cordero L, Timan CJ, Waters HH, Sachs LA . Mean arterial pressures during the first 24 hours of life in ≤600 gram birth weight infants. J Perinatol 2002;22:348–353.
Cordero L, Johnson JR . Mean arterial pressure in extremely low birth weight concordant and discordant twins during the first day of life. J Perinatol 2002;22:526–534.
Cordero L, Giannone PJ, Rich JT . Mean arterial pressure in very low birth weight (801 to 1500 g) concordant and discordant tiwns during the first day of life. J Perinatol 2003;23:545–551.
Entezami M, Runkel S, Becker R, Weitzel HK, Arabin B . Feto-feto-fetal triplet transfusion syndrome (FFFTTS). J Matern Fetal Med 1997;6:334–337.
Victoria A, Mora G, Arias F . Perinatal outcome, placental pathology, and severity of discordance in monochorionic and dichorionic twins. Obstet Gynecol 2001;97:310–315.
Sherer DM . Adverse perinatal outcome of twin pregnancies according to chorionicity: review of the literature. Am J Perinatol 2001;181:23–37.
Alexander GR, Kogan M, Martin J, Papiernik, E . What are the fetal growth patterns of singletons, twins, and triplets in the United States. Obstet Gynecol 1998;41:115–125.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of the subependymal intraventricular hemorrhage: a study of infants with weights less than 1500 g. J Pediatr 1978;92:529–534.
Versmold HT, Kitterman JA, Phibbs RH, Gregory GA, Tooley WH . Aortic blood pressure during the first 12 hours of life in infants with birth weight 610 to 4,220 grams. Pediatrics 1981;67:607–613.
Park MK, Menard SM . Accuracy of blood pressure measurement by the Dinamap monitor in infants and children. Pediatrics 1987;79:907–914.
Spinazzola RM, Harper RG, de Soler M, Lesser M . Blood pressure values in 500- to 750-gram birth weight infants in the first week of life. J Perinatol 1991;11:147–151.
Hegyi T, Carbone MT, Anwar J, et al. Blood pressure ranges in premature infants I. The first hours of life. J Pediatr 1994;124:627–633.
Hegyi T, Anwar M, Carbone MT, et al. Blood pressure ranges in premature infants: II. The first week of life. Pediatrics 1996;97:336–342.
Nuntnarumit P, Yang W, Bada-Ellzey HS . Blood pressure measurements in the newborn. Clin Perinatol 1999;26:981–996.
Al-Aweel I, Pursley DM, Rubin LP, Shah B, Weisberger S, Richardson DK . Variations in prevalence of hypotension, hypertension, and vasopressor use in NICUs. J Perinatol 2001;21:272–278.
Evans N, Moorcraft J . Effect of patency of the ductus arteriosus on blood pressure in very preterm infants. Arch Dis Child 1992;67:1169–1173.
Zubrow AB, Hulman S, Kushner H, Falkner B . Determinants of blood pressure in infants admitted to neonatal intensive care units: a prospective multicenter study. J Perinatol 1995;15:470–479.
Lee J, Rajadurai VS, Tan KW . Blood pressure standards for very low birth weight infants during the first day of life. Arch Dis Child 1999;81: F168–F170.
Tan KL . Blood pressure in very low birth weight infants in the first 70 days of life. J Pediatr 1998;112:266–270.
Segar JL . Neural regulation of blood pressure during fetal and newborn life In: Polin RA, Fox WW, Abman SH, editors. Fetal and Neonatal Physiology. Pennsylvania: Saunders; 2004. p. 717–726.
Sasidharan P . Role of corticosteriods in neonatal blood pressure homeostasis. Clin Perinatol 1998;25:723–740.
Rizzo G, Arduini D, Romanini C . Cardiac and extracardiac flows in discordant twins. Am J Obstet Gynecol 1994;170:1321–1327.
Ezra Y, Jones J, Farine D . Umbilical artery waveforms in triplet and quadruplet pregnancies. Gynecol Obstet Invest 1999;47:239–243.
McMillen IC, Adams MB, Ross JT, et al. Fetal growth restriction: adaptations and consequences. J Reprod Fertil 2001;122:195–204.
Figueras F, Puerto B, Martinez JM, Cararach V, Vanrell JA . Cardiac function monitoring of fetuses with growth restriction. Eur J Obstet Gynecol Reprod Biol 2003;110:159–163.
Cheung YF, Taylor MJO, Fisk NM, Redington AN, Gardiner HM . Fetal origins of reduced arterial distensibility in the donor twin in twin–twin transfusion syndrome. Lancet 2000;355:1157–1158.
Bajoria R, Sullivan M, Fisk NM . Endothelin an association with cardiac dysfunction in the recipient fetus of twin-twin transfusion syndrome. Hum Reprod 1999;14:1614–1618.
Edwards LJ, Simonetta G, Owens JA, Robinson JS, McMillen IC . Restriction of placental and fetal growth in sheep alters fetal blood pressure responses to angiotensin II and captopril. J Physiol 1999;515:897–904.
Martyn CN, Barker DJP, Jespersen S, Greenwald S, Osmond C, Berry C . Growth in utero, adult blood pressure, and arterial compliance. Br Heart J 1995;73:116–121.
Robinson JS, McMillen IC, Fielke S, Evans L, Lok F, Owens JA . Role of placenta: development and function. Equine Vet J 1998;30:456–457.
Louey S, Cock ML, Stevenson KM, Harding R . Placental insufficiency and fetal growth restriction lead to postnatal hypotension and altered postnatal growth in sheep. Pediatr Res 2000;48:808–814.
Acknowledgements
We would like to acknowledge Larry A. Sachs, PhD for his assistance with statistical analysis.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Cordero, L., Giannone, P., Ramirez, N. et al. Mean Arterial Pressure in Concordant and Discordant Triplets during the First Week of Life. J Perinatol 25, 198–204 (2005). https://doi.org/10.1038/sj.jp.7211232
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211232
This article is cited by
-
Early neonatal hypotension in premature infants born to preeclamptic mothers
Journal of Perinatology (2006)