Abstract
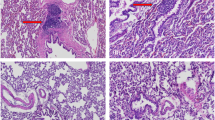
Bone marrow stromal cells isolated from a model of osteogenesis imperfecta (oim) mice, were transduced with a retrovirus (BAG) carrying the LacZ and neor genes after passage 21. The transduced cells retained the ability to express alkaline phosphatase activity in vitro when treated with recombinant human bone morphogenetic protein two (rhBMP-2), formed cartilage in vitro in aggregate cultures and formed bone in ceramic cubes after 6 weeks of implantation in nude mice. X-gal staining of ceramic cubes seeded with the transduced cells demonstrated the presence of LacZ-positive cells on the edges of bone and also in the lacunae of the newly formed bone 6 weeks after implantation. After infusion into femurs of oim mice, the transduced cells were detected in the marrow cavity and on the edges of the trabecular bone of the injected and contralateral femurs by X-gal staining and PCR analysis at 4, 10, 20, 30 and 40 days after injection. The LacZ gene was also detected in the lung and liver of the recipient mice at 4 and 10 days after injection but not at later time-periods. The present findings suggest that long-term cultured bone marrow stromal cells from osteogenesis imperfecta (OI) animals have the potential to traffic through the circulatory system, home to bone, form bone and continue to express exogenous genes. These findings open the possibility of using these cells as vehicles to deliver normal genes to bone as an alternative approach for the treatment of some forms of OI and certain other bone acquired and genetic diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Kuivaniemi H, Tromp GA, Prockop DL . Mutations in collagen genes: causes of rare and some common diseases in humans FASEB 1991 5: 2050–2052
Byers PH . Disorders of collagen biosynthesis and structure. In: Scriver CR, Beander AL, Sly WS, Valle D (eds). The Metabolic Basis of Inherited Disease, 6th edn McGraw-Hill: NY, pp 2805–2842
Prockop DJ . Mutations in collagen genes as a cause of connective tissue diseases New Engl J Med 1992 326: 540–546
Niyibizi C, Byers PH, Bonadio J, Eyre DR . Incorporation level of a mutant collagen α2(I) chain (Gly580-Asp) into bone matrix in a lethal case of osteogenesis imperfecta J Biol Chem 1992 25: 23108–23112
Byers PH, Pyritz RE, Uitto J . Research perspectives in heritable disorders of connective tissue Matrix 1992: 333–342
Shapiro JR, Chapman SD . Osteogenesis imperfecta. In: Kang A, Nimni ME (eds). Collagen, Vol. 5 Pathobiochemistry CRC Press: Boca Raton, pp 49–85
Pereira RF et al. Cultured adherent cells from marrow can serve as long-lasting precursor cells for bone, cartilage and lung in irradiated mice Proc Natl Acad Sci USA 1995 92: 4857–4861
Prockop DJ, Kiviriko KI . Collagens: molecular biology and potentials for therapy Ann Rev Biochem 1995 64: 403–434
Colige A et al. Use of antisense oligonucleotides to inhibit expression of mutated human procollagen gene (COL1A1(I)) in transfected mouse 3T3 cells Biochemistry 1993 32: 7–11
Laptev AV, Lu Z, Colige A, Prockop DJ . Specific inhibition of a human collagen gene (COL1A1(I) with modified antisense oligonucleotides. The most effective target sites are clustered in double stranded regions of the predicted secondly structure for mRNA Biochemistry 1994 33: 11033–11039
Wang Q, Marini JC . Antisense oligonucleotides selectively suppress expression of the mutant α2(I) collagen allele in type IV osteogenesis imperfecta fibroblasts J Clin Invest 1995 97: 448–454
Chipman SD et al. Defective proα2(I) collagen synthesis in a recessive mutation in mice: a model of human osteogenesis imperfecta Proc Natl Acad Sci USA 1993 90: 1701–1705
Crystal R . Transfer of genes to humans early lessons and obstacles to success Science 1995 270: 404–410
Evans CH, Robbins PD . Possible orthopaedic applications of gene therapy J Bone Joint Surg 1995 77A: 1103–1114
Friedenstein AJ, Chailakhjan RK, Lalykina KS . The development of fibroblasts colonies in monolayer cultures of guinea pig bone marrow and spleen cells Cell Tissue Kinet 1970 3: 393–403
Friedenstein AJ . Precursor cells of mechanocytes Int Rev Cytol 1976 47: 327–359
Benayahu D et al. Bone marrow-derived stromal cell line expressing osteoblastic phenotype in vitro and osteogenic capacity in vivo J Cell Physiol 1989 140: 1–7
Owen M . Marrow stromal cells J Cell Sci 1988 10: 63–76
Prockop DJ . Marrow stromal cells as stem cells for nonhematopoetic tissues Science 1997 276: 71–74
Caplan AI . Messenchymal stem cells J Orthop Res 1991 9: 641–650
Aubin JE, Turksen K, Heersche JNM . Osteoblastic lineage. In: Noda M. Cellular and Molecular Biology of Bone Academic Press: San Diego, 1993, pp 1–45
Beresford JN . Osteogenic stem cells and the stromal system Clin Orthopaedics Rel Res 1989 240: 270–279
Balk ML et al. Effect of rhBMP-2 on osteogenic potential of bone marrow stromal cells from an osteogenesis imperfecta (oim) mouse Bone 1977 21: 7–15
Kamalia N, McCulloch CAG, Tanebaum HC, Linback H . Dexamethasone recruitment of self-renewing osteoprogenitor cells in chick bone marrow stromal cell cultures Blood 1992 79: 320–326
Simmons DJ et al. Partial characterization of rat marrow stromal cells Calcif Tissue Int 1991 48: 326–334
Thies R et al. Recombinant human bone morphogenetic protein-2 induces osteoblastic differentiation in W-20-17 stromal cells Endorcinology 1992 130: 1318–1324
Vukicevic S, Luyten FP, Reddi AH . Stimulation of the expression of osteogenic and chondrogenic phenotypes in vitro by osteogenin 2 Proc Natl Acad Sci USA 1989 86: 8793–8797
Pitaru S, Kotev-Emeth S, Noff D, Savion N . Basic fibroblast growth factor (BFGF) enhances the capacity of rat bone stromal bone marrow cells to form mineralized bone-like tissue in culture. J Bone Miner Res 1990; 5 (Suppl 2) S78
Dennis JE, Caplan AI . Porous ceramic vehicles for rat marrow-derived osteogenic cell delivery: effects of pre-treatment with fibronectin or laminin J Oral Implantol 1993 19: 106–115
Allay J et al. LacZ and interleukin-3 expression in vivo after retroviral transduction of marrow derived human osteogenic mesenchymal progenitors Hum Gene Ther 1997 8: 1417–1427
Price J, Turner D, Cepko C . Lineage analysis in the vertebrate nervous system by retrovirus mediated gene transfer Proc Natl Acad Sci USA 1987 84: 156–160
Johnstone B et al. In vitro chondrogenesis of bone marrow derived mesenchymal progenitor cells Exp Cell Res 1998 238: 265–272
Kato Y et al. Terminal differentiation and calcification in rabbit chondrocyte cultures grown in centrifugre tubes: regulation by transforming growth factor β and serum factors Proc Natl Acad Sci USA 1988 85: 9552–9556
Ballock TR, Reddi AH . Thyroxine is the serum factor that regulates morphogenesis of columnar cartilage from isolated chondrocytes in chemically defined medium J Cell Biol 1994 126: 1311–1318
Cassiede P, Dennis J, Ma F, Caplan AI . Osteochondrogenic potential of marrow mesenchymal progenitor cells exposed to TGFβ1 or PDGF-BB as assayed in vivo and in vitro J Bone Miner Res 1996 11: 1264–1273
Sanes JR, Rubenstain JLT, Nicolas JF . Use of recombinant retrovirus to study post-implantation cell lineage in mouse embryos EMBO J 1986 5: 3133–3142
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Oyama, M., Tatlock, A., Fukuta, S. et al. Retrovirally transduced bone marrow stromal cells isolated from a mouse model of human osteogenesis imperfecta (oim) persist in bone and retain the ability to form cartilage and bone after extended passaging. Gene Ther 6, 321–329 (1999). https://doi.org/10.1038/sj.gt.3300839
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.gt.3300839
Keywords
This article is cited by
-
Animal models of osteogenesis imperfecta and related syndromes
Journal of Bone and Mineral Metabolism (2007)
-
Gene therapy approaches for osteogenesis imperfecta
Gene Therapy (2004)
-
Characterization of the distinct orthotopic bone-forming activity of 14 BMPs using recombinant adenovirus-mediated gene delivery
Gene Therapy (2004)
-
Hydroxyapatite ceramics as a carrier of gene-transduced bone marrow cells
Journal of Orthopaedic Science (2002)
-
Gene therapy for osteoporosis: evaluation in a murine ovariectomy model
Gene Therapy (2001)