Abstract
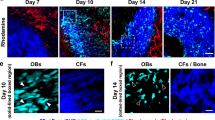
Nonviral gene delivery is a promising, safe, therapeutic tool in regenerative medicine. This study is the first to achieve nonviral, ultrasound-based, osteogenic gene delivery that leads to bone tissue formation, in vivo. We hypothesized that direct in vivo sonoporation of naked DNA encoding for the osteogenic gene, recombinant human bone morphogenetic protein-9 (rhBMP-9) would induce bone formation. A luciferase plasmid (Luc), encoding rhBMP-9 or empty pcDNA3 vector mixed with microbubbles, was injected into the thigh muscles of mice. After injection, noninvasive sonoporation was applied. Luc activity was monitored noninvasively, and quantitatively using bioluminescence imaging in vivo, and found for 14 days with a peak expression on day 7. To examine osteogenesis in vivo, rhBMP-9 plasmid was sonoporated into the thigh muscles of transgenic mice that express the Luc gene under the control of a human osteocalcin promoter. Following rhBMP-9 sonoporation, osteocalcin-dependent Luc expression lasted for 24 days and peaked on day 10. Bone tissue was formed in the site of rhBMP-9 delivery, as was shown by micro-computerized tomography and histology. The sonoporation method was also compared with previously developed electrotransfer-based gene delivery and was found significantly inferior in its efficiency of gene delivery. We conclude that ultrasound-mediated osteogenic gene delivery could serve as a therapeutic solution in conditions requiring bone tissue regeneration after further development that will increase the transfection efficiency.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Parker SE, Vahlsing HL, Serfilippi LM, Franklin CL, Doh SG, Gromkowski SH et al. Cancer gene therapy using plasmid DNA: safety evaluation in rodents and non-human primates. Hum Gene Ther 1995; 6: 575–590.
Burke B, Sumner S, Maitland N, Lewis CE . Macrophages in gene therapy: cellular delivery vehicles and in vivo targets. J Leukoc Biol 2002; 72: 417–428.
Hamm A, Krott N, Breibach I, Blindt R, Bosserhoff AK . Efficient transfection method for primary cells. Tissue Eng 2002; 8: 235–245.
Faurie C, Phez E, Golzio M, Vossen C, Lesbordes JC, Delteil C et al. Effect of electric field vectoriality on electrically mediated gene delivery in mammalian cells. Biochim Biophys Acta 2004; 1665: 92–100.
Cemazar M, Wilson I, Dachs GU, Tozer GM, Sersa G . Direct visualization of electroporation-assisted in vivo gene delivery to tumors using intravital microscopy—spatial and time dependent distribution. BMC Cancer 2004; 4: 81.
Ward M, Wu J, Chiu JF . Experimental study of the effects of Optison concentration on sonoporation in vitro. Ultrasound Med Biol 2000; 26: 1169–1175.
Lawrie A, Brisken AF, Francis SE, Cumberland DC, Crossman DC, Newman CM . Microbubble-enhanced ultrasound for vascular gene delivery. Gene Therapy 2000; 7: 2023–2027.
Duvshani-Eshet M, Adam D, Machluf M . The effects of albumin-coated microbubbles in DNA delivery mediated by therapeutic ultrasound. J Control Release 2006; 112: 156–166.
Duvshani-Eshet M, Machluf M . Efficient transfection of tumors facilitated by long-term therapeutic ultrasound in combination with contrast agent: from in vitro to in vivo setting. Cancer Gene Ther 2007; 14: 306–315.
Amabile PG, Waugh JM, Lewis TN, Elkins CJ, Janas W, Dake MD . High-efficiency endovascular gene delivery via therapeutic ultrasound. J Am Coll Cardiol 2001; 37: 1975–1980.
Chen S, Shohet RV, Bekeredjian R, Frenkel P, Grayburn PA . Optimization of ultrasound parameters for cardiac gene delivery of adenoviral or plasmid deoxyribonucleic acid by ultrasound-targeted microbubble destruction. J Am Coll Cardiol 2003; 42: 301–308.
Hashiya N, Aoki M, Tachibana K, Taniyama Y, Yamasaki K, Hiraoka K et al. Local delivery of E2F decoy oligodeoxynucleotides using ultrasound with microbubble agent (Optison) inhibits intimal hyperplasia after balloon injury in rat carotid artery model. Biochem Biophys Res Commun 2004; 317: 508–514.
Hauff P, Seemann S, Reszka R, Schultze-Mosgau M, Reinhardt M, Buzasi T et al. Evaluation of gas-filled microparticles and sonoporation as gene delivery system: feasibility study in rodent tumor models. Radiology 2005; 236: 572–578.
Lu QL, Liang HD, Partridge T, Blomley MJ . Microbubble ultrasound improves the efficiency of gene transduction in skeletal muscle in vivo with reduced tissue damage. Gene Therapy 2003; 10: 396–405.
Miao CH, Brayman AA, Loeb KR, Ye P, Zhou L, Mourad P et al. Ultrasound enhances gene delivery of human factor IX plasmid. Hum Gene Ther 2005; 16: 893–905.
Nakashima M, Tachibana K, Iohara K, Ito M, Ishikawa M, Akamine A . Induction of reparative dentin formation by ultrasound-mediated gene delivery of growth/differentiation factor 11. Hum Gene Ther 2003; 14: 591–597.
Taniyama Y, Tachibana K, Hiraoka K, Namba T, Yamasaki K, Hashiya N et al. Local delivery of plasmid DNA into rat carotid artery using ultrasound. Circulation 2002; 105: 1233–1239.
Tsutsui JM, Xie F, Porter RT . The use of microbubbles to target drug delivery. Cardiovasc Ultrasound 2004; 2: 23.
Miller DL, Quddus J . Sonoporation of monolayer cells by diagnostic ultrasound activation of contrast-agent gas bodies. Ultrasound Med Biol 2000; 26: 661–667.
Dijkmans PA, Juffermans LJ, Musters RJ, van Wamel A, ten Cate FJ, van Gilst W et al. Microbubbles and ultrasound: from diagnosis to therapy. Eur J Echocardiogr 2004; 5: 245–256.
Pislaru SV, Pislaru C, Kinnick RR, Singh R, Gulati R, Greenleaf JF et al. Optimization of ultrasound-mediated gene transfer: comparison of contrast agents and ultrasound modalities. Eur Heart J 2003; 24: 1690–1698.
Liang HD, Lu QL, Xue SA, Halliwell M, Kodama T, Cosgrove DO et al. Optimisation of ultrasound-mediated gene transfer (sonoporation) in skeletal muscle cells. Ultrasound Med Biol 2004; 30: 1523–1529.
Kodama T, Tan PH, Offiah I, Partridge T, Cook T, George AJ et al. Delivery of oligodeoxynucleotides into human saphenous veins and the adjunct effect of ultrasound and microbubbles. Ultrasound Med Biol 2005; 31: 1683–1691.
Gehl J . Electroporation: theory and methods, perspectives for drug delivery, gene therapy and research. Acta Physiol Scand 2003; 177: 437–447.
Golzio M, Teissie J, Rols MP . Cell synchronization effect on mammalian cell permeabilization and gene delivery by electric field. Biochim Biophys Acta 2002; 1563: 23–28.
Reddi AH . Role of morphogenetic proteins in skeletal tissue engineering and regeneration. Nat Biotechnol 1998; 16: 247–252.
Einhorn TA . Clinical applications of recombinant human BMPs: early experience and future development. J Bone Joint Surg Am 2003; 85-A (Suppl 3): 82–88.
Aslan H, Zilberman Y, Arbeli V, Sheyn D, Matan Y, Liebergall M et al. Nucleofection-based ex vivo nonviral gene delivery to human stem cells as a platform for tissue regeneration. Tissue Eng, accepted for publication (MS: TEN-05-0208.R1) 2006; 12: 877–889.
Cheng H, Jiang W, Phillips FM, Haydon RC, Peng Y, Zhou L et al. Osteogenic activity of the fourteen types of human bone morphogenetic proteins (BMPs). J Bone Joint Surg Am 2003; 85-A: 1544–1552.
Brown MA, Zhao Q, Baker KA, Naik C, Chen C, Pukac L et al. Crystal structure of BMP-9 and functional interactions with pro-region and receptors. J Biol Chem 2005; 280: 25111–25118.
Li JZ, Li H, Dunford B, Holman D, Beres B, Pittman DD et al. Rat strain differences in the ectopic osteogenic potential of recombinant human BMP adenoviruses. Mol Ther 2003; 8: 822–829.
Bekeredjian R, Grayburn PA, Shohet RV . Use of ultrasound contrast agents for gene or drug delivery in cardiovascular medicine. J Am Coll Cardiol 2005; 45: 329–335.
Pan H, Zhou Y, Izadnegahdar O, Cui J, Deng CX . Study of sonoporation dynamics affected by ultrasound duty cycle. Ultrasound Med Biol 2005; 31: 849–856.
Honigman A, Zeira E, Ohana P, Abramovitz R, Tavor E, Bar I et al. Imaging transgene expression in live animals. Mol Ther 2001; 4: 239–249.
Dayoub H, Dumont RJ, Li JZ, Dumont AS, Hankins GR, Kallmes DF et al. Human mesenchymal stem cells transduced with recombinant bone morphogenetic protein-9 adenovirus promote osteogenesis in rodents. Tissue Eng 2003; 9: 347–356.
Iris B, Zilberman Y, Zeira E, Galun E, Honigman A, Turgeman G et al. Molecular imaging of the skeleton: quantitative real-time bioluminescence monitoring gene expression in bone repair and development. J Bone Miner Res 2003; 18: 570–578.
Moutsatsos IK, Turgeman G, Zhou S, Kurkalli BG, Pelled G, Tzur L et al. Exogenously regulated stem cell-mediated gene therapy for bone regeneration. Mol Ther 2001; 3: 449–461.
Turgeman G, Pittman DD, Muller R, Kurkalli BG, Zhou S, Pelled G et al. Engineered human mesenchymal stem cells: a novel platform for skeletal cell mediated gene therapy. J Gene Med 2001; 3: 240–251.
Andre F, Mir LM . DNA electrotransfer: its principles and an updated review of its therapeutic applications. Gene Therapy 2004; 11 (Suppl 1): S33–S42.
Lefesvre P, Attema J, van Bekkum D . A comparison of efficacy and toxicity between electroporation and adenoviral gene transfer. BMC Mol Biol 2002; 3: 12.
Kishimoto KN, Watanabe Y, Nakamura H, Kokubun S . Ectopic bone formation by electroporatic transfer of bone morphogenetic protein-4 gene. Bone 2002; 31: 340–347.
Musgrave DS, Bosch P, Ghivizzani S, Robbins PD, Evans CH, Huard J . Adenovirus-mediated direct gene therapy with bone morphogenetic protein-2 produces bone. Bone 1999; 24: 541–547.
Betz OB, Betz VM, Nazarian A, Pilapil CG, Vrahas MS, Bouxsein ML et al. Direct percutaneous gene delivery to enhance healing of segmental bone defects. J Bone Joint Surg Am 2006; 88: 355–365.
Chakkalakal DA, Strates BS, Mashoof AA, Garvin KL, Novak JR, Fritz ED et al. Repair of segmental bone defects in the rat: an experimental model of human fracture healing. Bone 1999; 25: 321–332.
Clemens TL, Tang H, Maeda S, Kesterson RA, Demayo F, Pike JW et al. Analysis of osteocalcin expression in transgenic mice reveals a species difference in vitamin D regulation of mouse and human osteocalcin genes. J Bone Miner Res 1997; 12: 1570–1576.
Contag CH, Spilman SD, Contag PR, Oshiro M, Eames B, Dennery P et al. Visualizing gene expression in living mammals using a bioluminescent reporter. Photochem Photobiol 1997; 66: 523–531.
Lavon I, Goldberg I, Amit S, Landsman L, Jung S, Tsuberi BZ et al. High susceptibility to bacterial infection, but no liver dysfunction, in mice compromised for hepatocyte NF-kappaB activation. Nat Med 2000; 6: 573–577.
Ruegsegger P, Koller B, Muller R . A microtomographic system for the nondestructive evaluation of bone architecture. Calcif Tissue Int 1996; 58: 24–29.
Muller R, Ruegsegger P . Micro-tomographic imaging for the nondestructive evaluation of trabecular bone architecture. Stud Health Technol Inform 1997; 40: 61–79.
Balto K, Muller R, Carrington DC, Dobeck J, Stashenko P . Quantification of periapical bone destruction in mice by micro-computed tomography. J Dent Res 2000; 79: 35–40.
Muller R, Van Campenhout H, Van Damme B, Van Der Perre G, Dequeker J, Hildebrand T et al. Morphometric analysis of human bone biopsies: a quantitative structural comparison of histological sections and micro-computed tomography. Bone 1998; 23: 59–66.
Acknowledgements
We thank Rich-Mar Corp. (Inola) for kindly providing the sonoporation Sonitron2000 device for the experiments described in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sheyn, D., Kimelman-Bleich, N., Pelled, G. et al. Ultrasound-based nonviral gene delivery induces bone formation in vivo. Gene Ther 15, 257–266 (2008). https://doi.org/10.1038/sj.gt.3303070
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.gt.3303070
Keywords
This article is cited by
-
iPSC-neural crest derived cells embedded in 3D printable bio-ink promote cranial bone defect repair
Scientific Reports (2022)
-
Reprogrammed mesenchymal stem cells derived from iPSCs promote bone repair in steroid-associated osteonecrosis of the femoral head
Stem Cell Research & Therapy (2021)
-
Mesenchymal stem cells overexpressing BMP-9 by CRISPR-Cas9 present high in vitro osteogenic potential and enhance in vivo bone formation
Gene Therapy (2021)
-
Nonviral ultrasound-mediated gene delivery in small and large animal models
Nature Protocols (2019)
-
Inhibition of myostatin signal pathway may be involved in low-intensity pulsed ultrasound promoting bone healing
Journal of Medical Ultrasonics (2019)