Abstract
Aims
The aim of this study was to evaluate the motor, sensory, functional, and head posture results of recession of the lateral rectus muscle contralateral to the involved eye in patients with exotropic Duane retraction syndrome (DRS) type 3.
Methods
This was a retrospective, longitudinal, observational study of a consecutive clinical case series. Of the 11 patients with DRS type 3 operated on at a tertiary medical center from 1977 to 2012, 8 underwent recession of the lateral rectus muscle contralateral to the involved eye (with combined Y-splitting of ipsilateral lateral rectus muscle in 3 of them). Full ophthalmic, orthoptic, and neurological examination was performed before and after surgery. Main outcome measures included intragroup changes in motor misalignment, abnormal head turn, ocular upshoot, and stereopsis.
Results
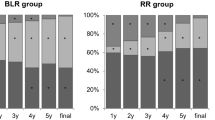
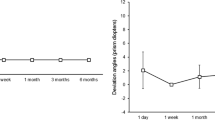
Mean patient age was 8.75±3.1 years at surgery. Mean exodeviation for distance was −17.3±3.5 prism diopters (PD) preoperatively and −4.0±6.1 PD postoperatively; corresponding values for near were −23.1±7.2 PD and −5.9±8.7 PD. Motor deviation improved by 77% for distance (P=0.017) and 74.5% for near (P=0.01). In 7/8 patients, the postoperative residual exodeviation (distance and near) was <8.0 PD. There was an 80% improvement in head turn, from 15.3±4° before surgery to 3.1±5.0° after (P=0.01). Stereopsis improved significantly in 6/8 patients. Findings remained stable during follow-up (mean duration 35.9±50.8 months, range 5–132 months).
Conclusions
Contralateral lateral rectus muscle recession appears to be a promising technique for the treatment of moderate unilateral DRS type 3, with patients showing significant motor and functional improvement and a decrease in head turn.
Similar content being viewed by others
Introduction
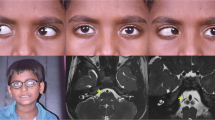
Duane retraction syndrome (DRS) is a spectrum of congenital ocular motility disorders characterized by limitation of horizontal duction associated with globe retraction1, 2, 3 and consequent narrowing of the palpebral fissure in adduction.4 DRS is caused by dysinnervation of the extraocular muscles (EOMs) by branches of the oculomotor nerve.5, 6 Huber7 classified DRS into three categories on the basis of electromyography examinations: type 1, limitation of abduction; type 2, limitation of adduction of the involved eye; and type 3, limitation of abduction and adduction of the involved eye. Co-contraction of the horizontal and/or vertical rectus muscle is typical to all three types.8 DRS type 3 is the second most common after DRS type 1, usually monocular, and mostly sporadic. It is characterized by exotropic or esotropic deviation or orthophoria because of the abnormal innervation of the lateral and medial rectus muscle by the ipsilateral oculomotor nerve.9, 10, 11
Traditionally, surgery for the treatment of exotropic DRS type 3 consists mainly of recession of the ipsilateral lateral rectus muscle to correct the horizontal misalignment.11, 12, 13, 14 However, the resulting primary position of the eye is unpredictable, with increasing lateral rectus limitation, and the visual field of single binocular vision may be reduced. An alternative surgical approach is recession of the lateral rectus muscle of the noninvolved (normal) eye in selected patients in order to better estimate the postoperative horizontal alignment. The aim of the present study was to evaluate the motor and sensory functional results of recession of the lateral rectus muscle contralateral to the affected eye in patients with exotropic DRS type 3.
Patients and methods
Design and patients
A retrospective study design was used. Patients were identified by a search of the electronic database of the Pediatric Ophthalmology Unit of Schneider Children’s Medical Center of Israel for all children treated for DRS type 3 from 1997 to 2012. Exclusion criteria were previous EOM or retinal detachment surgery, presence of an ocular malformation or neurological deficit, and <5 months of postoperative follow-up. The study was presented to the Institutional Review Board and was approved by the Ministry of Health and the hospital director.
Patient evaluation
Of the 31 patients with DRS who underwent EOM surgery at our unit during the study period, 11 had DRS type 3. All underwent full ophthalmic, orthoptic, and neurological evaluation before surgery, including cycloplegic refraction with 2 instillations (10 min apart) of cyclopentolate 1%. Distance (6 m) and near (0.33 m) deviations in the primary position were measured by the alternate prism cover test on an accommodative target in all diagnostic positions of gaze and in down gaze with normal head posture, and with the best optical correction, if necessary. Additional ocular upshoot and head turn (measured by goniometer) were evaluated as well, and binocular tests for fusion (Worth 4-dot test) and stereopsis (Titmus fly test) were conducted. The presence of a space-occupying lesion, myasthenia gravis, or intracranial vascular problem was ruled out. Duction limitation in the involved eye was identified by evaluating ocular motility toward the horizontal side, abduction and adduction, and nasal and temporal up/down positions, with comparison of the findings with the (normal) contralateral eye. Only patients with ocular abduction and adduction limitation of ≥−2 were classified as DRS type 3. Indications for surgery were horizontal distance and near vision misalignment of ≥10 prism diopters (PD) in the primary position, significant ocular upshoot, and abnormal head turn of >10°. A forced duction test in all directions was performed intraoperatively in all cases.
Surgical technique
All operations on the noninvolved eye were performed under general anesthesia by two surgeons (MS and NG-C). In patients with similar exotropia for distance and near, standard lateral rectus recession was performed in the uninvolved eye, as described by Parks.15 In patients with a significant difference between distance and near exodeviation, we used the slanted procedure wherein the upper and lower pole of the lateral rectus muscle was recessed nonsymmetrical from the original insertion, as described in detail by Snir et al.16 In the presence of moderate–severe upshoot, this procedure was combined with Y-split (bifurcation) of the lateral rectus muscle in the involved eye,17, 18 according to the guidelines of Rosenbaum and Santiago19 and Jampolsky.20, 21 The split ipsilateral lateral rectus muscle was recessed for 1.0 mm. The upper half was sutured to the adjacent upper corner of the original insertion and the lower half was sutured adjacent to the lower corner of the original insertion. The distance between the two halves at the suturing points was equal to the muscle width.
Outcome measures
Surgical and functional results were evaluated by repeating the presurgical examinations (including double Maddox rod test) on postoperative day 1, at 1, 3, and 6 months postoperatively, and periodically thereafter. Successful outcome was defined as a reduction in ocular horizontal (distance/near) deviation to ≤8 PD, alleviation of abnormal head tilt to ≤5°, and minimal to no ocular upshoot with regain of binocular functions (stereopsis) at the last ophthalmic examination.
Statistical analysis
The amount of slanted lateral muscle recession was measured by the midpoint distance between the recession points of the upper and lower pole of the muscle. To evaluate the impact on collapse of the angles of head turn and horizontal distance and near deviations, the mean postoperative measurements were deducted from the preoperative measurements divided by the lateral rectus muscle recession. The nonparametric Wilcoxon test was used to analyze the change in abnormal head tilt and in distance and near horizontal exodeviation and stereopsis from before to after surgery. The Mann–Whitney test was used to evaluate age at surgery and postoperative follow-up. A P-value of ≤0.05 was considered significant. All statistical calculations were performed with the SPSS program (Professional statistic release 11.5/2003, Chicago, IL, USA).
Results
Ages of the 11 patients with DRS type 3 ranged from 4 to 19 years. All were exotropic; none of the patients had orthotropia or esodeviation. Lateral rectus restriction was mild–moderate (+1) in 8 patients and moderate (+2/+3) in 3.
Of the 11 patients, 8 (73%) underwent recession of the lateral rectus muscle contralateral to the involved eye, and formed the study group. The other 3 patients were treated by the standard surgical approach (ipsilateral surgery of the involved eye).
The study group consisted of 5 boys (62.5%) and 3 girls of mean age 8.75±3.1 years at surgery (range, 4–14). The left eye was affected in 6 patients (75%) and the right eye in 2 patients. All patients were followed for ≥5 months postoperatively (mean 31±46.0 months, range 5–114 months).
Standard lateral rectus recession was performed in five patients and slanting recession procedures in three patients. The mean amount of lateral rectus muscle recession in the nondiseased eye was 6.95±1.2 mm (range, 6–9). Mean exodeviation for distance in primary gaze improved from −17.3±3.5 PD preoperatively (range, −14 to 25) to −4.0±6.1 PD (range, 0–18) postoperatively; corresponding values for near were −23.1±7.0 PD (range, −12 to 35) and −5.9±8.6 PD (range, 0–25). On statistical analysis, every 1.0 mm of lateral muscle recessed was associated with a 1.9 PD correction in exodeviation for distance and a 2.5 PD correction for near.
Four patients had ocular upshoot on adduction of the involved eye, of whom three underwent combined lateral rectus recession in the noninvolved eye and Y-split procedure on the lateral rectus muscle in the involved eye. None had ocular upshoot postoperatively. The remaining patient presented with flick ocular upshoot that resolved after horizontal EOM surgery in the noninvolved eye.
Gross stereopsis was present preoperatively in 4 patients (50%), with a range of 80 to 3000 s of arc, and in 7 patients (87.5%) postoperatively, with a range of 40 to 3000 s of arc (40 to 50 s of arc in 2 patients and 140 to 3000 s of arc in 5). Mean head turn measured 15.63±4.2° preoperatively (range 0–20) and 3.1±5.3° postoperatively (0–15). According to our calculations, every 1.0 mm recession of the lateral rectus muscle in the noninvolved eye corrected the head turn by a mean of 1.8°.
The patients who underwent ipsilateral lateral rectus surgery were not included in the study because of their small number (n=3) and one of them was lost to follow-up. In all three patients, results for all postoperative motoric and sensory parameters were unsatisfactory. Mean amount of lateral rectus recession in the involved eye measured 4.7±1.6 mm (range 4–9 mm). The difference in mean exodeviation for distance from before to after surgery did not achieve statistical significance (P=0.29); the same was true for the corresponding changes for near (P=0.1). One patient (1/3) had an ocular upshoot before and after surgery. None of the patients had stereopsis. Reoperation was recommended in 1/3 patients.
Overall, the postoperative evaluation of the study group yielded significant motor changes and improvement in alignment, with a 77% reduction in distance deviation (P=0.017) and a 74.5% reduction in near deviation (P=0.012) in primary gaze. In some patients, the horizontal deviation in side gaze was measured only preoperatively. However, none of the operated patients complained of diplopia on abduction of the noninvolved operated eye. In 7 of the 8 patients (87.5%), the postoperative residual exodeviation for distance and near was <8 PD; the remaining patient had hypertropia with residual exotropia of >8 PD. In addition, there was a significant (80%) improvement in head turn (P=0.01). Single binocular visual field examination was not performed because of technical problems. No torsional effect was found after surgery on double Maddox rod test. Reoperation was recommended in one patient.
Discussion
The surgical strategy for DRS type 3 poses a challenge as all three components of the disorder (horizontal deviation, head turn, and upshoot/downshoot) need to be taken into account on a case-by-case basis.22 The present study evaluated the outcome of patients with exotropic DRS type 3 treated by contralateral lateral rectus recession instead of the traditional ipsilateral lateral rectus muscle recession. Motor and functional results were good and remained stable throughout a follow-up period of ≥5 months. Specifically, distance/near exodeviation decreased to ≤8 PD in primary position, anomalous head turn decreased to ≤5°, eliminating the ocular upshoot, and stereopsis was regained. Together, these findings emphasize the advantages of this surgical technique.
Several surgical methods have been proposed in the ophthalmic literature to treat DRS,23, 24, 25, 26, 27 but most apply to types 1 and 2. Published results of DRS type 3 surgery are sparse in the medical literature, and the approaches used were not uniform. Most are also old. Using a tailored approach, Jampolsky21, 28 and others24, 25, 26 veered from the classification of Huber7 and considered the coexisting horizontal (either esotropia or exotropia) or vertical deviation; that is, they applied the surgical treatment intended for esotropic or exotropic DRS types 1 and 2 to DRS type 3 patients with esotropia or exotropia. In two case reports, Von Noorden29 and Sprunger30 recessed the ipsilateral medial and lateral rectus muscles simultaneously in a patient with DRS type 3 (with upshoot and downshoot), and Liu et al,31 in a study of 16 patients with DRS, 13 patients with type 3 (esotropic and exotropic), recessed both horizontal rectus muscles, with good results in primary position in all patients. Spielmann et al32 also reported good results with a posterior fixation suture of the horizontal rectus muscles of the sound eye. These procedures were based on the rationale of transposing the insertion of these muscles posteriorly in relation to the center of rotation of the globe.
Owing to the severe paradoxical EOM innervation in the involved eye in DRS type 3, operating on the ipsilateral lateral rectus muscle poses a risk of increasing the abduction limitation and incomitant deviation, with unpredictable results. Furthermore, it is difficult to sufficiently weaken the lateral rectus muscle surgically and it increases esotropia in lateral gaze.21, 28 However, when recession is performed on the lateral rectus muscle in the contralateral eye, with normal EOM innervation, the postoperative alignment is more predictable. This procedure also increases the tone in the contralateral normally innervated medial rectus muscle. Surgery is planned according to the misalignment of the secondary deviation.
Several authors agree with the notion of operating on the noninvolved eye to improve alignment results.33, 34, 35 Lingua and Walonker35 suggested operating on the noninvolved eye when the weakened EOM retains enough strength to rotate the eye into its field of action. Recession of either the yoke muscle of the paretic muscle or the yoke’s antagonist exerts the greatest effect in the primary direction of gaze, where it is needed. Archer33, 34 suggested that recession of the contralateral (noninvolved) eye decreased both the innervation of the normal operated eye and the aberrant innervation to the EOM in the involved eye.
According to Saunders et al,36 two conditions are necessary to achieve good results with surgery on the contralateral agonist EOM of the involved DRS muscle. First, very large recessions or posterior fixation sutures (Faden procedure) are used in the noninvolved eye to cause comparable duction limitations as in the affected eye. By matching the movement abnormalities of the eye with DRS, alignment can be restored in the primary position, with the creation of a wider diplopia-free field (and improved single binocular vision) postoperatively. Second, as the normal eye is usually the dominant one, this technique should be done only in patients with moderate-angle deviation.
The rationale for contralateral rectus muscle recession in DRS type 3 may be clarified by the study of Lingua and Walonker35 in patients with DRS type 1. These authors found that by using both recession and posterior fixation of the normal medial rectus muscle, they eliminated the abnormal head position and corrected moderate-angle esotropia (up to 40 PD). Similarly, in a discussion of the study results of Saunders et al,36 Kraft37 recommended that this technique be applied on the normal EOM only for esotropia of at least 20 PD (in DRS type 1).
Upshoot and downshoot are more common in DRS type 3 than in types 1 and 2.38 In the present study, half the patients had an upshoot of the affected eye on adduction. In three of these patients, we combined a splitting procedure of the lateral rectus muscle on the involved side in the same session that successfully eliminated the disfiguration in all cases. This approach was based on the rationale, as advocated by Jampolsky,20, 21 that repositioning each half of the ipsilateral lateral rectus muscle could stabilize the globe and prevent its slippage above or below the horizontal plane. It may add a weakening impact or reduce the residual postoperative exodeviation. Others reported that this combined technique in the involved eye led to dramatic improvement in patients with moderate globe retraction on adduction.17, 18, 39, 40, 41
It is noteworthy that our cohort was considerably older (8.75±3.13 years) than in most other common strabismus studies. Kubota et al23 reported that 92.7% of their patients with DRS underwent surgery after age 3 years, and Waddell et al9 suggested that surgery for DRS should be performed before age 8 years. However, although DRS is diagnosed early, the indications for surgery may develop only later in life.
Sloper and Collins8 and Chua et al12 reported the absence of binocular vision in 20% of their patients. Evaluation of the postoperative functional/sensory results in our study showed that 6 of the 8 patients (75%) had improved binocular function (stereopsis) compared with preoperative ranges. It is noteworthy that the improved motoric results were combined with better functional outcomes that helped to stabilize the ocular alignment during the follow-up period. Surgical treatment for DRS in the literature appears to focus more on the motor than the sensory aspect. However, both features are important in visual rehabilitation, especially in patients with complicated DRS type 3.
Our study is limited by the retrospective design and lack of a control group. The small cohort was because of the rarity of DRS type 3: in the past 15 years, we operated on a total of only 11 patients, of whom 8 were treated with the new approach. Furthermore, the changes in horizontal deviation in side gazes from before to after surgery were not calculated and the field of single binocular vision was not measured.
In conclusion, the present study shows that in a selected group of patients with unilateral moderate exotropic DRS type 3, lateral rectus muscle recession in the noninvolved eye has several important advantages. It reduces the mean distance/near exodeviation (to ≤8 PD in our cohort), minimizes the head turn (to ≤5° in our cohort), and eliminates the disfiguring upshoot position (when combined with ipsilateral Y-split). In addition, most of the patients regained stereopsis. The motor, functional, and head posture improvements remain stable during follow-up. At present, this technique is preferred at our center to correct moderate-angle exodeviation in DRS type 3 with anomalous head turn. Further collaborative multicenter studies in larger cohorts are needed to corroborate these findings.

References
Duane A . Congenital deficiency of abduction, associated with impairment of adduction, retraction movements, contraction of the palpebral fissure and oblique movements of the eye. Arch Ophthalmol 1905; 14: 133–159.
Altintas AG, Arifoglu HB, Arikan M, Simsek S . Clinical findings and surgical results of Duane retraction syndrome. J Pediatr Ophthalmol Strabismus 2010; 47: 220–226.
De Respinis PA, Caputo AR, Wagner RS, Guo S . Duane’s retraction syndrome. Surv Ophthalmol 1993; 38: 257–288.
Freedman HL, Kushner BJ . Congenital ocular aberrant innervation – new concepts. J Pediatr Ophthalmol Strabismus 1997; 34: 10–16.
Parsa CF, Grant E, Dillon WP Jr, du Lac S, Hoyt WF . Absence of the abducens nerve in Duane syndrome verified by magnetic resonance imaging. Am J Ophthalmol 1998; 125: 399–401.
Scott AB, Wong GY . Duane’s syndrome. An electromyographic study. Arch Ophthalmol 1972; 87: 140–147.
Huber A . Electrophysiology of the retraction syndrome. Br J Ophthalmol 1974; 58: 293–300.
Sloper JS, Collins AD . Effects of Duane’s retraction syndrome on sensory visual development. Strabismus 1999; 7: 25–36.
Waddell EM . Duane’s retraction syndrome reconsidered. Br Orthoptic J 1980; 37: 56–65.
Isolated Duane retraction syndrome. Genetics Home Reference. March 2009. At http://ghr.nlm.nih.gov/condition/isolated-duane-retraction-syndrome. Accessed 18 November 2011.
Barbe ME, Scott WE, Kutschke PJ . A simplified approach to the treatment of Duane’s syndrome. Br J Ophthalmol 2004; 88: 131–138.
Chua B, Johnson K, Donaldson C, Martin F . Management of Duane retraction syndrome. J Pediatr Ophthalmol Strabismus 2005; 42: 13–17.
Natan K, Traboulsi EI . Unilateral rectus muscle recession in the treatment of Duane syndrome. J AAPOS 2012; 16: 145–149.
Pressman SH, Scott WE . Surgical treatment of Duane’s syndrome. Ophthalmology 1986; 93: 29–38.
Parks MM . Ocular Motility and Strabismus. Harper & Row: Hagerstown, MD, 1975.
Snir M, Axer-Siegel R, Shalev B, Sherf I, Yassur Y . Slanted lateral rectus recession for exotropia with convergence weakness. Ophthalmology 1999; 10: 992–996.
Das JC, Chaudhuri Z, Bhomaj S, Sharma P . Lateral rectus split in the management of Duane’s Retraction Syndrome. Ophthalmic Surg Lasers 2000; 31: 499–501.
Rao VB, Helveston EM, Sahare P . Treatment of upshoot and downshoot in Duane syndrome by recession and Y-splitting of the lateral rectus muscle. J AAPOS 2003; 7: 389–395.
Rosenbaum AL, Santiago AP . Clinical Strabismus Management. Principles and Surgical Techniques. WB Saunders, St Louis 1999.
Jampolsky A . Surgical leashes and reverse leashes in strabismus surgical management. In: Helveston EM (ed) Symposium on Strabismus: Transactions of the New Orleans Academy of Ophthalmology. CV Mosby: St Louis, MO, 1978 pp 244–268.
Jampolsky A . Strategies in strabismus surgery. In: Crawford IC, Flynn IT, Haik BG, Helveston EM, Hayt CS, Jampolsky A et al (eds). Pediatric Ophthalmology and Strabismus: Transactions of the New Orleans Academy of Ophthalmology. Raven Press: New York, 1985 pp 363–368.
Kraft SP . A surgical approach for Duane syndrome. J Pediatr Ophthalmol Strabismus 1988; 25: 119–130.
Kubota N, Takahashi H, Hayashi T, Sakaue T, Maruo T . Outcome of surgery in 124 cases of Duane’s retraction syndrome (DRS) treated by intraoperatively graduated recession of the medial rectus for esotropic DRS, and of the lateral rectus for exotropic DRS. Binocul Vis Strabismus Q 2001; 16: 15–22.
Souza-Dias C . Recession of both horizontal recti muscles in Duane’s retraction syndrome with elevation and depression of the adducted eye. Am J Ophthalmol 1993; 115: 685–686.
Puerto-Hernández B, López-Caballero C, Rodríguez-Sánchez JM, González-Manrique M, Contreras I . [Surgical treatment of Duane’s syndrome type I by recession of the medial rectus of the affected eye and faden operation of the contralateral medial rectus]. [Article in Spanish] Arch Soc Esp Oftalmol 2008; 83: 113–116.
Farvardin M, Rad AH, Ashrafzadeh A . Results of bilateral medial rectus muscle recession in unilateral esotropic Duane syndrome. J AAPOS 2009; 13: 339–342.
Nelson LB . Severe adduction deficiency following a large medial rectus recession in Duane’s retraction syndrome. Arch Ophthalmol 1986; 104: 859–862.
Jampolsky A . When is supermaximal surgery safe? Am Orthopt J 1987; 37: 33–44.
Von Noorden GK . Recession of both horizontal recti muscles in Duane’s retraction syndrome with elevation and depression of the adducted eye. Am J Ophthalmol 1992; 114: 311–313.
Sprunger DT . Recession of both horizontal rectus muscles in Duane syndrome with globe retraction in primary position. J AAPOS 1997; 1: 31–33.
Liu MM, Zhao KX, Zhang W, Guo X, Zhu LN, Ma HZ et al. [Recession of both horizontal rectus muscles in Duane Retraction Syndrome with significant globe retraction]. [Article in Chinese] Zhonghua Yan Ke Za Zhi 2012; 48: 776–780.
Spielmann A, Lagrange B, Laurent M . Le syndrome de retraction de Stilling Duane. Etiopathogénie clinique. Regulation motrice par la Faden-operation de Cüppers sur l’oeil sain, associé ou non a la chirurgie de l’oeil atteint. J Fr Orthop 1976; 8: 105–107.
Archer SM . Contralateral medial rectus muscle recession in patients with Duane syndrome. J AAPOS 2004; 8: 296 author reply 296.
Archer SM . Results of bilateral medial rectus muscle recession in unilateral esotropic Duane syndrome. J AAPOS 2010; 14: 103–104 author reply 104-5.
Lingua RW, Walonker F . Use of the posterior fixation suture in type I Duane’s syndrome. J Ocul Ther Surg 1985; 4: 107–111.
Saunders RA, Wilson ME, Bluestein EC, Sinatra RB . Surgery on the normal eye in Duane retraction syndrome. J Pediatr Ophthalmol Strabismus 1994; 31: 162–169.
Kraft SP . Surgery on the normal eye in Duane retraction syndrome: Discussion. J Pediatr Ophthalmol Strabismus 1994; 31: 170–171.
Mohan K, Saroha V . Vertical rectus recession for the innervational upshoot and downshoot in Duane’s retraction syndrome. J Pediatr Ophthalmol Strabismus 2002; 39: 94–99.
Britt MT, Velez FG, Thacker N, Alcorn D, Foster RS, Rosenbaum AL . Surgical management of severe cocontraction, globe retraction, and pseudo-ptosis in Duane syndrome. J AAPOS 2004; 8: 362–367.
Ohtsuki H, Hasebe S, Tadokoro Y, Kishimoto N, Watanabe S, Okano M . Synoptometer analysis of vertical shoot in Duane’s retraction syndrome. Ophthalmologica 1992; 204: 82–87.
Von Noorden GK, Murray E . Up- and downshoot in Duane’s retraction syndrome. J Pediatr Ophthalmol Strabismus 1986; 23: 121–123.
Acknowledgements
We thank Dorit Karesh for the statistical analysis and Gloria Ginzach for her editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Snir, M., Dotan, A., Friling, R. et al. Contralateral lateral rectus muscle recession in patients with Duane retraction syndrome type 3. Eye 28, 279–284 (2014). https://doi.org/10.1038/eye.2013.260
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2013.260