Abstract
Purpose
To evaluate the correlation of subretinal fluid volume with choroidal thickness and macular volume in acute central serous chorioretinopathy (CSC).
Methods
Twenty patients with acute unilateral treatment-naive idiopathic CSC and 20 age-matched normal eyes were included in this prospective cross-sectional study. Subretinal fluid volume (SRFV) of study eyes was estimated using a built-in segmentation-modifying tool of Spectralis spectral-domain optic coherence tomography (SD-OCT). Subfoveal choroidal thickness (SCT) (measured with enhanced depth imaging-OCT) and macular volume (MV) were also determined. The correlation of SRFV with SCT and MV was analyzed statistically.
Results
There was no significant correlation of SRFV with SCT and MV in the study eyes (r=0.062, P=0.796 and r= −0.061, P=0.798, respectively). The mean SCT of the study eyes, the fellow eyes and the control eyes were 461.4±101.4, 375.3±103.7, 287.6±62.5 μm, respectively (P<0.001). The mean modified MV (determined excluding SRF volume) of the study eyes, the macular volume of the fellow and the control eyes was 8.57±0.59 mm3, 8.75±0.4 mm3 and 8.73±0.38 mm3, respectively (P>0.05).
Conclusions
The current study shows that subretinal fluid volume does not correlate with subfoveal choroidal thickness. This novel finding suggests that formation of subretinal fluid is not solely associated with choroidal vasculature in acute CSC.
Similar content being viewed by others
Introduction
Central serous chorioretinopathy (CSC) is a disorder characterized by serous retinal detachment and/or retinal pigment epithelial detachment (RPE), changes most often confined to the macula, and associated with leakage of fluid through the RPE into the subretinal space.1 Two theories in the pathogenesis of CSC have been proposed: one is choroidal dysfunction and the other is RPE dysfunction theory.2 Although the evidence for a choroidal vasculopathy in CSC is strong, the underlying mechanism of choroidal disease remains to be determined.
The availability of optical coherence tomography (OCT) has vastly enhanced the anatomical assessment and understanding of CSC by providing cross-sectional imaging of the macula and the presence of subretinal fluid. Recent advances in choroidal imaging with OCT, coupled with the enhanced depth imaging (EDI) technique,3 have revealed choroidal thickening in eyes with CSC, and such thickening decreased after the treatment with photodynamic therapy.1 Furthermore, various morphological features of CSC have been reported with OCT evaluation. The thickness of the outer nuclear layer, as measured with SD-OCT, appears to correlate with acuity in CSC.4 OCT suggests that photoreceptor outer segments elongate in eyes with active serous detachment5 and foveal thickness at presentation and after resolution of subretinal fluid (SRF) appear to correlate with acuity outcomes.6 In one study, three-dimensional (3D) configuration of SRF was characterized in CSC using spectral-domain (SD) OCT and the 3D configurations were found to be different between acute and chronic CSC.7
Choroidal vascular hyperpermeability on ICGA is associated with an increase in subfoveal choroidal thickness on OCT.1 Moreover, one study showed increase in choroidal thickness after administration of a selective inhibitor of cyclic guanosine monophosphate-specific phosphodiesterase-5, which acts as a vasodilator.8 Another study reported that choroidal thickness in patients with CSC decreased after photodynamic therapy, which targeted choroidal vasculature.9 In addition, the mean choroidal thicknesses of the affected eyes were found to be significantly greater than those of the unaffected fellow eyes in patients with unilaterally active CSC.10 All these studies suggest that change in choroidal thickness may reflect the choroidal vasculature. On the other hand, in several hypotheses, hyperpermeable choroidal vasculature has been regarded as a strong candidate for the origin of SRF.1 As a general rule, transport of fluid can be driven by hydrostatic pressure gradients. Thus, hyperpermeable choroidal vasculature is thought to produce increased tissue hydrostatic pressure, and leads to fluid accumulation between the retina and the RPE.1 On the basis of all the aforementioned data, thicker choroid would be expected to cause the formation of more SRF.
However, to the best of our knowledge, there has been no report thus far on the association of SRF volume that can be estimated using a built-in segmentation-modifying tool of SD-OCT11 and choroidal thickness of the patients suffering from acute CSC. Thus, the principle objective of this study was to evaluate the correlation between these two parameters. The effect of SRF volume on macular volume was investigated, as well.
Materials and methods
Twenty patients with acute, unilateral treatment-naive idiopathic CSC were included in this prospective cross-sectional study that was conducted at Retina Division, Ophthalmology Department of Kayseri Training and Research Hospital over a 12-month period. In addition, 20 healthy volunteers were included in the study as a control group.
The study followed the tenets of the Declaration of Helsinki and approved by local ethical committee. Each participant provided informed consent.
Inclusion criteria were diagnosis of idiopathic CSC with symptom duration of less than 1 month and presence of subretinal fluid involving the macula associated with idiopathic leaks or mottling during fluorescein angiography (FA). Exclusion criteria were any prior treatment (such as laser photocoagulation, photodynamic therapy, or intravitreal injections of anti-VEGF), any presence of subretinal fluid or retinal pigment epithelium detachment in the fellow eyes at presentation and presence of subretinal fluid due to causes other than CSC (such as polypoidal choroidal vasculopathy).
Each patient underwent ophthalmologic examination, color fundus photography, fluorescein angiography (FA), and Spectralis spectral-domain OCT (Heidelberg Engineering Inc., Heidelberg, Germany). All OCT measurements were performed within a limited time (0900 to 1200 hours), which minimized the possibility of choroidal thickness change caused by diurnal variations.
For measurements of subfoveal choroidal thickness, 9 mm horizontal sections, which contained 100 duplicated scans, of the macula going through the foveola were obtained by the EDI-OCT maneuver previously described by Spaide et al.3 Subfoveal choroidal thickness was manually measured using the contained Heidelberg eye explorer software (version 1.5.12.0, Heidelberg Engineering Inc.). Choroidal thickness was defined as the vertical distance from the hyperreflective line of Bruch’s membrane to the innermost hyperreflective line of the chorio-scleral interface which was clearly visible in all eyes. Subfoveal choroidal thickness from the horizontal section was analyzed (Figure 1).
SRF volume was estimated using a built-in segmentation-modifying tool of SD-OCT.11 Segmentation lines for internal limiting membrane and RPE were determined automatically for each of the volume scans, and the total macular volume of nine macular sectors as defined by the Early Diabetic Retinopathy Study was provided (Figure 2). The density of the macular volume scan was determined as 25 scans spaced 240 μm apart. Using the modifying tool, the cursor line on the RPE was moved to the tips of the outer segments of the photoreceptors (Figure 3). The cursor lines were moved in all cuts so that the macular volume calculation could be accurately recalculated. If there was any pigment epithelial detachment, RPE line was moved to take that into account. With this movement, the modified macular volume was determined excluding SRF and was used as macular volume in the study eyes. The SRF volume was then calculated by subtracting this modified macular volume from the total macular volume.
SRF volume was estimated using a built-in segmentation-modifying tool of SDOCT. Segmentation lines for internal limiting membrane and RPE were determined automatically for each of the volume scans, and the total macular volume of nine macular sectors as defined by the Early Diabetic Retinopathy Study was provided.
Using the modifying tool, the cursor line on the RPE was moved to the tips of the outer segments of the photoreceptors. With this movement, the modified macular volume was determined excluding SRF and was used as macular volume in the study eyes. The SRF volume was then calculated by subtracting this modified macular volume from the total macular volume.
The distributions of all variables determined with Shapiro–Wilk test were normal. The parameters were presented as mean±standard deviation. The analysis of variance (one-way ANOVA) was used to evaluate the statistical significance over choroidal thickness and macular volume. All comparisons between the study eyes, the fellow eyes, and the control eyes were applied using Tukey post hoc correction. Pearson’s correlation coefficient was calculated to examine associations between choroidal thickness and SRF volume in the study eyes. All statistical analyses were performed using SPSS Version 13.0 statistical analysis software (SPSS Inc., Chicago, IL, USA) and P-values <0.05 were considered statistically significant.
Results
The study included 20 patients with a mean age of 41.2±7.2 (27–54) years and 12 patients were male. The mean age of the control group (13 male, 7 female) was 39.3±6.9 (25–48) years (P>0.05). The mean symptom duration was 18±6 (7–30) days. The mean decimal visual acuity was 0.51±0.13 (0.3–0.7). The FA leakage patterns were: inkblot (55%), mottled pattern (40%) and smokestack (5%).
The mean OCT parameters of the study eyes, fellow eyes, and control eyes were shown in Table 1.
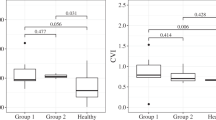
The mean subfoveal choroidal thicknesses of the study eyes, the fellow eyes, and the control eyes were 461.4±101.4, 375.3±103.7, 287.6±62.5 μm, respectively. The mean choroidal thicknesses of the study eyes were significantly greater than those of the fellow eyes and the control eyes (P<0.001). Also, the mean choroidal thicknesses of the fellow eyes were significantly greater than those of the control eyes (P<0.001).
The mean modified macular volume (determined excluding SRF volume) of the study eyes was 8.57±0.59 mm3. The macular volume of the fellow eyes and the control eyes were 8.75±0.43 and 8.73±0.38 mm3, respectively. However, the differences did not reach a statistical significance (P>0.05).
Pearson correlation analysis revealed no significant correlation of choroidal thickness with SRF volume in the study eyes (r=0.062 and P=0.796; Figure 4a). There was no significant correlation between macular volume and SRF volume in the study eyes (r= −0.061 and P=0.798; Figure 4b).
Discussion
The results of this study revealed that choroidal thickness was significantly increased in the affected eyes compared with unaffected fellow eyes of unilaterally active CSC patients and control eyes, confirming previous reports.10, 12, 13 To our knowledge, the unique aspect of the current study is the measurement of subretinal fluid volume and its correlation with subfoveal choroidal thickness and macular volume. The analysis showed that SRF volume does not correlate with subfoveal choroidal thickness and macular volume.
The mean subfoveal choroidal thicknesses of the study eyes, the fellow eyes, and the control eyes were 461.4±101.4, 375.3±103.7, 287.6±62.5 μm, respectively The differences were statistically significant. The pathogenesis of CSC is still partly controversial; however, its mechanism has been postulated to be hyperpermeability of the choroidal vessels and consequent increased choroidal hydrostatic pressure.1 This also was confirmed by a series of ICGA study,14 in which CSC was augmented by hyperfluorescein leakage from the choriocapillaris or large vessels. These facts led to the expectation that the choroid might become thickened in CSC, and the current study confirmed this using EDI-OCT and consistent with previous studies.10, 12, 13
However, it remains unclear as to whether or not thicker choroid on OCT is associated with larger SRF volume. If this is indeed the case, the assessment of choroidal thickness may prove to be a useful clinical indicator for the monitoring of SRF volume. To analyze this, the correlation of SRF volume and subfoveal choroidal thickness was investigated in the current study. But, no association was found between these two parameters. This novel finding suggests that formation of subretinal fluid is not solely associated with choroidal vasculature. Some factors such as RPE dysfunction other than choroidal disease may have a role in the pathogenesis of CSC. However, these data need to be clarified by further studies.
Macular volume analysis revealed that there was no significant difference between the affected, the unaffected eyes, and the control eyes. The mean modified macular volume (determined excluding SRF volume) of the study eyes was 8.57±0.59 mm3. The macular volume of the fellow eyes and the control eyes were 8.75±0.43 and 8.73±0.38 mm3, respectively. The differences were not statistically significant. On the other hand, Matsumoto et al5 showed that the median distance between the internal limiting membrane (ILM) and the external limiting membrane (ELM) at the central fovea was approximately 135 μm (range, 115 to 175 μm) in the 10 normal eyes. In the 20 eyes with CSC, the median distance was approximately 75 μm (range, 60 to 130 μm) at the central fovea, where the retina was always detached. In short, the distance between the ILM and the ELM was found to be significantly shorter in eyes with CSC than in normal eyes.5 Although there seems to be inconsistency between the current study and the study done Matsumoto et al, symptom duration was shorter in the current study (18 days vs 3.5 months). For this reason, there would not be enough time for the apoptosis of the photoreceptors occurs in the detached retina.
One limitation of this study was small sample size. The reason for this, unilateral treatment-naive idiopathic CSC patients with symptom duration of <1 month were chosen. Another limitation was manual measurement of subfoveal choroidal thickness. However, authors found high interobserver correlation,3 high repeatability,15 and high intersystem, interexaminer, and intervisit reproducibility16 in choroidal thickness measurements. Finally, our study cannot answer the question of cause–effect relationship. In other words, we cannot definitively conclude that subretinal fluid volume does not go parallel to subfoveal choroidal thickness in CSC. Therefore, randomized-controlled studies are needed to further explain this issue.
In conclusion, the current study shows that subretinal fluid volume does not correlate with subfoveal choroidal thickness. This novel finding suggests that formation of subretinal fluid is not solely associated with choroidal vasculature in acute CSC.

References
Nicholson B, Noble J, Forooghian F, Meyerle C . Central serous chorioretinopathy: update on pathophysiology and treatment. Surv Ophthalmol 2013; 58 (2): 103–126.
Gemenetzi M, De Salvo G, Lotery AJ . Central serous chorioretinopathy: an update on pathogenesis and treatment. Eye 2010; 24 (12): 1743–1756.
Spaide RF, Koizumi H, Pozzoni MC . Enhanced depth imaging spectral-domain optical coherence tomography. Am J Ophthalmol 2008; 146 (4): 496–500.
Matsumoto H, Sato T, Kishi S . Outer nuclear layer thickness at the fovea determines visual outcomes in resolved central serous chorioretinopathy. Am J Ophthalmol 2009; 148 (1): 105–110.
Matsumoto H, Kishi S, Otani T, Sato T . Elongation of photoreceptor outer segment in central serous chorioretinopathy. Am J Ophthalmol 2008; 145 (1): 162–168.
Furuta M, Iida T, Kishi S . Foveal thickness can predict visual outcome in patients with persistent central serous chorioretinopathy. Ophthalmologica 2009; 223 (1): 28–31.
Ahn SE, Oh J, Oh JH, Oh IK, Kim SW, Huh K . Three-dimensional configuration of subretinal fluid in central serous chorioretinopathy. Invest Ophthalmol Vis Sci 2013; 54 (9): 5944–5952.
Vance SK, Imamura Y, Freund KB . The effects of sildenafil citrate on choroidal thickness as determined by enhanced depth imaging optical coherence tomography. Retina 2011; 31 (2): 332–335.
Maruko I, Iida T, Sugano Y, Ojima A, Ogasawara M, Spaide RF . Subfoveal choroidal thickness after treatment of central serous chorioretinopathy. Ophthalmology 2010; 117 (9): 1792–1799.
Kim YT, Kang SW, Bai KH . Choroidal thickness in both eyes of patients with unilaterally active central serous chorioretinopathy. Eye 2011; 25 (12): 1635–1640.
Shin JW, Shin YU, Lee BR . Choroidal thickness and volume mapping by a six radial scan protocol on spectral-domain optical coherence tomography. Ophthalmology 2012; 119 (5): 1017–1023.
Imamura Y, Fujiwara T, Margolis R, Spaide RF . Enhanced depth imaging optical coherence tomography of the choroid in central serous chorioretinopathy. Retina 2009; 29 (10): 1469–1473.
Jirarattanasopa P, Ooto S, Tsujikawa A, Yamashiro K, Hangai M, Hirata M et al. Assessment of macular choroidal thickness by optical coherence tomography and angiographic changes in central serous chorioretinopathy. Ophthalmology 2012; 119 (8): 1666–1678.
Piccolino FC, Borgia L . Central serous chorioretinopathy and indocyanine green angiography. Retina 1994; 14 (3): 231–242.
Rahman W, Chen FK, Yeoh J, Patel P, Tufail A, Da Cruz L . Repeatability of manual subfoveal choroidal thickness measurements in healthy subjects using the technique of enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci 2011; 52 (5): 2267–2271.
Ikuno Y, Maruko I, Yasuno Y, Miura M, Sekiryu T, Nishida K et al. Reproducibility of retinal and choroidal thickness measurements in enhanced depth imaging and highpenetration optical coherence tomography. Invest Ophthalmol Vis Sci 2011; 52 (8): 5536–5540.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Rights and permissions
About this article
Cite this article
Goktas, A. Correlation of subretinal fluid volume with choroidal thickness and macular volume in acute central serous chorioretinopathy. Eye 28, 1431–1436 (2014). https://doi.org/10.1038/eye.2014.219
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2014.219
This article is cited by
-
Choroidal modifications assessed by means of choroidal vascularity index after oral eplerenone treatment in chronic central serous chorioretinopathy
Eye (2023)
-
Sensitivity and specificity of choroidal thickness measurement by EDI-OCT for central serous chorioretinopathy diagnosis
International Ophthalmology (2021)
-
Multimodal retinal imaging in central serous chorioretinopathy treated with oral eplerenone or photodynamic therapy
Eye (2018)
-
Macular ganglion cell complex thickness in acute and chronic central serous chorioretinopathy
International Ophthalmology (2017)