Abstract
Objectives
To evaluate the significance of the largest tumour diameter (LTD) of posterior uveal melanomas (ie, involving choroid), correlating this feature with histological and cytogenetic predictors and mortality.
Methods
Patients with posterior uveal melanoma were included. LTD was measured by echography and correlated with histological and cytogenetic findings and metastatic death.
Results
The cohort comprised 1776 patients with a median age of 60 years, a median tumour diameter of 14.0 mm, and a median tumour height of 7.5 mm. The LTD was greater in older patients (t-test, P<0.001). The presence of epithelioid cells, closed loops, high mitotic rate, chromosome 3 deletion, and chromosome 8 gains all correlated significantly with LTD (t-test, P<0.001). The 1521 British patients had a median follow-up of 4.9 years, with a disease-specific mortality of 28.9%. Metastatic death correlated with LTD (Cox multivariate analysis, P<0.001). Tumours with the same LTD showed significant variation in survival, according to the presence of epithelioid cells (Log rank, P<0.001), closed loops (Log rank, P=0.002), high mitotic rate (Log rank, P=0.003), and chromosome 3 loss (Log rank, P=0.008).
Conclusions
The value of LTD as a predictor of survival after treatment of posterior uveal melanoma is enhanced by taking histological and cytogenetic factors into account.
Similar content being viewed by others
Main
Uveal melanomas can cause a blind, painful eye, and death from metastasis. Ocular treatment is aimed primarily at preventing or arresting metastatic spread of tumour, preferably conserving the eye with as much useful vision as possible.1 Such treatment includes various forms of radiotherapy, local resection, and phototherapy. In specialist centres, ocular conservation is attempted in approximately 65% of patients and is successful in almost 90% of these.2
Several factors predict metastatic death. Clinical features include the following: largest basal tumour diameter (LTD), tumour height, ciliary body involvement, and extraocular spread.3, 4, 5 Older age and gender are unimportant. Histological factors include the presence of epithelioid cells; extravascular matrix patterns, such as closed loops; and high mitotic rate.6 Genomic factors include partial or total chromosome 3 deletions, and chromosome 8 gains.7, 8, 9
Largest tumour diameter is currently the most widely used predictor of metastatic disease.4, 10, 11, 12, 13, 14 This factor also correlates with extraocular spread and hence chances of orbital recurrence.5, 15 After conservative therapy, LTD is associated with increased risk of local tumour recurrence, exudative retinal detachment, neovascular glaucoma, and other ocular complications.2
The significance of LTD of uveal melanomas requires reappraisal in the light of insights gained from genetic studies.16 There is uncertainty as to whether these tumours become more life-threatening with increasing LTD. Furthermore, there are various explanations for the correlation between LTD and metastatic death. These considerations profoundly influence patient care.
The aims of this study were to reappraise the significance of LTD by correlating this with histological and cytogenetic features, and with survival.
Materials and methods
Patients eligibility
Patients were included in this study if (1) treated for posterior uveal melanoma (ie, tumours involving choroid, including those spreading posteriorly from ciliary body); and if (2) histological data were available. They were excluded if (1) both eyes had melanoma; (2) the patient received primary treatment elsewhere; or (4) histological cell type was not known. In follow-up analyses, patients were excluded if not resident in mainland Britain.
Clinical management
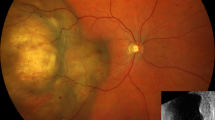
Full ophthalmological examination was performed. LTD and tumour thickness were measured by B-scan echography (I3, Innovative Imaging Inc., Sacramento, CA, USA). The echography was performed by the first author (BD) immediately after indirect ophthalmoscopy, thereby making it easier to define tapering tumour margins. In some patients, tumour biopsy was performed, either to establish the diagnosis or for prognostication.17
Before ocular treatment, systemic clinical examination and biochemical liver function tests were performed routinely, but liver ultrasonography was undertaken only if there was an increased risk of metastatic disease (ie, LTD >16 mm).
Our first choice of treatment was radiotherapy, delivered with a 106-ruthenium plaque or proton beam. Trans-scleral or trans-retinal resection was performed only if the tumour was considered unsuitable for radiotherapy, because of large size or unfavourable location (eg, large bulk increasing risk of exudative retinal detachment and neovascular glaucoma after proton beam radiotherapy; medial location risking canalicular damage and intractable epiphora after proton beam radiotherapy; or extension to within 1.5 mm of optic disc margin, predisposing to optic neuropathy). Enucleation was performed if the patient was not motivated to undergo conservational therapy or if conservational therapy was considered unlikely to succeed. Trans-pupillary thermotherapy was rarely administered as a primary treatment, usually reserved for exudation after radiotherapy.
Histopathological examination
The diagnosis of melanoma was routinely confirmed immunohistochemically using the Melan A, HMB-45, and pancytokeratin stains.18 Melanoma cytomorphology was assessed with haematoxylin and eosin staining and categorized according to the modified Callender system.19 Extravascular matrix patterns were assessed using the PAS reagent, without counterstaining. The mitotic rate was measured by counting the number of mitoses in forty high power fields.
Microsatellite analysis
Our techniques for microsatellite analysis (MSA) have been described previously.20 Briefly, fresh tumour specimens and venous blood samples were collected at the time of surgery. Matched DNA sample pairs from blood and tumour were analysed using the polymerase chain reaction (PCR). The chromosomal order, cytogenetic assignment, and map positions of these microsatellites were obtained by integrating published data from The Genome Database and Ensembl database (www.gdb.org and www.ensembl.org). Allelic imbalance (AI) was scored by comparing the allelic ratios of the normal and tumour specimens, either visually or, if this was not possible, by image analysis. The AI ratio was calculated by dividing the tumour ratio by the normal ratio, with values >1.4 or <0.6 signifying AI.20
Cytogenetic studies
Fluorescence in situ hybridisation (FISH) studies of interphase and metaphase cells were performed on touch preparations and short-term cultures, respectively. FISH was performed in the standard manner, as described previously.8 We used the following probes: centromere enumeration probe (CEP) 3, CEP 8, and locus specific indicator C-myc (ie, on the long arm of chromosome 8) (Vysis Inc., Downers Grove, IL, USA).
MLPA technique
DNA extraction, DNA quality assessment and quantification, and MLPA were performed as previously reported.21 Briefly, genomic DNA was isolated from frozen tumour specimens, and checked for quantity and quality using Nanodrop and multiplex PCR, respectively. Chromosomal imbalances in the tumour samples were identified using the SALSA MLPA kit P027 (MRC-Holland, Amsterdam, The Netherlands), which consisted of 31 probes for loci on chromosomes 1p, 3, 6 and 8, as well as 12 control probes on chromosomes 5, 7, 12, 14, 18, and 21. The MLPA reaction was performed in a G-Storm GS1 Thermal Cycler (Genetic Research Instrumentation Limited, Braintree, Essex, UK). Samples were separated by electrophoresis and analysed by GeneMapper software (Applied Biosystems Ltd, Warrington, Cheshire, UK) in the Molecular Genetics Department of the Liverpool Women's Hospital. Raw data obtained after sequencing were analysed using an Excel spreadsheet-based approach, designed by the National Genetics Reference Laboratory, Manchester, UK. The dosage quotients (DQ) were calculated by dividing the test sample matrix by the control mean matrix. The DQ was categorized as follows: low (<0.65); equivocally low (0.65–0.84); normal (0.85–1.14); equivocally high (1.15–1.34); and high (>1.34).
Statistical analyses
Clinical, pathological, and cytogenetic data were computerised into a customised database prospectively. Tumours were categorised as involving ciliary body if they extended anterior to ora serrata, and were recorded as having epithelioid cells irrespective of the proportion of such cells. Mitotic counts were excluded in patients having enucleation after radiotherapy, because of the effect of this treatment on cell division. Extraocular extension was recorded as being present irrespective of whether this was noted clinically or histopathologically.
We notified the NHS Cancer Registry of all newly diagnosed patients with uveal melanoma. These were then flagged at the Registry, using their NHS number. The Registry informed us automatically and within 2 months of the date and cause of any deaths. If we did not receive such information by the close of the study, we assumed that the patient was alive.
Death from metastatic disease was coded as caused by uveal melanoma unless another primary malignancy was specified as the cause in the death certificate. Follow-up time was estimated from the time of treatment to the date of death or to the 29 December 2008, when the data were downloaded.
Data analysis were carried out using a statistical program (SPSS, SPSS Inc., Chicago, IL, USA). Correlations between categorical baseline risk factors and LTD, which was normal, were analysed using the t-test. Predictive factors were correlated with melanoma mortality using the Cox proportional hazards model. Multivariate analysis was performed as a forward stepwise procedure. The Kaplan–Meier method was used to compute metastatic mortality and groups were compared using the log-rank test. A P-value of less than 0.05 was considered to be statistically significant. All statistical tests were two-sided.
This study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines. Consent for the use of tissues and data for research was obtained from all patients. Ethical committee approval was not required.
Results
The patients comprised 969 (54.6%) males and 807 (45.4%) females with a median age of 60 years (range, 17–97). The tumours had a median LTD of 14.0 mm (range, 4.0–28.0) and a median height of 7.5 mm (range, 0.9–20.0). The LTD showed a normal distribution. The LTD tended to be greater in older patients, with a median of 13.6 mm in patients less than 60-years old and a median of 14.5 mm in older patients. (t-test, P<0.001).
The tumour was located in the right eye in 874 (49.2%) patients and the left eye in 902 (50.8%) patients, with 685 (38.6%) involving ciliary body and 48 (2.7%) extending extraocularly. The primary tumour treatment consisted of enucleation in 973 (54.8%) patients, brachytherapy in 92 (5.2%) patients, proton beam radiotherapy in 107 (6.0%) patients, trans-scleral local resection in 528 (29.7%) patients, and endoresection in 76 (4.3%) patients. The cohort included 64 patients treated by secondary enucleation after radiotherapy. Histology showed epithelioid cells in 1084 (61.0%) tumours, closed loops in 530 (29.8%) tumours, and a high mitotic rate in 470 (27.5%) tumours. Genetic data were available on 800 patients and were based primarily on MSA in 98 patients, FISH in 605 patients, and MLPA in 97 patients, with some patients having more than one test. Chromosome 3 deletions and chromosome 8 gains were found in 358 (45.4%) and 345 (44.4%) of tumours that were tested for these abnormalities, respectively. The presence of epithelioid cells, closed loops, high mitotic rate, chromosome 3 deletion, and chromosome 8 gains all correlated significantly with LTD (t-test, P<0.001).
A total of 1521 patients resided in mainland Britain and they had a median follow-up of 4.9 years (range, 0–36.2). By the close of the study, 643 (42.3%) of these patients had died, the reported cause of death being metastatic disease in 439 (28.9%). In 145 patients with monosomy 3 who had died, the certified cause of death was metastatic disease in 90.3% (95% confidence interval (CI) 85.5–95.2).
With Cox multivariate analysis, metastatic death correlated significantly with largest basal tumour diameter (P<0.001), chromosome 3 loss (P<0.001), closed connective tissue loops (P<0.001), high mitotic rate (P<0.001), and epithelioid cells (P=0.009). There was no significant correlation with sex (P=0.763), ciliary body involvement (P=0.104), tumour height (P=0.264), extraocular spread (P=0.112), or type of treatment (P=0.419).
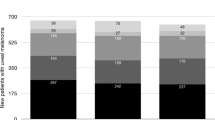
Table 1 lists the prevalences of (a) epithelioid cells; (b) closed loops; (c) high mitotic rate; (d) chromosome 3 loss; (e) chromosome 8 gain; and (f) combined chromosome 3–chromosome 8 abnormalities, for each category of LTD. These risk factors were more prevalent in larger tumours but were nevertheless common in small tumours (Figure 1). For example, chromosome 3 losses were present in 33.3% (95% CI 17.9–48.8) of 39 tumours with LTD <10 mm; 30.5% (95% CI 23.0–37.9) with LTD of 10–12 mm; 39.1% (95% CI 32.7–45.5) with LTD of 13–15 mm; 53.3% (95% CI 47.0–59.7) with LTD of 16–18 mm; and 61.9% (95% CI 53.6–70.3) with LTD >18 mm (Figure 2d).
Survival according to LTD
Figure 2 shows the Kaplan–Meier survival curves of disease-specific mortality. The 20-year melanoma-specific mortality rates were 25.2% (95% CI 10.8–39.7) in patients with an LTD <10 mm; 34.4% (95% CI 27.0–41.8) with LTD of 10–12 mm; 41.4% (95% CI 35.2–47.7) with LTD of 13–15 mm; 68.0% (95% 56.3–79.7) with LTD of 16–18 mm; and 65.4% (95% CI 56.1–74.7) with LTD >18 mm.
Survival according to histological and cytogenetic features
Figure 3 shows the Kaplan–Meier survival curves of metastasis-related mortality in patients with an LTD diameter of 15 mm, according to the presence of (a) epithelioid cells; (b) closed loops; (c) high mitotic rate; and (d) chromosome 3 loss. All these features correlated significantly with mortality (Figure 3).
Discussion
We found that (1) histological and cytogenetic predictors of metastatic death were more prevalent in tumours with greater LTD; (2) many small tumours showed risk factors for metastasis; (3) for each category of LTD, the prevalence of chromosome 3 loss was similar to the 20-year, metastatic mortality; (4) LTD inversely correlated with survival time; and (5) in patients with the same LTD, survival varied greatly according to histological and cytogenetic factors.
To our knowledge, there have not been any recent investigations into the pathological significance of LTD. Kujala et al4 reported long-term outcomes according to LTD without correlating this with histological and cytogenetic factors. The main strengths of our study are the (1) large patient numbers; (2) long follow-up; and (3) genetic tumour typing. The main weakness was the lack of histopathological confirmation of cause of death in all patients, a problem common to most published studies of this type. This did not prevent statistical correlations between survival and LTD. Possible inter-observer variation in assessing melanoma cell type did not prevent statistical correlation with survival. Chromosomal abnormality was investigated using a variety of methods; however, as these were selected according to the year of treatment it is unlikely that any significant bias occurred. Most genetic typing was performed with FISH, which does not detect all lethal chromosome 3 deletions, so that the prevalence of such genetic abnormality was underestimated (perhaps by as much as 10%). Some might question our dependence on the NHS Cancer Registry for survival data but our collaboration with this department for over a decade has provided us with consistent evidence of its reliability.
There is much evidence that uveal melanomas with chromosome 3 deletion are highly lethal, with patients being spared from metastatic disease only if they die of another illness before their metastases can be detected.7, 21 Our study showed that around 90% of deaths in patients with known chromosome 3 status had monosomy 3. Conversely, uveal melanomas without chromosome 3 loss seem to be non-lethal, with so-called ‘fatal disomy 3 melanomas’ proving to have missed chromosome 3 deletions when re-examined using more sensitive techniques.21 If metastatic death occurs exclusively in patients with a monosomy3 melanoma and in all patients with this tumour type, then the prognostic significance of LTD needs to be reappraised. In the absence of any information regarding chromosome 3 status, LTD and other gross physical tumour features indicate in a relatively crude manner: (1) the likelihood of the melanoma proving fatal; and (2) the median survival time should the tumour be lethal.3 If the tumour is of the disomy 3 type, then LTD is largely irrelevant as a prognostic factor, except that together with histological findings it may suggest that the genetic tumour typing is incorrect. For example, a large, high-grade melanoma with epithelioid cells, closed loops, and high mitotic rate is likely to be of the monosomy 3 type, so that a normal result with FISH is probably mistaken. If the tumour is known to have chromosome 3 loss, then LTD gives an indication of the patient's life expectancy, the precision of this estimation being enhanced by the consideration of histological grade of malignancy. In summary, the prognostic significance of LTD is greatly enhanced if the tumour's chromosome 3 status and histological grade of malignancy are known.
The high prevalence of chromosome 3 loss in small tumours has been reported elsewhere.22 This finding suggests that many small choroidal melanomas have metastatic potential. Randomised, prospective studies are needed to determine whether delaying treatment in such cases is harmful, but these investigations will require many patients, long follow-up, and genetic tumour typing. Conversely, more than 30% of choroidal melanomas with an LTD exceeding 18 mm did not show chromosome 3 loss, suggesting that these had little or no metastatic potential. Such non-lethal melanomas undermine investigations on the influence of ocular or systemic treatment on survival. The Collaborative Ocular Melanoma Study (COMS), which performed comparisons of enucleation vs plaque radiotherapy or enucleation with earlier radiotherapy, estimated its study sample sizes assuming that all melanomas had metastatic potential.10, 23 As this was not the case, the COMS patient numbers were insufficient to detect any significant differences.24 Studies on adjuvant systemic chemotherapy in high-risk patients have similar flaws.25 Figure 3 shows the importance of considering histological and cytogenetic predictors when estimating survival probability: the mortality of patients with an LTD of 15 mm varied greatly according to whether histological and cytogenetic risk factors were found. We have developed neural networks predicting survival according to all these factors, also taking age and sex into account.26
The survival time inversely correlated with LTD. With large tumours, metastatic death occurred more quickly. This was because metastases were present for a longer time (lead-time bias); and because of shorter doubling times, suggested by higher mitotic rates in these tumours. LTD correlated with shorter survival also in patients reportedly dying of other causes (Log rank, P=0.01, data not shown). This is probably because (1) older patients tended to have larger tumours; and (2) some deaths from melanoma were wrongly attributed to other causes. Other groups have discussed mistaken cause of death.3 The neural networks we have developed avoid this problem by generating curves of all-cause mortality both of patients with uveal melanoma and of the general population matched for age and sex; by subtracting one curve from the other it is possible to estimate the risk of metastatic death.26
It is assumed by many (but not all authors27, 28) that small uveal melanomas are relatively non-lethal but progressively de-differentiate with time and growth, gradually becoming more aggressive until they eventually metastasise. Zimmerman's hypothesis that enucleation causes fatal tumour dissemination implies a belief that metastasis commences only after uveal melanomas grow large.29 The COMS apparently supported the concept of late metastasis, because its investigation on the influence of pre-enucleation radiotherapy focused on large tumours and because patients with a small melanoma were observed, subsequently being reported as having a good 5-year survival.23, 30, 31
An alternative explanation for the higher prevalence of risk factors in larger tumours is that they grow faster. In countries such as the United Kingdom, middle-aged and elderly individuals tend to have an ocular examination every year or two, but a significant proportion of melanomas are missed at any single examination.32 When such failure occurs, then slow-growing, low-grade melanomas will probably still be small if they are detected 1 or 2 years later, whereas high-grade melanomas will grow larger.
The conventional interpretation of Kaplan–Meier survival curves after treatment of choroidal melanoma is that survival is better with smaller tumours because of earlier treatment. An alternative view is that survival is better with smaller tumours because fewer small tumours are fatal. Our data show that both the prevalence of chromosome 3 loss and the disease-specific mortality increased from around 25–33% when the LTD was <10 mm to approximately 62–65% when the LTD exceeded 18 mm. These survival curves are only approximate because of competing risks and because of misdiagnosed cause of death. Nevertheless, they are consistent with the hypothesis that, irrespective of size, all melanomas with chromosome 3 loss are eventually fatal, unless the patient dies of an unrelated cause before metastatic disease develops. These data provide further evidence that ocular treatment rarely, if ever, prevents the onset of metastatic spread, because such dissemination commences years before the uveal melanoma is detected and treated.28 It is not known whether or not ocular treatment prolongs life once metastatic spread has commenced, by arresting tumour dissemination and reducing the metastatic burden. To address this question one would need randomised, prospective studies on immediate vs delayed treatment, taking LTD and genetic tumour type into account. Statistical correlations between LTD and metastasis have led to the general impression that large uveal melanomas are more life threatening (ie, lethal). In contrast, the prevalence data in this study suggest an alternative scenario, which is that more large tumours are lethal. In other words, our data lend further support to the hypothesis that uveal melanomas grow large because they are aggressive and do not become aggressive because they grow large. Treatment rationale is profoundly influenced by whether it is believed that metastasis commences before uveal melanomas grow large or afterwards. The importance of evidence-based care is now accepted; however, we need to be conscious of how the same evidence can be interpreted in different ways.33
As early as the mid-nineteenth century, von Graefe34 observed that some patients with a small uveal melanoma died of metastasis, whereas others with a large tumour survived. We now know that this is because there are lethal and non-lethal subtypes of uveal melanoma. What this means is that the value of LTD as a survival predictor is enhanced when considered together with histological and genetic risk factors.

Conflict of interest
The authors declare no conflict of interest.
References
Damato B . Treatment of primary intraocular melanoma. Expert Rev Anticancer Ther 2006; 6: 493–506.
Damato B, Lecuona K . Conservation of eyes with choroidal melanoma by a multimodality approach to treatment: an audit of 1632 patients. Ophthalmology 2004; 111: 977–983.
Kujala E, Kivelä T . Tumor, node, metastasis classification of malignant ciliary body and choroidal melanoma evaluation of the 6th edition and future directions. Ophthalmology 2005; 112: 1135–1144.
Kujalá E, Mäkitie T, Kivelä T . Very long-term prognosis of patients with malignant uveal melanoma. Invest Ophthalmol Vis Sci 2003; 44: 4651–4659.
Coupland SE, Campbell I, Damato B . Routes of extraocular extension of uveal melanoma: risk factors and influence on survival probability. Ophthalmology 2008; 115: 1778–1785.
Folberg R, Pe’er J, Gruman LM, Woolson RF, Jeng G, Montague PR et al. The morphologic characteristics of tumor blood vessels as a marker of tumor progression in primary human uveal melanoma: a matched case-control study. Hum Pathol 1992; 23: 1298–1305.
Prescher G, Bornfeld N, Horsthemke B, Becher R . Chromosomal aberrations defining uveal melanoma of poor prognosis. Lancet 1992; 339: 691–692.
Damato B, Duke C, Coupland SE, Hiscott P, Smith PA, Campbell I et al. Cytogenetics of uveal melanoma: a 7-year clinical experience. Ophthalmology 2007; 114: 1925–1931.
White VA, Chambers JD, Courtright PD, Chang WY, Horsman DE . Correlation of cytogenetic abnormalities with the outcome of patients with uveal melanoma. Cancer 1998; 83: 354–359.
The COMS randomized trial of iodine 125 brachytherapy for choroidal melanoma: V. Twelve-year mortality rates and prognostic factors: COMS report No. 28. Arch Ophthalmol 2006; 124: 1684–1693.
De Potter P, Shields CL, Shields JA, Cater JR, Brady LW . Plaque radiotherapy for juxtapapillary choroidal melanoma. Visual acuity and survival outcome. Arch Ophthalmol 1996; 114: 1357–1365.
Diener-West M, Reynolds SM, Agugliaro DJ, Caldwell R, Cumming K, Earle JD et al. Development of metastatic disease after enrollment in the COMS trials for treatment of choroidal melanoma: Collaborative Ocular Melanoma Study Group Report No. 26. Arch Ophthalmol 2005; 123: 1639–1643.
Shammas HF, Blodi FC . Prognostic factors in choroidal and ciliary body melanomas. Arch Ophthalmol 1977; 95: 63–69.
Isager P, Ehlers N, Overgaard J . Prognostic factors for survival after enucleation for choroidal and ciliary body melanomas. Acta Ophthalmol Scand 2004; 82: 517–525.
Affeldt JC, Minckler DS, Azen SP, Yeh L . Prognosis in uveal melanoma with extraocular extension. Arch Ophthalmol 1980; 98: 1975–1979.
Damato B, Taktak A . Uveal malignant melanoma: mortality In: Singh AD, Damato B, Pe’er J (eds). Clinical Ophthalmic Oncology. Philadelphia: Saunders, Elsevier, 2007; pp 277–282.
Sen J, Groenewald C, Hiscott PS, Smith PA, Damato BE . Transretinal choroidal tumor biopsy with a 25-gauge vitrector. Ophthalmology 2006; 113: 1028–1031.
Font RL, Croxatto JO, Rao NA In: Tumors of the eye and ocular adnexa AFIP Fasc 4/5. Series 4 (ed). Washington: ARP Press, 2006. pp 56–59.
McLean IW, Foster WD, Zimmerman LE, Gamel JW . Modifications of Callender's classification of uveal melanoma at the Armed Forces Institute of Pathology. Am J Ophthalmol 1983; 96: 502–509.
Scholes AG, Liloglou T, Maloney P, Hagan S, Nunn J, Hiscott P et al. Loss of heterozygosity on chromosomes 3, 9, 13, and 17, including the retinoblastoma locus, in uveal melanoma. Invest Ophthalmol Vis Sci 2001; 42: 2472–2477.
Damato B, Dopierala J, Klaasen A, van Dijk M, Sibbring J, Coupland SE . Multiplex ligation-dependent probe amplification of uveal melanoma: correlation with metastatic death. Invest Ophthalmol Vis Sci 2009; 50: 3048–3055.
Shields CL, Ganguly A, Materin MA, Teixeira L, Mashayekhi A, Swanson LA et al. Chromosome 3 analysis of uveal melanoma using fine-needle aspiration biopsy at the time of plaque radiotherapy in 140 consecutive cases: the Deborah Iverson, MD, Lectureship. Arch Ophthalmol 2007; 125: 1017–1024.
Hawkins BS . The Collaborative Ocular Melanoma Study (COMS) randomized trial of pre-enucleation radiation of large choroidal melanoma: IV. Ten-year mortality findings and prognostic factors. COMS report number 24. Am J Ophthalmol 2004; 138: 936–951.
Damato B . Legacy of the collaborative ocular melanoma study. Arch Ophthalmol 2007; 125: 966–968.
Voelter V, Schalenbourg A, Pampallona S, Peters S, Halkic N, Denys A et al. Adjuvant intra-arterial hepatic fotemustine for high-risk uveal melanoma patients. Melanoma Res 2008; 18: 220–224.
Damato B, Eleuteri A, Fisher AC, Coupland SE, Taktak AF . Artificial neural networks estimating survival probability after treatment of choroidal melanoma. Ophthalmology 2008; 115 (9): 1598–1607.
Shields JA . Treating some small melanocytic choroidal lesions without waiting for growth. Arch Ophthalmol 2006; 124: 1344–1346.
Eskelin S, Phrönen S, Summanen P, Hahka-Kemppinen M, Kivelä T . Tumor doubling times in metastatic malignant melanoma of the uvea: tumor progression before and after treatment. Ophthalmology 2000; 107: 1443–1449.
Zimmerman LE, McLean IW, Foster WD . Does enucleation of the eye containing a malignant melanoma prevent or accelerate the dissemination of tumour cells. Br J Ophthalmol 1978; 62: 420–425.
Collaborative Ocular Melanoma Study Group. Mortality in patients with small choroidal melanoma. COMS report no. 4. The Collaborative Ocular Melanoma Study Group. Arch Ophthalmol 1997; 115: 886–893.
Melia BM, Diener-West M, Bennett SR, Folk JC . Factors predictive of growth and treatment of small choroidal melanoma. Arch Ophthalmol 1997; 115: 1537–1544.
Damato B . Detection of uveal melanoma by optometrists in the United Kingdom. Ophthal Physiol Opt 2001; 21: 268–271.
Damato B . Choroidal melanoma endoresection, dandelions and allegory-based medicine. Br J Ophthalmol 2008; 92: 1013–1014.
von Graefe A . Züsatze über intraocular Tumoren. Archiv für Ophthalmologie 1868; 14: 103–144.
Acknowledgements
We are grateful to Mr Gary Cheetham for database management and staff at the Liverpool Women's Hospital for cytogenetic testing.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Damato, B., Coupland, S. A reappraisal of the significance of largest basal diameter of posterior uveal melanoma. Eye 23, 2152–2162 (2009). https://doi.org/10.1038/eye.2009.235
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.235
Keywords
This article is cited by
-
SLC25A38 as a novel biomarker for metastasis and clinical outcome in uveal melanoma
Cell Death & Disease (2022)
-
No differences in the long-term prognosis of iris and choroidal melanomas when adjusting for tumor thickness and diameter
BMC Cancer (2021)
-
Uveal Melanoma: A Review of Prognostic Factors for Metastases
Current Ophthalmology Reports (2021)
-
Comparison of Germline versus Somatic BAP1 Mutations for Risk of Metastasis in Uveal Melanoma
BMC Cancer (2018)
-
Association between traditional clinical high-risk features and gene expression profile classification in uveal melanoma
Graefe's Archive for Clinical and Experimental Ophthalmology (2018)